Secondary Amenorrhea - Pediatric Residency Program
advertisement
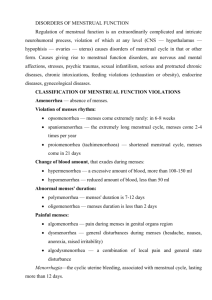
DYSMENORRHEA, DUB, AND AMENORRHEA AUGUST 2014 Pediatric Continuity Clinic Curriculum Created by: M.Srikanthan OBJECTIVES Review the classification and management dysmenorrhea Review the differential diagnosis and workup for amenorrhea Determine which patients warrant a pelvic exam and OB/GYN referral REGULAR MENSTRUAL CYCLE Follicular phase (estrogen) Ovulation Luteal Phase (progesterone) Puberty Thelarche (Tanner 2 breast development) Pubarche (Tanner 2 pubic hair) Menarche ©2002 by American Academy of Pediatrics CASE #1 A 15½-year-old girl came to the office with complaints of the recent onset of painful menstrual periods. Menarche occurred at the age of 13 years and except for an occasional mildly uncomfortable menstrual period, she has not experienced significant pain until recently. She described additional symptoms that also had not been present previously, including headache, loose stools, and breast tenderness. She has tried several over-the-counter medications, including acetaminophen, without significant relief. She has missed 3 days of school in the last 6 weeks because of these complaints. What are the differences between primary and secondary dysmenorrhea and the differential diagnosis for each? How would you manage this patient? PRIMARY VS. SECONDARY DYSMENORRHEA Primary Dysmenorrhea: pain associated in the absence of pelvic disease Associated with headache, nausea, diarrhea Due to Prostoglandin E2 and F2a secretion resulting in increased uterine contractility and upregulation of pain receptors Secondary Dysmenorrhea: Due to pathologic process Congenital partial outflow obstruction Endometriosis PID Pregnancy complication RED FLAGS: persistent pain after 3-6 months of OCP use (risk for endometriosis), pelvic pain/bleeding occurring midcycle, pain with vaginal discharge (concern for PID) The physiologic basis :cell membrane phospholipids, endomyometrial prostaglandins, and leukotrienes. After ovulation, in response to the production of progesterone, fatty acids build up in cell membrane phospholipids. Arachidonic acid and other omega-7 fatty acids are released and initiate a cascade of prostaglandins and leukotrienes in the uterus Low back pain occurring in association with dysmenorrhea is due to referred pain from spinal nerves. Bloating may result from sensitivity to progesterone, a smooth muscle relaxant, produced in the second half of the cycle. Subsequent loose stools are a PG-mediated symptom. Migraine or other headaches may be triggered by declining levels of estrogen in the immediate premenstrual phase of the cycle The pathologic mechanisms of pain associated with such causes of secondary dysmenorrhea as uterine fibroids, endometriosis, adenomyosis, and other pelvic pathologies may be somewhat more specific to the pathologic entity. MANAGEMENT Primary Dysmenorrhea NSAIDs (inhibit PG synthesis)-starting 1 day before onset on menses ,continue on day 1 and if needed on day 2. OCPs (eliminate ovulation and thin out endometrial lining) Secondary Dysmenorrhea If initial therapy is ineffective, consider bimanual exam to evaluate for cul-de-sac tenderness Consider OB/GYN referral if patient continues to have significant pain despite 3-6 months of OCP use for evaluation of endometriosis,fibroids Primary dysmenorrhea may result in significant school absence and lost productivity, so aggressive and evidence-based treatment is warranted. If appropriate doses of NSAIDs do not control symptoms after two to three cycles, a trial of OCPs may be indicated. OCPs reduce menstrual pain by eliminating ovulation and by thinning the endometrial lining; when ovulation does not occur and the endometrial lining is thinner, the synthesis of prostaglandins is reduced. 30- or 35-mcg ethinyl estradiol-containing pill may be preferable to a 20-mcg formulation. For adolescents whose external genitalia are normal and who have classic symptoms of dysmenorrhea, a pelvic examination is not required initially. If initial therapy is ineffective, a bimanual examination can be helpful; endometriosis can be associated with mild posterior uterine/cul-de-sac tenderness. The cul-de-sac (pouch of Douglas) posterior to the uterus is the most dependent portion of the pelvis and, thus, the most likely site for pelvic endometriosis. CASE #2 You are seeing a 16-year-old girl because she has not had a menstrual period in 6 months. She had menarche at 12 years of age and her periods had become progressively more irregular before completely stopping 6 months ago. Her past medical history is unremarkable and she is currently asymptomatic. Discuss the differential diagnosis for primary vs secondary amenhorrhea How would you work up this patient? DEFINITION: Primary Amenhorrhea: Lack of menses by the age of 15 years or by more than 3 years after the onset of secondary sexual development. Lack of any secondary sexual characteristics by age 13 years also is abnormal and should be investigated. Secondary Amenorrhea: 3 consecutive months of amenorrhea after the achievement of menarche or absence of 3 cycles in 6 months. DIFFERENTIAL OF AMENORRHEA List: Central: Ovarian: Anatomical-outflow tract Others: DIFFERENTIAL DIAGNOSIS FOR PRIMARY VS SECONDARY AMENORRHEA EVALUATION OF AMENORRHEA CASE #3 A 14-year-old girl is being evaluated for vaginal bleeding. Her menarche was about 18 months ago, and her periods have occurred at 5- to 6-week intervals; the flow is variable and she has had no dysmenorrhea. The current menstrual period has been heavier and she had cramps at the start. She remembers passing a few clots about 2 cm in size. She denies sexual activity. On physical examination, she is not pale, her heart rate is 68 beats/min, and her body mass index is 24. She is at sexual maturity rating 5 for pubertal development. She has vague tenderness diffusely in her lower abdomen with no guarding or rebound. A rapid pregnancy test result is negative, and her hemoglobin level is 12.6 g/dL (126 g/L). Of the following, the MOST likely explanation for the girl’s symptoms is A. a bleeding disorder B. dysfunctional uterine bleeding C. ectopic pregnancy D. hypothyroidism E. pelvic inflammatory disease CASE #3 A 14-year-old girl is being evaluated for vaginal bleeding. Her menarche was about 18 months ago, and her periods have occurred at 5- to 6-week intervals; the flow is variable and she has had no dysmenorrhea. The current menstrual period has been heavier and she had cramps at the start. She remembers passing a few clots about 2 cm in size. She denies sexual activity. On physical examination, she is not pale, her heart rate is 68 beats/min, and her body mass index is 24. She is at sexual maturity rating 5 for pubertal development. She has vague tenderness diffusely in her lower abdomen with no guarding or rebound. A rapid pregnancy test result is negative, and her hemoglobin level is 12.6 g/dL (126 g/L). Of the following, the MOST likely explanation for the girl’s symptoms is A. a bleeding disorder B. dysfunctional uterine bleeding C. ectopic pregnancy D. hypothyroidism E. pelvic inflammatory disease B. Painless, irregular, or prolonged bleeding of endometrial origin without any accompanying structural disease is referred to as dysfunctional uterine bleeding (DUB) physiologic anovulation seen in early puberty with immaturity of the hypothalamic-pituitary axis. Pt is within 2 years of menarche, when anovulatory bleeding is common. menstrual interval is at the upper limit of normal, and the fact that she has had no prior pain is suggestive of DUB. On average, ovulatory cycles start at 20 months after menarche, and her history of new onset of cramping suggests that her periods are now becoming ovulatory. CAUSES Local:. vulva, vagina, cervix, uterus, or ovaries and may be the result of trauma, foreign bodies, infections, pregnancy-related, and rarely, estrogen-producing ovarian tumors. Systemic: bleeding disorders and thyroid disease. Hypothyroidism -irregular or prolonged bleeding, hyperthyroidism -amenorrhea. Negative sexual activity, pregnancy test is negative,PID or ectopic very unlikely DYSFUNCTIONAL UTERINE BLEEDING/ABNORMAL UTERINE BLEEDING DUB is abnormal bleeding not resulting from uterine disease, medications, systemic illness, or pregnancy. DUB is considered a diagnosis of exclusion. Disorders affecting the hypothalamic-pituitary-ovarian axis can mimic DUB DUB/AUB DIFFERENTIAL DIAGNOSIS PHYSICAL EXAM PELVIC EXAM? Important for confirming normal anatomy, isolating source of pain, ruling outlesions/masses, and identifying sources of vaginal/uterine bleeding DUB WORKUP *Pregnancy Test* CBC/with reticulocyte count TSH Coagulation Studies to r/o Von willebrand disease Screening for Gonorrhea and chlamydia-causes friability of uterine endometrium and cervixthereby increased bleeding DUB MANAGEMENT Iron Supplementation Goal of medical therapy is to stop bleeding Nonsteroidal anti-inflammatory drugs such as ibuprofen and naproxen sodium can help reduce blood loss combination oral contraceptive (COC) containing estrogen, which promotes clotting and causes endometrial proliferation, and progestin, which stabilizes the endometrial lining WHEN TO REFER… PREP QUESTION A 16-year-old girl reports a history of irregular menses. Her periods have become progressively less frequent since menarche at 12 years of age. Her last menstrual period was 4 months ago. She is not sexually active and has had no galactorrhea. She is taking collegelevel classes in school, preparing for her college-entrance exams, and helping care for her sick mother. On physical examination, her vital signs are normal and her body mass index is 31. There are inflammatory acne lesions on her face and back, hyperpigmented velvety-appearing skin at the nape of her neck, and increased body hair. Her thyroid gland is not enlarged, and the diameter of her clitoris is 4 mm. Of the following, the condition MOST likely responsible for this girl’s symptoms and signs is A. dysfunctional uterine bleeding B. emotional stress C. hypothyroidism D. pituitary adenoma E. polycystic ovary syndrome . E. The presence of acanthosis nigricans combined with obesity (body mass index >30 kg/m2),acne, and some increase in body hair described for the girl in the vignette as well as irregular menses 3 years after menarche suggests the need for further evaluation for polycystic ovariansyndrome (PCOS). Diagnosis of PCOS, using the 2003 Rotterdam criteria, requires, in addition to exclusion of related conditions, the presence of two of the following three criteria: 1)oligo- or anovulation, 2) clinical or biochemical signs of hyperandrogenism, and 3) polycystic ovaries. Oligo- or anovulation presents as irregular menses, and hyperandrogenism may present as acne, increased body hair, and rarely, clitorimegaly (a transverse clitoral diameter greater than 3 mm). PREP QUESTION You are seeing a 16-year-old girl because she has not had a menstrual period in 6 months. She had menarche at 12 years of age and her periods had become progressively more irregular before completely stopping 6 months ago. Her past medical history is unremarkable and she is currently asymptomatic. She is on the cross country running team and is planning on running a marathon in the next year. She denies being sexually active or having any body image issues. Her vital signs are normal, her body mass index is 19.5, and her sexual maturity rating is stage 5. Results of the remainder of her physical examination are unremarkable. The pregnancy test result is negative. Additional tests, including a complete blood cell count, electrolytes, thyroxine, thyroid-stimulating hormone, luteinizing hormone, and follicle-stimulating hormone concentrations, yield normal results. Of the following, the MOST important next step in the management of this girl would be to have A. begin combined oral contraception B. increase her calcium and vitamin D intake C. increase her overall nutritional intake D. stop exercising till her menses returns E. switch to a nonendurance sport C negative energy balance in female athletes may lead to the female athlete triad amenorrhea, osteoporosis, and disordered eating. at risk for osteoporosis because of low BMI and estrogen deficiency. The return of menses signals an improvement in the hormonal status that, in turn, will increase the bone mineral density (BMD). a combined oral contraceptive is not as effective as increasing energy intake to improve BMD. Calcium, vitamin D, and weight-bearing exercise are needed to achieve peak bone mass in all adolescents, but requirements do not change with athletic participation, and supplements will not influence the menstrual status. Changing the type of sport or stopping exercising will reduce the energy output and help achieve energy balance, but the initial approach should be to increase energy intake. If the girl is unable or unwilling to increase energy intake, exercise restrictions may be required. REFERENCES AND FUTURE READING Consultation with a Specialist: Dysmenorrhea. Pediatrics in Review Vol. 27 No. 2 February 1, 2006. pp. 64 -71. Menstrual Disorders. Pediatrics in Review Vol. 28 No. 5 May 1, 2007. pp. 175 -182 Dysfunctional Uterine Bleeding. Pediatrics in Review Vol. 23 No. 7 July 1, 2002 pp. 227 -233 Secondary Amenorrhea. Pediatrics in Review Vol. 27 No. 3 March 1, 2006 pp. 113 -114 Gynecologic Examination for Adolescents in the Pediatric Office Setting. Pediatrics Vol. 126 No. 3 September 1, 2010 . pp. 583 -590 Nelson Textbook of Pediatrics : Expert Consult (19th Edition). Kliegman, Robert M. Stanton, Bonita St. Geme, Joseph thank you