Abnormal Uterine Bleeding: Not just OCPs and hysterectomies
advertisement

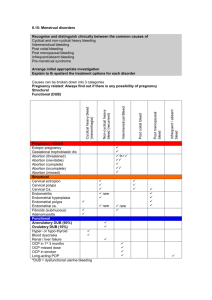
Abnormal Uterine Bleeding: Not just OCPs or hysterectomy anymore Tony Ogburn MD Professor, Dept. of Ob/Gyn University of New Mexico Objectives • Discuss the classification of abnormal uterine bleeding • Understand the evaluation of abnormal uterine bleeding in reproductive aged women • List the non surgical treatment options of abnormal uterine bleeding • Discuss the indications for surgical management for abnormal uterine bleeding Disclosures • Nexplanon trainer – no disclosure • IUD devotee… A lot of confusing terms! Dysfunctional uterine bleeding Epimenorrhagia Epimenorrhea Functional uterine bleeding Hypermenorrhea Hypomenorrhea Menometrorrhagia Menorrhagia (all usages: essential menorrhagia, idiopathic menorrhagia, primary menorrhagia, functional menorrhagia, ovulatory menorrhagia, anovulatory menorrhagia) Metrorrhagia Metropathica hemorrhagica Oligomenorrhea Polymenorrhagia Polymenorrhea Uterine hemorrhage Common Terminology Descriptive Term Menorrhagia Metrorrhagia Menometorrhagia Hypermenorrhea Polymenorrhea Oligomenorrhea Amenorrhea Bleeding pattern Regular cycles, prolonged duration, excessive flow Irregular cycles Irregular, prolonged, excessive Regular, normal duration, excessive flow Frequent cycles Infrequent cycles No cycles A new classification system PALM - COEIN • Initial conference – 2005 – Wide participation of stakeholders • FIGO, ACOG, FDA, Researchers, Journals • Focused on terminology, defining needs and resources • Follow-up conference – 2009 • Nomenclature and classification systems – Approved by FIGO - 2011 • Useful for clincians, researchers, and educators • Provides a tool for structured history, evaluation Nomenclature • Acute AUB – “an episode of bleeding in a woman of reproductive age, who is not pregnant, that, in the opinion of the provider, is of sufficient quantity to require immediate intervention to prevent further blood loss.” • Chronic AUB – “bleeding from the uterine corpus that is abnormal in duration, volume, and/or frequency and has been present for the majority of the last 6 months.” Suggested “norms” Clinical dimensions of menstruation and menstrual cycle Frequency of menses, d Descriptive term Normal limits (5th-95th percentiles) Frequent <24 Normal 24-38 Infrequent Regularity of menses: cycleto-cycle variation over 12 months, d Duration of flow, d Volume of monthly blood loss, mL >38 Absent No bleeding Regular Variation ± 2-20 Irregular Variation >20 Prolonged >8.0 Normal 4.5-8.0 Shortened <4.5 Heavy >80 Normal 5-80 Light <5 PALM-COEIN • 4 categories that are defined by visually objective structural criteria (PALM) – – – – Polyp Adenomyosis Leiomyoma Malignancy and hyperplasia • 4 criteria that are unrelated to structural anomalies (COEI) – – – – Coagulopathy Ovulatory dysfunction Endometrial Iatrogenic • 1 criterion that is reserved for entities that are not yet classified (N). Causes of AUB Structural abnormalities (PALM) • Polyps – AUB-P – endocervical or endometrial • Detected by ultrasound or sonohysterography • Often irregular, light bleeding Structural abnormalities (PALM) • Adenomyosis –AUB-A • Controversial as a cause of bleeding • Diagnosed with ultrasound, MRI, pathology Structural abnormalities (PALM) • Leiomyoma – AUB-L – Submucous – Intramural – Subserosal • Diagnosed with exam, ultrasound, MRI, CT • Heavy, regular bleeding Structural abnormalities (PALM) • Malignancy and hyperplasia – AUB-M • Diagnosed by biopsy • Irregular bleeding Non Structural Causes - COEI • Coagulopathy • Usually suspected based on history • Von Willebrands most common • Heavy, regular bleeding • Ovulation disorders • Suspected on history – Variable cycle length • Can be confirmed with laboratory testing • Wide range of bleeding patterns – usually irregular Causes of AUB • Anovulatory – Most common cause of AUB – Many reasons for anovulation • Unknown • PCOS • Stress, weight change, exercise • Endocrine – Thyroid, PRL – Secreting tumors Non Structural Causes - COEI • Endometrial • A diagnosis of exclusion – A wastebasket… • Iatrogenic – Hormone Use – IUD, implant Not Yet Classified - N • “Other entities that may or may not contribute to or cause AUB but have not been identified or have been poorly defined, inadequately examined, and/or are extremely rare” Evaluation • History – Acute • Stable? – Chronic – Characterize bleeding pattern • Examination – Is it from the uterus?! • Laboratory studies – Pregnancy test – Hct/CBC – Other labs only if indicated – e.g. • TSH/PRL • Iron studies • Labs for disorders of hemostasis Evaluation • Other diagnostic procedures – EMB • Consider in all patients over 45 or refractory bleeding • Pipelle vs. D&C – Ultrasound – Sonohysterogram – Hysteroscopy Endometrial biopsy Ultrasound - Abdominal or transvaginal - Inexpensive and readily available in most of the world Sonohysterogram – Inject small amount of fluid in uterine cavity – Transvaginal ultrasound – Endometrial thickness and evaluation of intrauterine structures Hysteroscopy Expensive Can be used for treatment MRI • Very expensive • Not readily available • Rarely needed! Treatment • Acute or chronic? • If you find something in your evaluation – Treat it! – Thyroid disease, cervical polyp, pregnancy, etc. • Structural – consider referral early on – Surgery, embolization, hormonal Rx • Often left with no obvious cause – Now what? Treatment - Acute • Unstable? – High dose hormones vs D&C • IV estrogen – 25 mg IV q 4-6 hours • Stable – Oral meds • Monophasic OCPs – One TID for seven days, then daily for at least one cycle • Medroxyprogesterone (Provera) – 20 mg TID for seven days, then daily for at least three weeks • Tranexamic acid (Lysteda) – 1.3 mg TID for five days Treatment - Chronic Considerations • Etiology and severity of bleeding (eg, anemia, interference with daily activities) • Associated symptoms (eg, pelvic pain, infertility) • Contraceptive needs or plans for future pregnancy • Contraindications to hormonal or other medications • Medical comorbidities • Patient preferences regarding medical versus surgical and short-term versus long-term therapy Treatment Options • Non-surgical – usually the first line of treatment – Expectant management – NSAIDs • Reduce blood loss by ~50% – Antifibrinolytic agents - Tranexemic acid (Lysteda) • Expensive – Hormonal methods • Combination methods – Reduce blood loss by ~50% – Regulate cycles in ~85% • Levonorgestrel IUD – Reduce blood loss by ~85% – Less effective at regulating cycles but usually not an issue • Cyclic progestin – Most appropriate for anovulatory bleeding if other methods contraindicated • GnRH agonists (leuprolide) – Expensive for long term use but good for pre-procedure preparation Levonorgestrel IUD • FDA approved for treatment of abnormal bleeding – More effective than OCPs, oral progestins, DepoProvera, NSAIDs • Cost effective • Few side effects • Reduces blood loss by up to 97% • Takes 3-6 months for optimal effect Combination Methods • OCPs – Use monophasic at least for first three months – Use 30-35 of estrogen – Continuous vs. cyclic • Patch/Rings – No good trials about efficacy for this indication Other? • Depo Provera • Implant Surgical Treatment • Two main approaches – Global endometrial ablation – Hysterectomy • Future pregnancy contraindicated/impossible Global Endometrial Ablation • Outpatient procedure • Excellent safety profile • A variety of methods – – – – Balloon – Thermachoice Radiofrequency electricity – Novasure Freezing – Her Option Circulating hot water – HTA • Unclear which, if any, is best! – All have about 80% “success” – Less in younger patients… – Equal to IUD in efficacy Thermachoice • Eight minute cycle • Lots of cramping during procedure HTA - 10 minute cycle - Vaginal burns an early issue Her Option - Takes a long time… Novasure - 1-2 minutes Have to dilate cervix more We have it at CRH!!! Hysterectomy • Random facts… – 100% effective for AUB – A significant minority of women with “conservative” management end up with a hyst eventually – Satisfaction rates are very high – Major complications do happen – Expensive Questions ? Maria • 32 yo G2P2 with post – coital spotting for several months • History completely unremarkable Cora • 37 yo with longstanding history of regular, heavy menses now bleeding heavily for 16 days. Passed out at home and brought in by ambulance. Erica • 62 yo postmenopausal for 11 years with spotting for several months Stephanie • 24 yo G0 with very heavy menses and cramping increasing over one year Jane • 42 yo G3P3 presents with heavy, regular bleeding for 9-12 months. • Bleeds 2-3 weeks each month with large clots and cramps. Sara • 46 yo G2P2 with heavy, irregular menses for two years. Now increasing in frequency and flow • Previous C/S X 2