abnormal bleeding in the childbearing years
advertisement

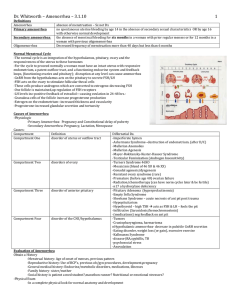
“Approved” on the meeting of methodical board Department of Obstetrics and Gynaecology with the Course of Infantile and Juvenile Gynaecology dated “__”_________ 20__, minutes № __ Deputy Chief, DMS ___________ professor O.A.Andriiets Methodological Instructions №6 to organize independent student’s work on the topic: “Abnormalities in menstrual function in girls” Subject: Infantile and Juvenile Gynaecology Year: VI Faculty: Medical Number of hours: 2 Methodical instructions compiled by: assistant lecturer Rak L.M. I. Topic: Abnormalities in menstrual function in girls II. Class duration – 4 hours. III. Educational objectives: The student must know: 1. Classification of abnormalities in menstrual cycle. 2. Pathogenesis of abnormalities of menstrual cycle. 3. Indications to physiotherapeutic and sanatoria and health methods of treatment of this pathology. 4. Justify symptomatic and pathogenetic treatment of different kinds of abnormalities of menstrual cycle. 5. Justify indications to surgical methods of treatment. The student must be able to: Make a scheme of non-hormonal, hormonal hemostasis in abnormalities of menstrual cycle in juvenile. Prescribe medicine. IV. Advice to the student. Functional components of menstruation hypothalamus, pituitary, ovary, outflow tract, feedback mechanism Primary amenorrhea is defined as the absence of menses by 16 years of age in the presence of normal secondary sexual characteristics, or by 14 years of age when there is no visible secondary sexual characteristic development. Secondary amenorrhea - absence of menses for 6 months in a previously menstruating female Amenorrhea 1. Genuine & false 2. Primary & secondary 3. Physiological & pathological 4. The hypothalamic amenorrhea, The pituitary amenorrhea, The ovarian amenorrhea, The uterine form of amenorrhea. The hypothalamic amenorrhea Psychogenic amenorrhea Amenorrhea during falls pregnancy Amenorrhea as a symptom of nervous anorexia Amenorrhea as a symptom of adiposogenital dystrophy Amenorrhea as a symptom of the Lorence-Moon-Barde-Bidle syndrome Amenorrhea as a symptom of the Morghani_Stuart syndrome Amenorrhea as a symptom of the persistent lactation syndrome (the KiariFromel syndrome) Psychogenic amenorrhea Appears as a result of stress situation or psychic traumas Excessive production of corticotropin within stress blocs production of releasing hormones by Hypotalamus. Treatment: – psychotherapy, – sedative remedies, – physiotherapy. – After 2-3 months of treatment without result we prescribe thyroidin. Amenorrhea during falls pregnancy Appears in women, who are eager or very afraid to become pregnant. Clinical features: – Nausea – Morning vomiting – Swelling of breast – Some enlarging & softening of uterus can appear But all test for pregnancy are negative. Anorexia Nervosa Onset between ages 10 and 30. Weight loss of 25% or weight 15% below normal for age and height. Special attitudes: —Denial, —Distorted body image, —Unusual hoarding or handling of food. At least one of the following: —Lanugo, —Bradycardia, —Overactivity, —Episodes of overeating (bulimia), —Vomiting, which may be self-induced Amenorrhea. No known medical illness. No other psychiatric disorder. Other characteristics: —Constipation, —Low blood pressure, —Hypercarotenemia, —Diabetes insipidus. Anorexia Nervosa Cessation of menstrual cycle via endurance activities, inadequate body weight, eating disorder, stress Reestablish normal hormone levels via diet and exercise counseling, hormone therapy Amenorrhea as a symptom of adiposogenital dystrophy It is usually associated with tumours of the hypothalamus, causing increased appetite and depressed secretion of gonadotropin. It seems to affect males mostly. Is a condition characterized by Feminine obesity Growth retardation and retarded sexual development, atrophy or hypoplasia of the gonads, and altered secondary sex characteristics, headaches mental retardation, problems with vision polyuria, polydipsia. tumours of the hypothalamus Amenorrhea as a symptom of the Laurence-Moon-Barde-Bidle syndrome Laurence-Moon syndrome comprises Onset in childhood. Inheritance is autosomal recessive. retinitis pigmentosa, initially, problem of night vision; then central vision and then peripheral vision loss progressing to blindness. mental retardation, stunted stature hypogonadism. Spinocerebellar ataxia and progressive spastic paraplegia The complete syndrome is seldom observed in the same individual, but the features are often scattered among the siblings of one family or generation. Members of these families have an increased number of miscarriages and early deaths. Amenorrhea as a symptom of the Morghani-Stuart syndrome The main features of this hereditary syndrome are: 1) hyperostosis frontalis interna, 2) adipositas, 3) virilism and hirsutism 4) menstrual disorders Treatment is symptomatic Hyperprolactinemia has such causes: prolactin-secreting pituitary adenomas -other pituitary or hypothalamic tumors that may distort the portal circulation and thereby prevent effective delivery of hypothalamic dopamine (the putative prolactin inhibitory factor or hormone) -a variety of drugs that lower dopamine levels or inhibit dopamine action (amphetamines, benzodiazepines, butyrophenones, metoclopramide, methyldopa, opiates, phenothiazines, reserpine, and tricyclic antidepressants) -breast or chest wall surgery, cervical spine lesions, or herpes zoster (activation of the afferent sensory neural pathway that stimulates prolactin secretion, in a manner similar to suckling) -hypothyroidism (increased hypothalamic thyrotropin-releasing hormone stimulates pituitary prolactin secretion directly) -pharmacologic estrogens (OCP) -other rare, nonpituitary sources (lung and renal tumors) or causes of decreased prolactin clearance (renal failure). The pituitary amenorrhea Amenorrhea in case of pituitary nanism Disease develops in prenatal period or during the first months of life due to infectious diseases or traumatic damages of anterior part of pituitary. Insufficiency of all its hormones including somatotropin appears as a result. Treatment mainly is in an endocrinologist competence. One should begin treatment in childhood with grows stimulation. Further replacement hormonal therapy is indicated Amenorrhea in case of gigantism and acromegalia Diseases are caused by Somatotropin hyperprodaction, production of gonadothropic hormones is decreased. Amenorrhea has a secondary character. Treatment. At pituitary tumors rhoentgenotherapy is indicated. For Patients with gigantism estrogen therapy for stopping of excessive growth is prescribed. Itsenko-Cushing syndrome Clinical features are: fatigue, weakness, abdominal obesity, «buffalo hump» (an excessive deposit of fat over the clavicles and back of the neck), moon-shaped face, nervousness, irritability, depression, amenorrhoea or menstrual irregularity. Most commonly observed in females in childbearing age. Clinical features are: fatigue, weakness, abdominal obesity, «buffalo hump» (an excessive deposit of fat over the clavicles and back of the neck), moon-shaped face, nervousness, irritability, depression, amenorrhoea or menstrual irregularity. Most commonly observed in females in childbearing age. Sheehan's Syndrome Acute infarction and necrosis of the pituitary gland due to postpartum hemorrhage and shock is known as Sheehan's syndrome. The symptoms of hypopituitarism are usually seen early in the postpartum period, especially failure of lactation and loss of pubic and axillary hair. Deficiencies in growth hormone and gonadotropins are most common, followed by ACTH, and last, by TSH in frequency. Diabetes insipidus is not usually present. This can be a life-threatening condition, but fortunately, because of good obstetrical care, this syndrome is never encountered by most of us. The ovarian amenorrhea The Shereshevsky-Terner’s syndrome The Stein-Levental syndrome What is Turner syndrome? Relatively common disorder caused by the loss of genetic material from one of the sex chromosomes. Affects only females Genetic causes X chromosome monosomy X chromosome mosaicism X chromosome defects Symptoms Clinical features Short stature (143-145cm tall) Loss of ovarian function Hormone imbalances( thyroid, diabetes) Stress and emotional deprivation Diseases affecting the kidneys, heart, lungs or intestines Bone diseases Learning problems( esp. in maths) Gonadal failure Internal genitalia of patient with gonadal dysgenesis (Turner syndrome), featuring normal but infantile uterus, normal fallopian tubes, and pale, glistening "streak" gonads in both broad ligaments. Diagnosis Possible during infancy or early childhood A physical exam is the first indication The best test is a karyotype, ie a laboratory test presenting the chromosomes Treatment Growth hormone therapy Estrogen replacement therapy Cardiac surgery (when needed) In vitro fertilization (to achieve pregnancy) Psychological help Polycystic Ovarian Syndrome Sagittal section of a polycystic ovary illustrating large number of follicular cysts and thickened stroma. an inversion of the normal LH/FSH ratio lack of ovulation increased levels of male hormones ("androgens") insulin resistance Presentation irregular or absent menstruation/ovulation infertility undesired hair growth and acne small benign cysts on the ovaries increased risk of miscarriage obesity endometrial cancer, heart disease and diabetes Diagnosis BBT (basal body temperature) B ultrasound: multiple small ovarian cysts enlarged ovary Endometrium biopsy(Curettage ) before menses reveal to proliferative glands Determination of LH,FSH,E2,P,T,PRL,Ins,(LH:FSH≧3:1) Laparoscopy The uterine form of amenorrhea Primary – Uterus congenital anomalies Secondary – Postinflammation intrauterine synechyas – Endometrium trauma – Tuberculosis of endometrium Mayer-Rokitansky-Kuster-Hauser Syndrome (utero-vaginal agenesis) 15% of primary amenorrhea Normal secondary development & external female genitalia Normal female range testosterone level Absent uterus and upper vagina & normal ovaries Karyotype 46-XX 15-30% renal, skeletal and middle ear anomalies COMPLICATIONS OF MENSTRUATION Premenstrual syndrome Symptoms include edema, weight gain, restlessness, irritability, and increased tension. Symptoms must occur in the second half of the menstrual cycle. There must be a symptom-free period of at least 7 days in the first half of the cycle. Symptoms must occur in at least 2 consecutive cycles. Symptoms must be severe enough to require medical advice or treatment. Mastodynia Pain, and usually swelling, of the breasts caused by edema and engorgement of the vascular and ductal systems is termed mastodynia, or mastalgia. Treatment Management of painful breasts due to fibrocystic changes consists of support of the breasts, avoidance of methylxanthenes (coffee, tea, chocolate, cola drinks), and occasional use of a mild diuretic. Patients with mastodynia have had improvement with danazol, bromocriptine, oral contraceptives, and vitamins, though with limited success. I In one study, lisuride maleate, a dopamine agonist, was associated with a significant decrease in pain. Dysmenorrhea Dysmenorrhea, or painful menstruation, is the most common complaint of gynecologic patients. There are 3 types of dysmenorrhea: (1) primary (no organic cause), (2) secondary (pathologic cause), (3) membranous (cast of endometrial cavity shed as a single entity). Dysmenorrhea Typically, pain occurs on the first day of the menses, usually about the time the flow begins, but it may not be present until the second day. Nausea and vomiting, diarrhea, and headache may occur. Treatment of dysmenorrhea ANTIPROSTAGLANDINS B. ORAL CONTRACEPTIVES C. SURGICAL TREATMENT D. ADJUVANT TREATMENTS Abnormal uterine bleeding Abnormal uterine bleeding includes: – abnormal menstrual bleeding – bleeding due to other causes such as pregnancy, systemic disease, or cancer. Patterns of Abnormal Uterine Bleeding Menorrhagia (hypermenorrhea) Hypomenorrhea (cryptomenorrhea) Metrorrhagia (intermenstrual bleeding) Polymenorrhea Menometrorrhagia Oligomenorrhea Contact bleeding (postcoital bleeding) Evaluation of abnormal uterine bleeding A. HISTORY B. PHYSICAL EXAMINATION C. CYTOLOGIC EXAMINATION D. ENDOMETRIAL BIOPSY H. OTHER DIAGNOSTIC PROCEDURES Dysfunctional uterine bleeding Treatment A. ADOLESCENTS B. YOUNG WOMEN C. PREMENOPAUSAL WOMEN D. SURGICAL MEASURES ABNORMAL BLEEDING IN THE CHILDBEARING YEARS Abnormal bleeding without obvious local cause is not uncommon in women of this age group. The bleeding may be cyclical or irregular. The uterus may be slightly and symmetrically enlarged, particularly in parous women. It is not uncommon for abnormal bleeding of endocrine origin to undergo spontaneous remission; in young women without abnormal physical signs it is worth waiting for a short time to see if normal menstruation returns. When abnormal bleeding persists the following options may be tried: Under 40 years of age, one can use the combined oral contraceptive pill for non-smoking and non-obese women. Otherwise non-steroidal anti-inflammatory drugs (NSAID) which inhibit pros-taglandin synthesis in the endometrium will relieve both menorrhagia and sysmenorrhoea (e.g. mefe-namic acid 500 mg tds given during ther period). Alternatively, anti-fibrinolysins will reduce bleeding by inhibiting plasminogen activity that may cause nausea and vomiting in a third of cases (tranexamic acid is given at a dose of 1.5gtds during the period). In a woman over 40 years of age, heavy bleeding of recent onset should be managed by hyseroscopy and diagnostic D & C, to exclude endometrial pathology such as endomet-rial hyperplasia. If nothing sinister is found at D & C, other measures include danazol which competitively binds sex hormones to their receptors and inhibits their production by direct enzymatic action. It is given orally as a dose of 200-800 mg daily in divided doses. It sometimes causes unpleasant masculinizing side effects. GnRH analogues may be used to inhibit gona-dotrophin secretion but they are expensive and cause menopausal side effects and osteoporosis. If these measures fail, endometrial resection or ablation can be considered. About one third of patients will have amenorrhoea, one third will be improved and one third will be unchanged. Finally, hysterectomy may be offered when menorrhagia cannot be controlled by any of these methods and there are still some 7 years before the menopause is expected. The ovaries are not removed unless involved by pathology or over the age of 50. Between the ages of 45 and 50 the case for their removal is more controversial and needs to be discussed on an individual case with each patient. V. Self-assessment tasks: 1. What classifications of abnormalities of menstrual cycle do you know? 2. What is bleeding of juvenile period? 3. Clinical picture of certain forms of abnormalities of menstrual cycle. 4. Methods of non-hormonal hemostasis by bleedings. 5. When can hormonal hemostasis be prescribed? 6. What are the indications for surgical treatment of bleedings? 7. Make up a plan of examination of a patient with abnormalities of menstrual function. 8. Prescribe treatment to the patient with function. abnormalities of menstrual VI. Literature. VI. Literature. 1. American Academy of Pediatrics Committee on Quality Improvement, Subcommittee on Urinary Tract Infection. Practice Parameter: The diagnosis, treatment and evaluation of the initial urinary tract infection in febrile infants and young children. Pediatrics 1999;103;4:843–852. 2. Sanfilippo JS. Pediatric and Adolescent Gynecology, 2nd Ed. Philadelphia: WB Saunders, 2001:227–231. 3. Reiter EO, Lee PA. Adolescent endocrinology: delayed puberty. Adolesc Med 2002;13 (1):101–118. 4. Larsen PR. Williams Textbook of Endocrinology, 10th Ed. Elsevier, 2003:1171–1202. 5. Stenchever MA. Comprehensive Gynecology, 4th Ed. Mosby, 2001:280–288. 6. Kaplowitz PB. Reexamination of the age limit for defining when puberty is precocious in girls in the United States: implication for evaluation and treatment. Drug and Therapeutics and Executive Committees of the Lawson Wilkins Pediatric Endocrine Society. Pediatrics 1999;104 (4 Pt 1):936–941. 7. Antoniazzi F, Zamboni G. Central precocious puberty: current treatment options. Paediatr Drugs 2004;6 (4):211–231. 8. Speroff L, Glass RH, Kase NG. Clinical Gynecologic Endocrinology and Infertility, 5th Ed. Baltimore: Williams & Wilkins, 1994:380–382. 9. Eugster EA, Rubin SD, Reiter EO, et al. Tamoxifen treatment for precocious puberty in McCune-Albright syndrome: a multicenter trial. J Pediatr 2003;143 (1):60–66. 10. Speroff L, Glass RH, Kase NG. Clinical Gynecologic Endocrinology and Infertility, 5th Ed. Baltimore: Williams & Wilkins, 1994:340–342. 11. Sanfilippo JS. Pediatric and Adolescent Gynecology, 2nd Ed. Philadelphia: WB Saunders, 2001:277–287. 12. Sanfilippo JS. Pediatric and Adolescent Gynecology, 2nd Ed. Philadelphia: WB Saunders, 2001:605–608.