Fall workshop presention - Rib Fracture Management
advertisement
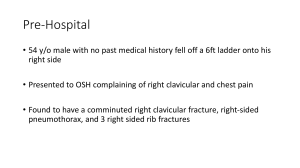
Management of Traumatic Rib Fractures Benjamin Jorgensen, MD PGY-2 University of South Dakota Surgery Department Importance? Rib Fractures • Most common injury in chest trauma – 10% of all traumas – 30% of significant chest trauma • # of rib fractures correlates with severity of injury • Geriatric population • Management largely conservative Outline • • • • • Background Anatomy Structural Physiology Injuries and mechanisms Treatments Trimodal Distribution of Death Rib fx correlating with Injury severity Graeber and Nazim, 2007. Graeber and Nazim, 2007. Graeber and Nazim, 2007. Graeber and Nazim, 2007. Case study • 80M farmer fall from ladder of tractor. • PMH/PSH: – Chronic Afib on Xarelto – CABG • Vitals: T 37 HR 110 BP 125/80 R 23 SpO2 100% 15L Mediastinal Injury Intrathoracic Injury Intraabdominal Injury *Think associated internal injury with serious trauma Associated Injuries • • • • • • • • • • Hemopneumothorax Lung parenchyma and airways Heart/Pericardium Aorta Spleen Liver Kidneys Clavicles and Scapula Spine Head Case (cont’d) Case (cont’d) Flail Segment “Three of more adjacent ribs are each fractured in two places, creating one floating segment comprised of several rib sections and the soft tissues between them.” Consequences of Rib Fractures • • • • • • • Pain Respiratory Failure Pneumonia Retained hemothorax Empyema Deformity Non-union General Management Issues • • • • • • Monitoring Pain management Respiratory therapy Fluid management DVT prophylaxis Nutrition for wound healing **Multidisciplinary approach associated with shorter ICU and hospital stay, and lower mortality. Outpatient Management • Clinical exam is going to be most important determinant of disposition. • Patients may safely be managed as an outpatient if able to clear secretions and cough with adequate pain control – ~20% return to the ED, most commonly due to inadequate analgesia • Followup chest X ray within 2 weeks. Indications for Transfer or ICU Observation • • • • • Age >65 >3 fractures Hypoxia Abnormal CXR High energy mechanism (pulmonary contusion) • Observation of pneumothorax • Other comorbidities/injuries Respiratory Care • Volume Expansion – EZ Pap – Incentive Spirometry – Acapella – Cough and deep breath • Monitor for respiratory fatigue – Intubation as needed – Flail chest increased risk. • Be cautious with IVF! Pain Management Difficult to control with multiple rib fractures leading to: – Decreased pulmonary function – Increased hospital length of stay – Increased health care expenditures **Multimodality pain approach Pain Management **Physical Exam COUGH assessment Pain Management **Goal is adequate pain relief for airway clearance. • PCA (Level 2 evidence) – Survival advantage in elderly pts with blunt trauma • IV NSAID – Decreased narcotic use – May prevent bone healing – Precaution with renal imparement Pain Management • Regional analgesia – Thoracic epidural analgesia or Thoracic paravertebral infusion • Technically demanding • Significant patient cooperation (feasibility in ICU?) – Continuous Bupivicaine (i.e. On-Q pump) • No comparative studies to epidurals in rib fx, but superior in thoracotomies • Must monitor cardiac depression (i.e. AV block, ventricular arrythmias) – Lidoderm Patches Operative Chest Wall Stabilization Case (cont’d) • Transferred to ICU from ED • Pain management with PCA and lidoderm patches pain difficult to control. • Requiring BIPAP. • HD #2, decision made to perform rib plating. Operative Chest Wall Stabilization • Indications: – Flail chest – Symptomatic fractures of 3 or more consecutive ribs – Severe chest wall deformity with or without pulm herniation – Symptomatic Nonunion – Unable to be wean from ventilator Operative Chest Wall Stabilization Studies suggest: – better pain control – earlier return to activity – potentially improved quality of life and pulmonary function tests at 6 month follow up. Case (cont’d) • Pain significantly improved. • Resp Insufficiency secondary to contusions and retained hemothorax • Transferred to floor POD #14 Summary • # of rib fractures correlates with severity of injury think associated injuries. • Be wary of geriatric patient • Cough assessment with physical exam • Multidisciplinary approach to management • Multimodality pain approach • Operative fixation for select patients Questions?