Vasopressors
advertisement

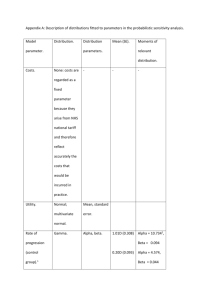
Activation of alpha-1 ◦ Postsynaptic adrenoreceptors located in smooth muscle throughout the body ◦ Increases intracellular calcium concentrations Blood vessels: Vasoconstriction Pancreas: Inhibits the release of insulin Intestine/Bladder: Relaxation, but constriction of sphincters Activation of alpha-2 ◦ Presynaptic receptors decreases NE release thru negative feedback Brain receptors lowers the blood pressure (decreases SNS activity) and causes sedation Beta-1 ◦ Located primarily on post synaptic membranes of the heart Positive chronotrope, dromotrope, and inotrope ◦ Fat Cells: Lipolysis Beta – 2 ◦ Located primarily on post synaptic smooth muscle and gland cells Blood Vessels: Vasodilation Bronchioles: Bronchodilaton Uterus: Relaxation of uterus Kidneys: Renin Secretion Liver: Gluconeogenesis, glycogenolysis Pancreas: Insulin secretion Dopamine-1 ◦ Blood Vessels: Dilates renal, coronary, and splanchnic vessels Dopamine-2 ◦ Presynaptic endings: inhibits NE release ◦ CNS: Psychic disturbances Phenylephrine ◦ Primarily direct alpha-1 agonist with minimal beta affects Arteriolar vasoconstriction Dose 50-200mcg bolus Duration 5 minutes PROS: increases CPP without increasing myocardial contractility (useful in CAD, hypertrophic subaortic stenosis, or aortic stenosis CONS: Decreased SV due to increased afterload, may increase PVR, may decrease perfusion to kidneys, gut and extremities Ephedrine ◦ ◦ ◦ ◦ ◦ Mild direct alpha, beta -1 and beta-2 agonist Primarily causes indirect release of NE Dose 5-10mg IV bolus Duration 3-10min PROS: Easy to titrate and rarely produces unexpected exaggerated response, does not reduce perfusion to placenta, ideal solution to correct sympathectomy induced hypovolemia and decr SVR ◦ CONS: Efficacy is reduced when NE stores are depleted Risk of malignant hypertension if used with MAOi Tachyphylaxis with repeat doses Norepinephrine ◦ Primary postganglionic sympathetic neurotransmitter ◦ Direct alpha 1&2 and beta-1 ◦ Starting Dose .05-.5 mcg/kg/min IV infusion via central access only ◦ PROS: Direct agonist, redistributes blood flow to the brain and heart because all other vascular beds are constricted ◦ CONS: Reduced organ perfusion: risk of ischemia to kidneys, gut, liver, skin and extremities, causes pulmonary vasoconstriction, arrhythmias, and possible skin necrosis with extravasation Epinephrine ◦ Catecholamine produced by the adrenal medulla ◦ Direct alpha 1&2, and beta 1&2 ◦ Peripheral vasoconstriction increases diastolic pressure ◦ PROS: Direct acting, potent alpha and beta activity gives max effects and give equivalent increases in SV, less tachycardia after heart SX than other ionotropes, effective bronchodilator ◦ CONS: Tachycardia and arrhythmias, potential organ ischemia including MI, increases PVR Dose(mcg/kg/min) Receptors Activated SVR 0.01-0.03 Beta May decrease 0.03-0.15 Beta >alpha Variable 0.15-0.5 Alpha 1 + Beta Increased Dopamine ◦ Direct alpha 1 and beta 1&2… and dopaminergic agonist ◦ Indirect action : releases stored NE ◦ Pros: increases renal perfusion and urine output at low doses, BP response is easy to titrate due to its mixed vasopressor/inotropic effects ◦ Cons: response can diminish when NE stores depleted, sinus/atrial/ventricular tachycardia or arrhythmias may occur, max inotropic effect less than epi, skin necrosis may occur w/ extravasation, MVO2 increases, and MI may occur if coronary blood flow doesn’t increase simultaneously, incr BP at higher doses may be detrimental to failing heart Dopamine Dose (mcg/kg/min) Receptors Activated Effect 1-3 Dopaminergic (DA1) Increased renal & mesenteric blood flow 3-10 Beta 1 & 2 (plus DA1) Incr HR, CO, contractility, and PVR decreased SVR >10 Alpha (plus beta&DA1) Increased SVR, PVR,HR, arrhythmias Decreased renal blood flow and poss CO Vasopressin ◦ Endogenous antidiuretic hormone that produces direct peripheral vasoconstriction thru V1 receptors ◦ Pros: effective in increasing SVR in severe acidosis, sepsis, and after CPB, cerebral vasodilator, may restore CPP after cardiac arrest without producing tachycardia ◦ Cons: Unpleasant symptoms in awake patients( abd cramping, uterine contractions, nausea, bronchoconstriction, skin pallor, incr liver enzymes and perfusion to gut with prolonged use, decr plts, lactic acidosis Utilized to suppress ventricular ectopy Lidocaine ◦ Depresses automaticity by reducing slope of phase 4 depolarization Amiodarone ◦ ◦ ◦ ◦ Na, K, Ca, alpha, and beta blocking properties Stabilizes atrial and ventricular membranes Utilized in ACLS for refractory VF and dysrhthmias May causes hypotension and bradycardia Atropine ◦ Vagolytic effect enhances sinus node automaticity and AV conduction Sodium Bicarbonate ◦ No longer routinely utilized in ACLS Use restricted to arrest associated with hyperkalemia, pre-existing metabolic acidosis, tricyclic/phenobarbital ◦ Cons: metabolic alkalosis, hypernatremia, hyperosmolarity Calcium ◦ Increases contractility and increases ventricular automaticity ◦ CaCl produces higher and more consistent levels of ionized calcium than other salts