Supplementary Information (docx 15K)
advertisement
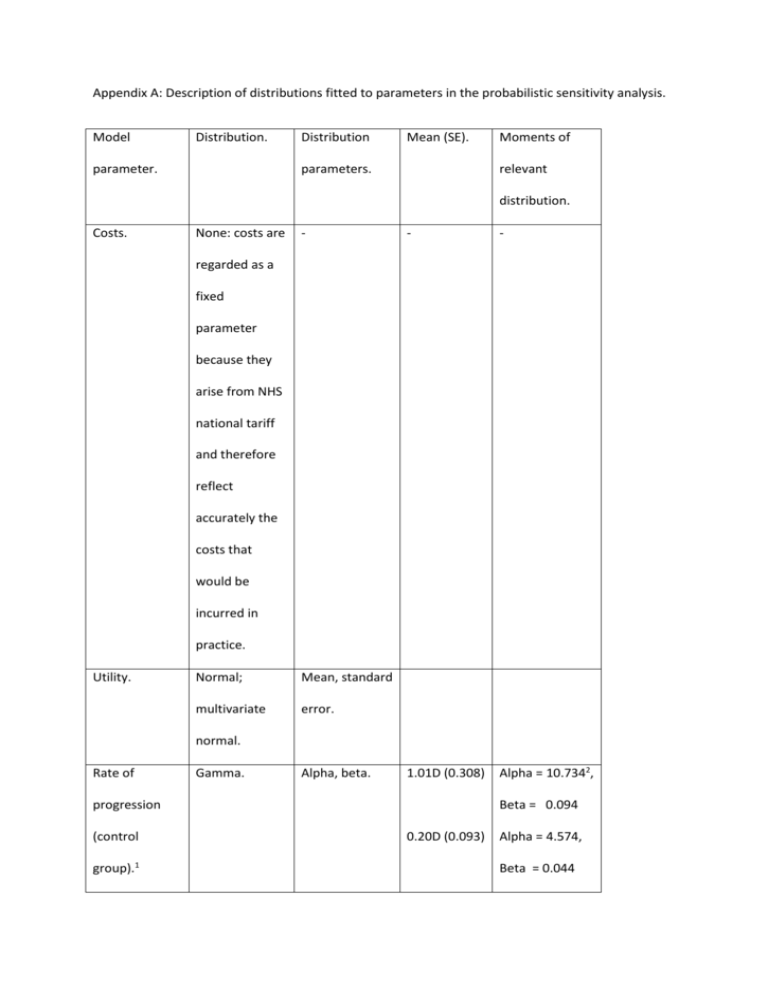
Appendix A: Description of distributions fitted to parameters in the probabilistic sensitivity analysis. Model Distribution. parameter. Distribution Mean (SE). parameters. Moments of relevant distribution. Costs. None: costs are - - - 1.01D (0.308) Alpha = 10.7342, regarded as a fixed parameter because they arise from NHS national tariff and therefore reflect accurately the costs that would be incurred in practice. Utility. Normal; Mean, standard multivariate error. normal. Rate of Gamma. Alpha, beta. progression (control group).1 Beta = 0.094 0.20D (0.093) Alpha = 4.574, Beta = 0.044 Probability of Uniform. grafting per Lower and 0.001 Upper bounds. Lower = 0.0003 Upper = 0.003 cycle once in AK Stage 4. Efficacy of Beta. Alpha, beta. 0.076 initial collagen Alpha =7.6 Beta = 92.4 crosslinking treatment. Efficacy of Uniform. Lower and No fixed Lower= upper bounds. value as this proportion crosslinking at is a successful at 5 year conditional first treatment retreatment distribution Upper = 1 interval based on the (Expressed as value the proportion selected for of treatments the first five which fail). years3. collagen Proportion of Standard Lower and patients Uniform. upper bounds. Standard Lower and 0.5 0,1 0.5 0,1 retreated with collagen crosslinking at 5 year interval. Probability of starting model Uniform. upper bounds. in AK state 1 or State 2 is 2. conditional on state 1. Probability of Beta. Alpha, beta. 3/93 cataract after Alpha = 3 Beta = 90 grafting. Probability of Beta. repeat Alpha, beta. 1/93 Alpha = 1 Beta = 92 grafting. Notes 1. Rates of progression for the treatment group were calculated by multiplying control rates by a constant, with standard errors adjusted accordingly. The rate of progression in the second eye never exceeds that of the first. 2. All gamma and beta parameters were calculated by the method of moments. 3. That is to say, if the initial efficacy for the first five years is expressed as some value k (0<k<1), and u ~ U(0,1), then the values ud this distribution are given by ud = 1-((1-k)u). Utilities for the bilateral states were correlated using the Cholesky decomposition method, in order to prevent simulations arising in which utility increased with worsening disease. To do this we used a correlation coefficient between visual acuity and utility of -0.477, derived by taking Brown’s measured correlation of 0.477, and adding the minus sign to account for the change in unit from Snellen (Brown) to logMAR. Although correlation coefficient does not normally change with the change of units, in this case a change was required because the measurement concept behind each method is different. Specifically, Snellen values (when expressed as a decimal) decrease as vision worsens, whereas logMAR values will increase. The adequacy of this substitution was established using a simulation, in which a set of visual acuities, measured in both units, was correlated to a set of utility values.