AMP
advertisement

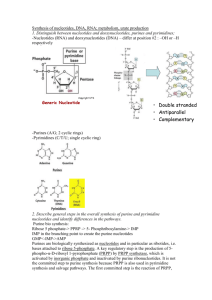
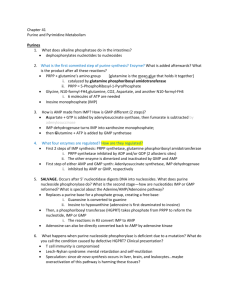
CASE: BUSINESSMAN WITH PAIN IN BIG TOE • History Of Presenting Illness: Started to have severe pain in his big toe in the early morning . Binge eating and drinking (beer) at a dinner party last night. • Past history: Similar attacks in the past. Kidney stones removed 2 years back. • Social history: Upper middle class, drinks beer every night • Musculoskeletal: The big toe red, hot and swollen; painful to active and passive movement; tophaceous deposits in left ear and olecranon bursitis. • Investigations: WBCs: 12000, Serum Uric Acid: 8.0 mg/dL • X-ray: Punched-out erosions in right big toe at metatarsophalangeal joint, producing “overhanging’’ spicules LEARNING OBJECTIVES Describe the metabolic basis of gouty arthritis including • the key reactions of de novo and salvage pathway in the biosynthesis of purine ribo- and deoxyribonucleotides (Focus on the sources of the individual atoms in the purine rings and the key regulatory steps) • the key steps in the degradation of purines • causes of primary and secondary hyperuricemia Also familiarize yourselves with • the basis of other disorders associated with the nucleotide metabolism (Lesch-Nyhan syndrome, adenosine deaminase deficiency) • why/how nucleotide analogs and inhibitors of nucleotide synthesis are used in various drug therapies Q. Nucleotides serve all of the following roles EXCEPT A. B. C. D. E. monomeric units of nucleic acids physiological mediators sources of chemical energy structural components of membranes structural components of coenzymes FUNCTIONS OF NUCLEOTIDES • Polymerize to make DNA and RNA • Energy currency of the cell e.g. ATP, GTP • Act as carriers of active intermediates in various metabolic pathways e.g. UDP-glucose in glycogen synthesis, SAM • Component of coenzymes e.g. FAD, NADH, NADPH • Act as 2nd messengers e.g. cAMP and cGMP • Allosteric regulation of various metabolic pathways e.g. ATP inhibits PFK-1 NITROGENOUS BASES A B Q. Which one of the following is not a purine? A. B. C. D. E. Adenine Guanine Cytosine Xanthine Hypoxanthine THE PENTOSE SUGARS A B NUCLEOTIDE SYNTHESIS: DE NOVO AND SALVAGE PATHWAYS De novo pathway Synthesis from low molecular weight precursors Salvage pathway Synthesis from nucleosides or bases that become available through the diet or from degradation of nucleic acids Q. Which of the following do NOT serve as a source of C in purine ring synthesis? A.CO2 B.Glycine C.Aspartate D.Glutamine E.Tetrahydrofolate DE NOVO PURINE SYNTHESIS Source of Nitrogen • 2 from Glutamine • 1 from Aspartate • 1 from Glycine Source of Carbon • 2 from Glycine • 2 from N10-Formyl tetrahydrofolate • 1 from CO2 DE NOVO PURINE SYNTHESIS PURINE SYNTHESIS: PRPP SYNTHESIS PURINES ARE NOT MADE AS FREE BASES – BUT AS NUCLEOTIDES 5’-PRPP GLUTAMINE 1 PPi DISPLACEMENT BY NH2 GLYCINE + ATP 2 ADDITION OF GLYCINE N10-FORMYL THF 3 FORMYL GROUP TRANSFER 4 NH2 GROUP TRANSFER ATP 5 RING CLOSURE CO2 6 COO- ADDITION 7 ASPARTATE ADDITION 8 FUMARATE LOSS 9 FORMYL GROUP TRANSFER GLUTAMINE + ATP ASPARTATE + ATP N10-FORMYL THF 10 RING CLOSURE INOSINE 5’- MONOPHOSPHATE (IMP) INOSINE 5’- MONOPHOSPHATE (IMP) Adenylosuccinate synthetase GTP + Asp GDP + Pi Adenylosuccinate Adenylosuccinase Fumarate NAD+ IMP dehydrogenase NADH Xanthine monophosphate (XMP) ATP + Gln GMP synthetase AMP + Glu Adenosine monophosphate (AMP) Guanosine monophosphate (GMP) CONVERSION OF NMP TO NDP & NTP Base specific nucleoside monophosphate kinases AMP + ATP Adenylate kinase 2ADP GMP + ATP Guanylate kinase GDP + ADP Nucleoside diphosphate kinases GDP + ATP GTP + ADP CDP + ATP CTP + ADP Q. Which one of the following is NOT a regulatory enzyme of nucleotide metabolism? A. B. C. D. E. PRPP Synthetase GMP synthetase IMP dehydrogenase Gln:PRPP amidotransferase Adenylosuccinate synthetase REGULATION OF PURINE SYNTHESIS Ribose 5 Phosphate PRPP synthetase PRPP Amido tranferase 5-Phosphoribosylamine Adenylosuccinate synthetase Adenylosuccinate IMP IMP dehydrogenase XMP AMP GMP ADP GDP ATP GTP ENERGY REQUIREMENTS FOR PURINE SYNTHESIS a) Ribose-5-PO4 IMP TOTAL = 6 high energy bonds 4 ATP, 1 PPi (2 high energy bonds) 1 GTP b) IMP AMP TOTAL = 7 high energy bonds 1 ATP c) IMP GMP TOTAL = 7 high energy bonds PURINE NUCLEOTIDE SYNTHESIS: THE SALVAGE PATHWAY Hypoxanthine Guanine Hypoxanthine-guanine phosphoribosyltransferase PRPP PPi Hypoxanthine-guanine phosphoribosyltransferase PRPP Adenine Adenosine GMP PPi Adenine phosphoribosyltransferase PRPP PPi Adenosine kinase ATP IMP ADP AMP AMP RIBONUCLEOTIDES DEOXYRIBONUCLEOTIDES ADP GDP CDP UDP Ribonucleotide reductase dADP dGDP dCDP dUDP RIBONUCLEOTIDES DEOXYRIBONUCLEOTIDES NDP Thioredoxin NADP+ Thioredoxin reductase NADPH SH SH Ribonucleotide reductase Thioredoxin S S dNDP Q. The regulation if ribonucleotide reductase is complex! Assume an enzymic deficiency that leads to an increase in the cellular levels of dATP which one of the following is most likely to occur? A.The formation of dADP will be favored B.The cellular levels of AMP will be reduced C.Elevated levels of all dNTPs will occur D.The formation of all dNTPs will be reduced E.Reduced thioredoxin will not be formed RIBONUCLEOTIDE REDUCTASE • CATALYTIC SITE – Converts NDPs to dNDPs • ACTIVITY SITE – Activation by ATP – Inhibition by dATP • SUBSTRATE SPECIFICITY SITE – Binding by ATP = CDP & UDP→ dCDP & dUDP – Binding by dTTP = GDP → dGDP – Binding by dGTP = ADP → dADP DEGRADATION OF PURINE NUCLEOTIDES Q. Uric acid is A. B. C. D. E. a degradation product of cytidine deficient in the condition known as gout a competitive inhibitor of xanthine oxidase formed from xanthine in the presence of O2 oxidized, in humans, before it is excreted in urine DEGRADATION OF PURINE NUCLEOTIDES AMP deaminase AMP IMP Pi 5’ Nucleotidase Adenosine Adenosine deaminase GMP Pi 5’ Nucleotidase Inosine Pi Guanosine Ribose Ribose 5’ Phosphorylase Guanine Hypoxanthine Uric Acid (excreted) Xanthine oxidase Xanthine Xanthine oxidase Guanase NH3 DISEASES ASSOCIATED WITH DEFECTS IN PURINE METABOLISM • • • • • HYPERURICEMIA GOUT LESCH-NYHAN SYNDROME KIDNEY STONES SEVERE COMBINED IMMUNODEFECIENCY (SCID) HYPERURICEMIA Characterized by plasma urate (uric acid) level greater than 7.0 mg/dL Normal plasma levels Females = 2.4 - 6 mg/dL Males = 3.4 - 7 mg/dL HYPERURICEMIA •Primary Hyperuricemia: an innate defect in purine metabolism and/or uric acid excretion •Secondary Hyperuricemia: increased availability of purines due to medications/ medical conditions or through diet. GOUT Gout is caused by precipitation of sodium urate crystals in the joints resulting in inflammation and pain. Progression of Hyperuricemia to Gout Stage 1: Asymptomatic hyperuricemia. At a serum urate concentration greater than 6.8 mg/dL, urate crystals may start to deposit in the joints. No evidence that treatment is required. Stages 2 : Acute gout. If sufficient urate deposits develop around joints, and if the local environment or some trauma triggers the release of crystals into the joint space, an inflammatory response occurs. These flares can be self-resolving but are likely to recur. Stage 3: Intercritical periods. These are the intervals between attacks. During these periods, crystals may still be present at a low level in the synovial tissue and fluid, resulting in future attacks. Stage 4: Advanced gout. If crystal deposits continue to accumulate, patients may develop chronically stiff, swollen joints and tophi. This advanced stage of gout is relatively uncommon generally avoidable with therapy. Clinical features – Swollen MTP joint and ankle Clinical features - tophaceous deposits in left ear Clinical features – Olecranon bursitis Clinical features – punched out erosions with overhanging spicules GOUT - DIAGNOSIS Definitive diagnosis is made by the presence of urate crystals in the synovial fluid of the joint – crystals are needle-shaped and negatively birefringent GOUT - Causes • Underexcretion of uric acid • Diet rich in purines/alcohol; deficient in dairy products • Increased purine degradation • Increased PRPP Synthetase activity overproduction of PRPP = increased purine synthesis = increased purine degradation = increased uric acid production • Decreased/partial HGPRT activity 1) Deficiency of HGPRT = increased HX and G 2) Deficiency of HGPRT = accumulation of PRPP = increased purine synthesis = increased uric acid levels 3) Deficiency of HGPRT = decreased IMP and GMP = decreased inhibitors for purine synthesis GOUT - Treatment • Colchicine –reduces inflammation • Uricosuric agents – increase renal excretion of uric acid (probenecid) • Allopurinol – inhibits uric acid synthesis • Low purine diet - Foods that are high in purine include: – Red meat and organ meats (eg. liver) – Yeasts and yeast extracts (eg. beer and alcoholic beverages) – Asparagus, spinach, beans, peas, lentils, oatmeal, cauliflower and mushrooms • Avoid caffeine and alcohol • Keep hydrated KIDNEY STONES When uric acid is present in high concentrations in the blood, it may precipitate as a salt in the kidneys. The salt can form stones, which can in turn cause pain, infection, and kidney damage. LESCH-NYHAN SYNDROME • X-Linked recessive disorder • Complete HGPRT deficiency • Characterized by mental deficiency, aggression, self-destructive behavior, characterized by lip and finger biting. • Since high urate levels are present in the blood, individuals with this condition are also prone to gout and kidney stones Q. Lesch-Nyhan disease is due to the inability to catalyze which one of the following reactions? A. B. C. D. E. AMP to ATP Adenine to AMP Guanine to GMP Adenosine to AMP Hypoxanthine to xanthine SEVERE COMBINED IMMUNODEFICIENCY (SCID) • Adenosine deaminase deficiency • Accumulation of dATP = inhibition of ribonucleotide reductase =B and T cells unable to divide Q. Methotrexate affects nucleotide synthesis by inhibiting A.IMP dehydrogenase B.dihydrofolate reductase C.dihydropteroate synthase D.glutamine:PRPP amidotransferase E.PRPP synthase