5-P
advertisement

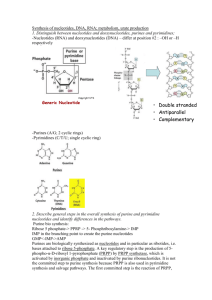
Prof. Mária Sasvári NUCLEOTIDE METABOLISM Metabolism of purine nucleotides Gergely Keszler 2009. 1 The biological role of nucleotides 1. Building blocks of nucleic acids (DNA and RNA) 2. Storage of biochemical energy (ATP and GTP) 3. Activation of biosynthetic precursors (UDP-glucose, CDP-choline) 4. Components of coenzymes (NAD, FAD, Coenzyme A etc.) 5. Regulation of metabolism (cAMP, cGMP) 6. Nucleotide analogues: anticancer and antiviral therapies 2 Terminology of nucleotides phosphoanhydride bonds phosphoester bond N-glycosidic bond Nucleotides are composed of: a nucleobase a nucleoside a pentose at least one phosphate group 3 Ribo- and deoxyribonucleotides (Ado) (Guo) (Urd) (Cyd) (dAdo) (dGuo) (Thd) (dCyd) 4 Structures of nucleobases N-containing, heterocyclic aromatic compounds; substituted purine or pyrimidine rings RNA DNA 5 Nucleotide synthesis „de novo” stepwise assembly from small precursors (C1 fragments, CO2, amino acids, ribose-P) salvage (recycling) • base + ribose-P → nucleotide (typical for purines) OR • nucleoside + Pi → nucleotide (typical for pyrimidines) 6 The origin of ribose-P glc-6-P PPP fru-6-P ATP ri-5-P PRPP synthetase AMP 5’ P-O-H2C O O-P P 1’ PRPP Purine “de novo” and salvage reactions Pyrimidine “de novo” synthesis 7 Intestine Food Blood brain, RBC, lymphocytes RNA, DNA “salvage reactions” polynucleotides nucleotides nucleosides bases nucleosides bases “de novo” synthesis nucleotides urate URINE liver DNA RNA nucleosides bases urate 8 Purine nucleotide synthesis ATP ADP AMP GTP GDP GMP IMP purine bases salvage reactions “de novo” synthesis 9 The origin of the purine ring IMP Asp N6 7 N10formyl H4F CO2 5 4 N 2 Glycine N 1 N 3 N10formyl H4F Gln 10 “de novo” purine synthesis CO2 Asp N Glycine N PRPP Gln + H2O N10formyl H4F N N N10formyl H4F 1. Gln PRPP amidotransferase Gln 9. Glu + PPi NH3+ ri-5-P PRA (5-phosphoribosyl-1-amine) Glycine ATP 2. GAR synthetase ADP + Pi 11 “de novo” purine synthesis CO2 Asp N10formyl H4F NH3+ N Glycine N 9. N N Gln N10formyl H4F 9. NH O ri-5-P GAR (5’PR-Glycinamide) N10formyl H4F 3. GAR formyltransferase H4F 12 “de novo” purine synthesis CO2 Asp N10formyl H4F NH N Glycine N 9. N N Gln N10formyl H4F O NH O ri-5-P FGAR (5’PR-formyl-glycinamide) Gln 4. ATP FGAM synthetase Glu ADP + Pi 13 “de novo” purine synthesis CO2 Asp N10formyl H4F NH N Glycine N 9. N N Gln N10formyl H4F HHN 2N NH O ri-5-P FGAM (5’PR-formylglycinamidine) ATP 5. AIR synthetase ADP + Pi 14 “de novo” purine synthesis CO2 Asp N10formyl H4F N N Glycine N 9. N N Gln N10formyl H4F H2N N ri-5-P AIR (5’PR-5-amino-imidazole) CO2 6. AIR carboxylase 15 “de novo” purine synthesis CO2 Asp N Glycine N N10formyl H4F 9. N N Gln -OOC N N10formyl H4F H2N N ri-5-P CAIR (5’PR-4-Carboxy- 5-amino-imidazole) Asp ATP 7. SAICAR synthetase ADP + Pi 16 “de novo” purine synthesis CO2 Asp N10formyl H4F O N Glycine N 9. N N succinyl- HN N N10formyl H4F Gln H2N N ri-5-P SAICAR (5’PR-succinyl-5-aminoimidazole-4-carboxamide) 8. Adenylosuccinase (ASA) fumarate 17 “de novo” purine synthesis CO2 Asp N10formyl H4F O N Glycine N 9. N N H2N N10formyl H4F N Gln H2N N ri-5-P ACAIR (5’PR-5-aminoimidazole-4-carboxamide N10formyl H4F 9. AICAR transformylase H4F 18 “de novo” purine synthesis CO2 Asp N10formyl H4F O N Glycine N 9. N N H2N N N10formyl H4F Gln O N H N ri-5-P FACAIR 5’PR-5-formamidoimidazole-4-carboxamide) 10 . IMP cyclohydrolase H2O IMP 19 ATP ADP AMP GTP GDP GMP IMP “de novo” purine synthesis and the purine nucleotide cycle AMP AMP DA (6-amino) GMP (2-amino-6-oxo) AMP+PPi GS ASL ATP fumarate Gln Xanthylate Adenylosuccinate ASS (2,6,-dioxo) GDP+Pi NADH + H+ IMPDH GTP Asp NAD+ H2 O IMP(6-oxo) 20 The role of the purine nucleotide cycle ADP + Pi ATP 2 ADP AMP kinase ATP + AMP Substrate level/oxidative phosphorylation AMP DA IMP urate PNC Adenylosuccinate severe Pi deficiency [AMP] hyperuricaemia 21 e.g. fructose intolerance Muscle: high AMP DA level Muscle Liver ATP AMP + glycolysis NH3 NH3 IMP inosine urate inosine urate strenuous exercise: NH3 , urate Muscle AMP DA def.: cramps, NH3, urate is NOT elevated 22 “de novo” purine synthesis Summary No free purine base during synthesis Carbon donors: „C1 units” (N10-formyl-THF) CO2 Glycine N-donors: Asp Gln Gly Energy: 6 ATP for 1 IMP Multifunctional proteins 23 AMP of de novo purine GMP Regulation synthesis “salvage” ATP ADP AMP IMP + + GTP GDP GMP “salvage” - IMP Gln PRPP amidotransferase + PRPP - IMP, GMP, AMP PRPP synthetase - ATP,GTP 24 Purine salvage reactions ATP ADP AMP PRT (phosphorybosyl transferase) base + ribose-P nucleotide APRT AMP adenine PRPP PPi HGPRT hypoxantine guanine PRPP GTP GDP GMP IMP purine bases salvage reactions “de novo” synthesis IMP GMP PPi 25 The Lesch-Nyhan syndrome HGPRT deficiency: low GTP levels in the basal ganglia Hyp/G + PRPP → IMP/GMP + PPi linked to X-chromosome mental retardation self-mutilation aggression hyperuricemia 26 Catabolism of purine nucleotides AMP B r -p 5’nucleotidase Pi adenosine deaminase Pi B adenosine (6-amino) H2O ADA GMP r guanosine NH3 inosine (6-oxo) Pi PNP (purine nucleoside Pi phosphorylase) ri-1-P ri-1-P hypoxantine guanine B 27 Purine salvage reactions hypoxantine (6-oxo-purine) guanine (2-oxo-6-amino-purine) E H 2 O + O2 x xanthine c (2,6-dioxopurine) H2O2 r xanthine oxidase H2O + O2 e t H2 O2 i o urate n (2,6,8-trioxopurine) H2 O guanase NH3 URINE 28 Why is uric acid acidic? uric acid (oxo) uric acid (enol) urate (dissociated anion) well soluble poor solubility precipitates in joints, initiates chemical arthritis GOUT 29 Hyperuricemia (gout) Symptoms: urate crystals on the napkin (Lesch-Nyhan) Na-urate crystals kidney stones urate in connective tissues and joints: „tophus”, inflammation, pain acute gouty arthritis chronic gouty arthritis Reason: Urate has low solubility (especially at acidic pH ) 30 Reasons for hyperuricemia 1. PRPP overproduction • as a consequence of mutation at the allosteric site of PRPP synthase, the enzyme cannot be inhibited gl-6-P •overproduction of ribose-5-P PPP fr-6-P e.g. gl-6-phosphatase deficiency (von Gierke’s disease) Gl- 6-P fr- 6-P ri- 5-P ri-5-P PRPP 31 Reasons for hyperuricemia 2. Absence of purine salvage reactions ATP ADP AMP e.g. HPRT deficiency Decreased adenine, guanine reutilization purine increased excretion bases GTP GDP GMP IMP salvage reactions “de novo” synthesis 32 Reasons for hyperuricemia 3. Low ATP level, disturbed ATP metabolism • strenuous exercise • fructose intolerance (phosphate trap) 2 ADP see before AMP kinase ATP + AMP AMP DA AMPS IMP urate 33 Reasons for hyperuricemia 4. Secondary reasons: • tissue damage • cancer, cell damage DNA breakdown overproduction of purines • Overproduction of organic anions (lactate, ketone bodies, drug derivatives) 34 Medication of gout: allopurinol hypoxanthine Xanthine oxidase allopurinol alloxanthine xanthine oxopurinol Competitive inhibitors Hypoxanthine and xanthine in urine (better solubility) 35 Allopurinol, a special purine analogue N-7 and C-8 have been scrambled up Blocks xanthine oxidase, the enzyme catalyzing the oxidation of xanthine to uric acid – cures gout 36 Enzyme deficiency: ADA / PNP / (ADA + PNP) Symptoms: immunodeficiency, “NON-HIV AIDS” Reason: B/T lymphocyte deficiency Mechanism: adenosine dATP (ATP) dATP inhibits ribonucleotide reductase inhibits DNA synthesis promotes apoptosis Treatment: ADA enzyme therapy, gene therapy 37 Adenosine deaminase functions on the outer surface of red and white blood cell membranes (ectoenzyme) binding glycoprotein („complexing factor”) 38 The pathogenesis of SCID - selective lymphotoxicity 1. Extracellular accumulation of (deoxy)adenosine (d)Ado A2 A1 Gi Gs dAdo cAMP cAMP Inhibition of the SAM/SAH cycle Impaired DNA synthesis 39 The pathogenesis of SCID - selective lymphotoxicity 2. Intracellular accumulation of (deoxy)adenosine triphosphate Inhibition of ribonucleotide reductase Inhibition of cell proliferation dCK dAdo dAdo dATP dAMP AK DNA strand breaks Lymphocyteselectivity!! Inhibition of DNA polymerases apoptosis 40 Clinical manifestation of SCID Recurring, opportunistic infections: candidiasis, Pneumocystis-pneumonia Absence of lymph nodes, no thymic shadow upon chest X-ray examination Severe impairment of both humoral and cellular immunity: lower than 500/μl total lymphocyte count very low plasma immunoglobulin levels Untreated patients die before their age of 2 years 41 Treatment of ADA deficiency 1. Treatment of symptoms Infections antibiotics, antiviral and antifungal drugs Immunoglobulin supplementation Maternal immunoglobulins are effective in the first few weeks of life 42 Treatment of ADA deficiency 2. Enzyme substitution Red blood cell transfusion Polyethylene-glycol-conjugated recombinanat ADA (PEG-ADA): intramuscular injection costs: 250,000 USD a year 43 Treatment of ADA deficiency 3. Gene therapy Principle: Introduction of the normal allele into the patients’ own stem cells Ex vivo: Stem cells are transfected and transplanted into the patient 44 Ex vivo gene therapy 45 Ashanti da Silva: the first patient in the world treated by retrovirus-mediated ADA gene therapy The introduced ADA gene functioned fine for a few months. Later on, PEG-ADA substitution therapy must have been restarted due to inactivation of the gene. 46