Aprile
Strategies to overcome resistance in NSCLC
with driver mutations
Piano Generale di Emergenza
Federico Cappuzzo
Presidio Ospedaliero
di Livorno
Istituto Toscano Tumori
Ospedale Civile
Viale Alfieri 36
Livorno-Italy
2
First-line therapy for metastatic NSCLC in 2012
Stratification for EGFR, ALK and histology
EGFR mutated
EGFR-TKI
ALK+
Crizotinib
EGFR WT nonsquamous
EGFR WT
squamous
Platinum +
pemetrexed
+/bevacizumab
Platinumbased doublet
Mut+ NSCLC: EGFR-TKI Acquired Resistance
Baseline
Tumor regression
(RR up to 90%)
Progression
(median 9 months)
Disease Flare: Hospitalization and/or death attributable to disease progression
after discontinuation of gefitinib or erlotinib and before initiation of study drug
Risk of disease flare in EGFR mut+ NSCLC with
acquired resistance: Chaft J et al. (O 19.05)
Characteristic: Total patients=61
Male sex – N (%)
N (% or range)
13 (21)
Age at diagnosis (years)
Median (range)
58 (26-78)
EGFR mutation – N (%)
Exon 19 deletion
Exon 18 G719A
Exon 21 L858R
41 (67)
1 (2)
19 (31)
Time on gefitinib or erlotinib (months)
Median (range)
19 (7-78)
Age in years - Median (Range)
61 (27-80)
Karnofsky Performance Status (%)
90%
80%
70%
13 (21)
37 (61)
11 (18)
•
14 of 61 patients (23%, 95% CI 14-35%) had a
disease flare (hospitalization or death)
–
Flare & no flare group – same 30 day pretrial
hospitalization rate
•
Median time from last TKI to flare was 8 days
(range 3-21 days)
•
3 patients went on to trial treatment
Changes in Tumor Diameter (RECIST) After
Discontinuation and Re-introduction of EGFR TKI
Change from baseline
50%
20%
0%
-30%
EGFR TKI
re-start
stop
3 weeks
3 weeks
Riely et al, CCR 2007
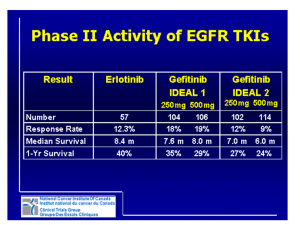
Mechanisms responsible for EGFR-TKI
resistance
Sequist et al, Science Transl Med 2011
EGFR-TKI resistance
A
B
T790M Mutation causes drug resistance by
increasing affinity for ATP
Yun PNAS 2008
T790M mutations in EGFR-TKI naive NSCLC
• Present in up to 50% of NSCLC with EGFR-TKI
acquired resistance
• Rare event in EGFR-TKI naive NSCLC (<3%) using low
sensitive methods
• Detected in up to 40% of EGFR-TKI naive patients
using high sensitive methods
Presence of T790M mutation predicts poor
outcome to EGFR-TKI
Su et al. JCO 2012; Rosell et al. Clin Cancer Res 2011;
T790M mutation and acquired resistance to gefitinib
therapy
Irreversible EGFR-TKI are still effective
Kobayashi et al. NEJM, 352, 786-792, 2005
Afatinib: Dual irreversible EGFR-HER2
inhibitor
•
Orally bioavailable, small molecule
tyrosine kinase inhibitor (TKI)
Afatinib
•
Designed to irreversibly bind to the
ATP binding pocket of EGFR and
HER2
•
Highly specific for EGFR and HER2
EGFR IC50:
0.50 nM
HER2 IC50:
14 nM
EGFR or HER2
+ ATP binding pocket
Afatinib: active against resistance mutation
BIBW2992 but not erlotinib is active against cells expressing T790M
EGFR mutation:
NCI-H1975
Li et al. Oncogene. 2008;27:4702–4711
Afatinib + cetuximab as the best option in
presence of EGFR T790M mutation
Regales et al. JCI 2009
Afatinib + cetuximab for metastatic NSCLC:
Study Design
Phase Ib, open-label, multicenter trial in the US and The Netherlands
NSCLC with
EGFR mutation1
Dose escalation schema 3–6 patients
per cohort
OR
Afatinib p.o. daily + escalating doses
of i.v. cetuximab q 2 weeks
SD 6 months
with erlotinib/gefitinib
OR
Partial or complete
response
to erlotinib/gefitinib
Disease
progression2
Stop erlotinib/
gefitinib for
≥72 hours3
Dose levels starting at:
afatinib 40 mg +
cetuximab 250 mg/m2
Predefined maximum dose:
afatinib 40 mg +
cetuximab 500 mg/m2
MTD cohort expanded up to 80 EGFR
mutation-positive patients4:
40 T790M+ and 40 T790M–
1EGFR
G719X, exon 19 deletion, L858R, L861Q; 2Progression of disease (Response Evaluation Criteria in Solid Tumors v1.1) on
continuous treatment with erlotinib or gefitinib within the last 30 days; 3Amended from original 14-day interval; 4Acquisition of tumor
tissue after the emergence of acquired resistance was mandated.
i.v.=intravenous; MTD=maximum tolerated dose; NSCLC=non-small cell lung cancer; SD=stable disease.
Tumor Regression by T790M Mutation Status
at Recommended Dose
39 patients with proven EGFR T790M mutation: confirmed RR=31%
Acquired resistance to EGFR-TKIs
• Acquired drug resistance is almost inevitable (~10 months)
• About 30% of resistant mechanisms are unknown.
Mitsudomi, et al. Cancer Sci., 2007
Resistant mechanisms in 33 tumors from 6
patients with EGFR-TKI acquired resistance
Tumors with T790M
Number of Tumors
Tumors without T790M
<2.0
2.0 - 4.0
< 4.0
MET gene copy numbers (folds)
Suda et al. Clin Cancer Res 2010
Inhibition of both EGFR and MET is necessary for
growth inhibition of HCC827 GR cells
125
Gefitinib
PHA665752
Gefitinib/PHA665752
% of control
100
75
50
25
0
0
0.01
0.1
Drug Concentration (
1
10
μ M)
•
Irreversible EGFR inhibitors have no effect on HCC827 GR
•
MET shRNA restores sensitivity to gefitinib
Engelman et al. Science 2007
EML4-ALK fusion oncogene in NSCLC
3–7% of patients with NSCLC have an
EML4-ALK gene fusion1
detection test available
mainly seen in adenocarcinomas
(mutually exclusive with EGFR
mutations)2
phase I/II trial of crizotinib, oral
c-MET and ALK inhibitor in selected
patients: DCR = 70%3
further potential for personalising
therapy in NSCLC
1. Koivunen, et al. Clin Cancer Res 2008
2. Shaw, et al. ASCO 2009; 3. Bang, et al. ASCO 2010
ALK secondary mutations and crizotinib
resistance
Sasaki et al. Cancer Res 2011
New ALK inhibitors TAE684 and AP26113 overcome
crizotinib resistance in H3122 CR cell line
Katayama et al. PNAS 2011
Cell lines with ALK secondary mutation and ALK
and EGFR co-dependency
Sasaki et al. Cancer Res 2011
ALK amplification or ALK FISH loss as
mechanisms of crizotinib resistance
Katayama et al. PNAS 2011, Katayama et al Science Transl Med 2012, Doebele et al. Clin Cancer Res 2012
Several mechanisms responsible for crizotinib
resistance: clinical implications
Doebele et al. Clin Cancer Res 2012
Conclusions
• Different mechanisms are responsible for acquired
resistance to novel targeted therapies
• So far no proven efficacy of irreversible EGFR-TKIs
in NSCLC with acquired resistance to reversible
agents
• No clinically available strategies for crizotinib
resistant patients
• New drugs and new strategies are under
investigation