Challenging Cases in Lung Cancer
advertisement
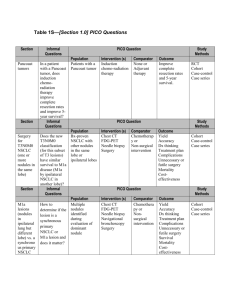
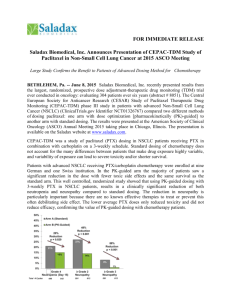
Please note, these are the actual video-recorded proceedings from the live CME event and may include the use of trade names and other raw, unedited content. Select slides from the original presentation are omitted where Research To Practice was unable to obtain permission from the publication source and/or author. Links to view the actual reference materials have been provided for your use in place of any omitted slides. Challenging Cases in Lung Cancer Oncologist and Nurse Investigators Consult on Actual Patients from the Practices of the Invited Faculty Friday, May 2, 2014 6:00 AM – 7:30 AM Faculty Geoffrey R Oxnard, MD Karen L Reckamp, MD, MS Rebecca Lynn Sipples, MSN, APRN, ACNP, AOCNP Alison J Holmes Tisch, MSN, RN, ANP-BP, AOCNP Moderator Neil Love, MD Oncology 6-Part Case Series: Key Themes • Mechanisms of action of novel agents and tissue assays to predict response • Side effects and toxicities of novel agents; dose adjustments • Assessment and management of adherence • Specific goals of therapy and likely outcomes; sequencing of agents in advanced disease • Local and systemic complications of cancer: Fatigue, pain, CNS involvement • Care of older, frail patients and those with comorbidities Oncology 6-Part Case Series: Key Themes • Clinical trials as a means to access new treatments earlier • Management of anxiety and depression • Key determinants of patient satisfaction: What do people with cancer want and need? • Quality, value and cost: Investing resources optimally • End-of-life care and planning • Impact of the cancer experience on family and loved ones, including minor children • Impact of the oncology experience on oncology health professionals Agenda Two Patients with Adenocarcinoma and EGFR Tumor Mutations •54 yo woman with advanced EGFR-mutant NSCLC with progressive disease after responding to erlotinib (Ms Sipples) •36 yo Afghani woman with advanced EGFR-mutant NSCLC currently receiving afatinib/cetuximab (Ms Tisch) A Patient with Metastatic Adenocarcinoma Who Received Front-Line Chemobiologic Therapy Followed by Maintenance •41 yo woman with advanced “pan-wild-type” NSCLC with 2 young children (Ms Tisch) Agenda A Patient Who Received Immunotherapy on a Clinical Trial • 77 yo woman with advanced NSCLC who went on a clinical trial of nivolumab and is currently receiving nanoparticle albumin-bound (nab) paclitaxel (Ms Sipples) Two Patients with Tumor Mutations: ROS1 and HER2 • 70 yo man with advanced, ROS1-mutant NSCLC receiving crizotinib (Ms Sipples) • 64 yo woman with advanced NSCLC with a HER2 insertion who has requested help with assisted suicide (Ms Tisch) Two Patients with Adenocarcinoma and EGFR Tumor Mutations • 54 yo woman with advanced EGFR-mutant NSCLC with progressive disease after responding to erlotinib (Ms Sipples) • 36 yo Afghani woman with advanced EGFR-mutant NSCLC currently receiving afatinib/cetuximab (Ms Tisch) Case 1 (from the practice of Ms Sipples) • A 54-year-old woman was diagnosed 9 months ago with advanced non-small cell lung cancer (NSCLC) (adenocarcinoma with EGFR L858R exon 21 point mutation) and multiple ring-enhancing brain metastases • She responded to erlotinib but then developed progressive disease Discussion Point Incidence of tumor driver mutations in patients with NSCLC; algorithms for tissue testing Incidence of Single Driver Mutations in Metastatic Lung Adenocarcinoma N = 733 Kris MG et al. JAMA 2014;311(19):1998-2006. Discussion Point Selection of first-line therapy for patients with EGFR activating mutations; similarities and differences between erlotinib and afatinib Select Trials of First-Line Treatment with EGFR TKIs vs Chemotherapy in EGFR-Mutant NSCLC Study Treatment N RR, % PFS, mo OS, mo IPASS1,2 Gefitinib vs Carbo/pac 261 71.2 vs 47.3 9.5 vs 6.3 21.6 vs 21.9 NEJ0023 Gefitinib vs Carbo/pac 230 73.7 vs 30.7 10.8 vs 5.4 30.5 vs 23.6 OPTIMAL4,5 Erlotinib vs Carbo/gem 165 83 vs 36 13.1 vs 4.6 22.7 vs 28.9 Erlotinib vs Platinumbased chemo 174 58 vs 15 9.7 vs 5.2 19.3 vs 19.5 EURTAC6 1 Mok TS et al. N Engl J Med 2009;361(10):947–57. 2 Fukuoka M et al. J Clin Oncol 2011;29(21):2866–74. 3 Maemondo M et al. N Engl J Med 2010;362(25):2380–8. 4 Zhou C et al. Lancet Oncol 2011;12(8):735–42. 5 Zhou C et al. Proc ASCO 2012;Abstract LBA7520. 6 Rosell R et al. Lancet Oncol 2012;13(3):239–46. Possible Erlotinib-Associated Side Effects Most Common AEs • Rash • Fatigue • Diarrhea • Appetite loss Afatinib: An Irreversible ErbB Family Blocker EGF ligands Heregulins EGFR inhibitors ErbB Family Blockade EGFR (ErbB1) HER2 (ErbB2) ErbB3 ErbB4 Afatinib is an orally available, irreversible ErbB family blocker, with high efficacy potential • Inhibition of ErbB family receptor heterodimerization • In vitro activity against EGFR-resistant T790M mutation Adapted from Li D et al. Oncogene 2008;27:4702-11. Phase III LUX-Lung 3 Study for Patients with Treatment-Naïve Advanced Lung Cancer Stage IIIB/IV lung adenocarcinoma EGFR mutation in tumor R 2:1 Afatinib Cisplatin + Pemetrexed Primary endpoint: PFS Secondary endpoints: ORR, DCR, DoR, tumor shrinkage, OS, patient-reported outcomes, safety, PK Yang JC et al. Proc ASCO 2012;Abstract LBA7500. LUX-Lung 3: Response and PFS (Independent Review) Afatinib (n = 230) Cis/pem (n = 115) 56% 23% 11.1 mo 6.9 mo Response rate Median progression-free survival Sequist LV et al. J Clin Oncol 2013;31(27):3327-34. Possible Afatinib-Related AEs Most Common AEs • Diarrhea • Rash/acne • Stomatitis/mucositis • Paronychia • Dry skin Sequist LV et al. J Clin Oncol 2013;31(27):3327-34. Discussion Point Mechanisms of resistance to EGFR TKI therapy LUX-Lung 1 Phase IIb/III Study of Afatinib After Failure of Erlotinib, Gefitinib or Both and Chemotherapy • N = 585 patients with Stage IIIB/IV adenocarcinoma of the lung • Afatinib/best supportive care (BSC) vs placebo/BSC • All received prior EGFR TKI and chemotherapy Afatinib Placebo Median OS 10.8 mo 12.0 mo Median PFS 3.3 mo 1.1 mo 7% <1% ORR No complete responses Miller VA et al. Lancet Oncol 2012;13(5):528-38. Phase II Study of Afatinib/Cetuximab • EGFR mutant • Advanced NSCLC Afatinib + Cetuximab • Progressing on erlotinib or gefitinib • N = 100 ORR: 30% Median PFS: 4.7 mo Median DoR: 8 mo Grade 3 Rash: 18% Grade 3 Diarrhea: 7% Janjigian YY et al. Proc ESMO 2012;Abstract 1227O. Afatinib + cetuximab at MTD: Responses by T790M mutation Maximum percentage decrease from baseline (%) T790M+ T790M– EGFR wt Uninformative for T790M 50 40 30 20 10 0 –10 –20 –30 –40 –50 –60 –70 –80 –90 –100 –110 0 5 10 15 20 25 30 35 40 45 50 55 60 65 70 75 80 85 90 95 100 Patient index sorted by maximum % decrease With permission from Janjigian YY et al. Proc ESMO 2012;Abstract 12007O. Best Response Rates T790 Mutation Status T790M+ (n = 53) T790M(n = 39) Total (n = 96) Clinical benefit rate 81% 64% 75% Median duration of response 6.4 mo 9 mo 8 mo Response Janjigian YY et al. Proc ESMO 2012;Abstract 12007O. Case 2 (from the practice of Ms Tisch) • A 36-year-old Afghani woman was initially diagnosed in June 2005 with bronchoalveolar carcinoma that has since been categorized as adenocarcinoma with lepidic features • The patient’s disease has progressed through multiple treatments including chemotherapy, erlotinib, bevacizumab and 2 clinical trials, one of a single-agent investigational tyrosine kinase inhibitor (TKI) and one of erlotinib combined with cabozantinib • She was later enrolled on a clinical trial of CO-1686 and experienced a life-threatening tumor flare reaction after discontinuation of the drug, which was reversed by restarting erlotinib • She is currently receiving cetuximab and afatinib • The patient is a married mother of young children • Her Muslim faith plays a strong role in her desires concerning possible future end-of-life care Progressive Disease on a Trial of CO-1686 Partial Response After Retrial with Erlotinib Progressive Disease After Retrial of Erlotinib Partial Response to Cetuximab and Afatinib CO-1686 • Mutation-specific TKI targeting activating mutations and T790M • Theoretically offers key advantage by not inhibiting wild-type EGFR • 45 2nd-line TKI patients, 74% T790M+ • Notably absent was rash and diarrhea • Clinical responses have been observed in 3 of 4 patients who received the highest dose • Phase II and III studies are under development Soria JC et al. Proc WCLC 2013;Abstract O03.06. Skin Rash from Tyrosine Kinase Inhibitors • Most frequent dermatologic side effect reported is acneiform eruption. • Affects mainly face, upper chest and/or back. • Also known as acne, acneiform skin reaction/rash, follicular rash and maculopapular skin rash. Ricciardi S et al. Clin Lung Cancer 2009;10(1):28-35. Clinical Grades of Erlotinib-Induced Rash • Mild – Generally localized papulopustular reaction – Minimally symptomatic – No impact on daily activities – No sign of superinfection • Moderate – Generalized papulopustular reaction – Mild pruritus or tenderness – Minimal impact on daily activities – No sign of superinfection • Severe – Generalized papulopustular reaction – Severe pruritus or tenderness – Significant impact on daily activities – Potential for or has become superinfected Saif MW et al. JOP 2008;9(3):267-74. Case 3 (from the practice of Ms Tisch) • A 41-year-old woman was diagnosed in 2010 with a Stage IIIA adenocarcinoma that was treated with cisplatin/pemetrexed followed by right upper lobectomy and then consolidative chemoradiation therapy • In 2011 she experienced systemic disease recurrence and was started on carboplatin/paclitaxel/bevacizumab followed by maintenance bevacizumab • The patient is married with 2 young children 2011: Systemic Disease Recurrence Response to Carboplatin/Paclitaxel/Bevacizumab Prior to Maintenance Therapy Discussion Point Systemic treatment of metastatic “pan-wild-type” NSCLC: Choice of chemotherapy regimen and role of bevacizumab Chemotherapeutic Regimens Commonly Employed in the Front-Line Management of Metastatic Pan-Wild-Type NSCLC • Carboplatin/paclitaxel ± bevacizumab • Carboplatin/nab paclitaxel ± bevacizumab • Carboplatin/pemetrexed ± bevacizumab • Cisplatin/chemotherapy ± bevacizumab NCCN NSCLC Clinical Practice Guidelines v 3.2014 ECOG-E4599: Bevacizumab in Nonsquamous NSCLC Paclitaxel/carbo platin/bevacizum Paclitaxel/carbo ab platin (n = 443) (n = 444) Median progression-free survival (PFS) 6.2 months 4.5 months Median overall survival (OS) 1-yr OS 2-yr OS 12.3 months 51% 23% 10.3 months 44% 15% Sandler A et al. N Engl J Med 2006;355(24):2542-50. Discussion Point Recognition and management of hypertension and proteinuria with bevacizumab; risk of cardiovascular events Discussion Point Maintenance strategies in NSCLC: biologic therapy, chemotherapy or both What Is Maintenance Therapy? • Use of systemic therapy following 1st-line therapy, for patients with CR/PR/SD, before documentation of progression – Continuation of a targeted agent – Continuation of one of the agents used in the 1st-line combination regimen – Switch to a new agent after 1st-line therapy Rogerio C Lilenbaum, MD, Winter Lung Cancer Conference 2014 PointBreak: Phase III Trial Design Induction Phase Maintenance Phase Pemetrexed + Carboplatin + Bevacizumab Pemetrexed + Bevacizumab Inclusion: - No prior systemic therapy for lung cancer - PS 0/1 - Stage IIIB-IV NS-NSCLC - Stable tx’t brain mets Exclusion: - Peripheral neuropathy ≥Grade 1 - Uncontrolled pleural effusions R Paclitaxel + Carboplatin + Bevacizumab Patel JD et al. J Clin Oncol 2013;31(34):4349-57. Bevacizumab ECOG-E5508: A Phase III Study of Maintenance Bevacizumab, Pemetrexed or the Combination in Advanced NSCLC Target Accrual: 1,282 Study is currently recruiting participants Study Start Date: August 2010 Maintenance therapy Eligibility Bevacizumab • Stage IIIB/IV nonsquamous NSCLC • No brain metastases • Stable or better response after 4 courses of carbo, paclitaxel and bev R Pemetrexed Bevacizumab + Pemetrexed Primary Endpoint: Overall survival Induction therapy: Carboplatin, paclitaxel and bevacizumab www.clinicaltrials.gov, May 2014 Case 4 (from the practice of Ms Sipples) • A 77-year-old woman diagnosed in 1982 with earlystage NSCLC experienced disease recurrence in the right upper lobe in 2011, for which she underwent a segmentectomy followed by adjuvant cisplatin/pemetrexed • Her disease recurred in May 2012, at which time she received carboplatin/gemcitabine • After further disease progression, in April 2013 she was enrolled on a clinical trial of an immune checkpoint inhibitor but 2 months later developed brain metastases, which were resected • Since June 2013 she has been receiving nab paclitaxel 3 out of 4 weeks and has responded well but has developed neuropathy within the past month Discussion Point Adjuvant therapy for NSCLC: Choice of platinum doublet in older patients Discussion Point Available data with nab paclitaxel in lung cancer Phase III Nab P/C vs P/C Study Design Chemo-naïve PS 0-1 Stage IIIb/IV NSCLC N = 1,052 Nab Paclitaxel 100 mg/m2 d1, 8, 15 Carboplatin AUC 6 d1 q3wk No Premedication n = 521 1:1 Stratification factors: • Stage (IIIb vs IV) • Age (<70 vs >70) • Histology (squamous vs nonsquamous) Socinski MA et al. J Clin Oncol 2012;30(17):2055-62. Paclitaxel 200 mg/m2 d1 q3wk Carboplatin AUC 6 d1 q3wk With Premedication of Dexamethasone + Antihistamines n = 531 Common Treatment-Related ≥Grade 3 Adverse Events Nab Paclitaxel (n = 514) Standard Paclitaxel (n = 524) Adverse event Grade 3 Grade 4 Grade 3 Grade 4 p-value Neutropenia 33% 14% 32% 26% <0.001 Thrombocytopenia 13% 5% 7% 2% <0.001 Anemia 22% 5% 6% <1% <0.001 Sensory neuropathy 3% 0% 11% <1% <0.001 Socinski MA et al. J Clin Oncol 2012;30(17):2055-62. Objective Responses by Histology Squamous P < 0.001 P = 0.060 Nonsquamous P = 0.808 P = 0.069 Percent Responses Nab P/C P/C n = 228 n = 221 Socinski MA et al. J Clin Oncol 2012;30(17):2055-62; Socinski MA et al. ASCO 2010;Abstract 7511. n = 292 n = 310 Response and Survival in Elderly Patients (≥70) Nab P/C (n = 74) P/C (n = 82) Overall response rate 34% 24% Median progression-free survival 8 mo 6.8 mo 19.9 mo 10.4 mo Endpoint Median overall survival Adverse events similar in both groups • Nab paclitaxel - Less neuropathy - Less neutropenia - Less arthralgia - More anemia Socinski MA et al. Ann Oncol 2013;24(2):314-21. Discussion Point Anti-PD-1 and anti-PD-L1 antibodies: Mechanisms of action, predictors of response, time sequence of antitumor benefit, side effects and toxicities Role of PD-1 in Suppressing Antitumor Immunity Patient’s T cells Tumor cell MHC TCR T cell PD-1 PD-L1 B7.1 MHC T-cell blockade T cells TCR Tumor cell growth PD-1 PD-L1 Engineered Fc-domain B7.1 T-cell activation + Anti-PD-L1 Granzymes and perforin Tumor cell death • Blocking PD-L1 restores T-cell activity, resulting in tumor regression in preclinical models • Binding to PD-L1 leaves PD-1/PD-L2 interaction intact and may enhance efficacy and safety Adapted from Spigel et al. Proc ASCO 2013;Abstract 8008. Activity of Nivolumab in Patients with Treatment-Refractory Cancer • Two patients with lung cancer who received 10 mg/kg of nivolumab experienced unconfirmed responses, and 8 additional patients with melanoma, lung cancer or renal cell cancer had a persistent reduction in baseline target lesions in the presence of new lesions, a finding consistent with an immune-related response pattern. • In patients with lung cancer, 14 objective responses were observed. • All 14 patients with objective responses started treatment 24 weeks or more before data analysis, and 8 of these patients had a response that lasted 24 weeks or more. Five of 14 patients with objective responses started treatment 1 year or more before data analysis, 2 of whom had a response that lasted 1 year or more. Stable disease lasting 24 weeks or more was observed in 5 patients with lung cancer. Topalian SL et al. N Engl J Med 2012;366(26): 2443-54. Clinical Development of Inhibitors of PD-1 Immune Checkpoint Target PD-1 PD-L1 Antibody Molecule Development stage Nivolumab (BMS936558/MDX1106/ONO-4538) Fully human IgG4 mAb Phase II multiple tumors Pidilizumab (CT-011) Humanized IgG1 mAb Phase II multiple tumors Lambrolizumab (MK3475) Humanized IgG4 mAb Phase I AMP-224 B7-DC/IgG1 fusion protein Phase I MDX-1105/BMS936559 Fully human IgG4 mAb Phase I Giaccone G. Proc ASCO Clinical Science Symposium. Two Patients with Tumor Mutations: ROS1 and HER2 • 70 yo man with advanced, ROS1-mutant adenocarcinoma of the lung receiving crizotinib (Ms Sipples) • 64 yo woman with advanced NSCLC with a HER2 insertion (Ms Tisch) Case 5 (from the practice of Ms Sipples) • A 70-year-old man with a history of Stage IIB lung adenocarcinoma treated in 2006 with resection and adjuvant cisplatin/vinorelbine experienced local recurrence 4 years ago and received chemoradiation therapy • In 2013 the patient developed biopsy-confirmed metastatic lung adenocarcinoma positive for ROS1 mutation • He is currently receiving crizotinib but experienced acute renal injury that led to a treatment interruption • The patient is married and is well known by the medical staff because his daughter was a patient for breast cancer in the past Discussion Point ALK and ROS tumor rearrangements: Indications for testing EML4-ALK and ROS1 Alterations in NSCLC EML4-ALK alterations1 • In ~4% of NSCLC cases • Enriched in younger, never or light smokers with adenocarcinoma • Rarely overlaps with EGFR and K-ras mutations ROS1 alterations2-3 • In ~1% of NSCLC cases • Enriched in younger, never or light smokers with adenocarcinoma • No overlap with other oncogenic drivers 1 Soda M et al. Nature 2007;448(7153):561-6; 2 Bergethon K et al. J Clin Oncol 2012;30(8):86370; 3 Takeuchi K et al. Nat Med 2012;18(3):378-81. ALK Rearrangement in Cancer • Chromosomal translocation most common ALK abnormality in cancer • Rearrangement of genetic info when parts of one chromosome break off and fuse with another or flip around (inversion) • Results in new gene and expression of fusion protein Cancer Genome Atlas, National Cancer Institute Discussion Point Efficacy of crizotinib in patients with ALK and ROS rearrangements; unique toxicities associated with crizotinib: Vision abnormalities, hypogonadism Activity of Crizotinib in ALK+ NSCLC Update of the Phase II Study Variable (n = 259) Crizotinib 250 mg, n (%) Objective response rate 155 (59.8) Complete response 4 (1.5) Partial response 151 (58.3) Stable disease 69 (26.6) Objective progression 19 (7.3) Kim DW et al. Proc ASCO 2012;Abstract 7533. FDA NEWS RELEASE April 29, 2014 “The US Food and Drug Administration today granted accelerated approval to ceritinib for patients with a certain type of late-stage (metastatic) non-small cell lung cancer (NSCLC). “Ceritinib is an anaplastic lymphoma kinase (ALK) tyrosine kinase inhibitor that blocks proteins that promote the development of cancerous cells. It is intended for patients with metastatic ALK-positive NSCLC who were previously treated with crizotinib, the only other approved ALK tyrosine kinase inhibitor.” www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm395299.htm Ceritinib (LDK378) Induces Responses in the Majority of Crizotinib-Resistant Patients • A total of 114 patients with NSCLC received at least 400 mg of ceritinib daily • Overall response rate (ORR) was 58% • Confirmed complete response: 1(1%) • Confirmed partial response: 65 (57%) • The majority of patients with NSCLC who received ceritinib had previously received crizotinib: 83/122 (68%) • Among patients who previously received crizotinib, ORR = 56% • Among patients who had not received crizotinib previously and who received ceritinib at ≥400 mg daily, ORR = 21/34 (62%) Shaw AT et al. N Engl J Med 2014;370(13):1189-97. Typical Responses to Ceritinib (LDK378) • In the Phase I study of ceritinib in ALK-rearranged NSCLC, some patients experienced rapid responses to crizotinib. – In one patient with crizotinib-resistant disease, the comparison of positron emission tomography scans taken at baseline and 3.5 weeks of ceritinib treatment was dramatic. – Subsequent computed tomography scans after 6 weeks of ceritinib treatment showed a 52% reduction in tumor burden in this patient. Shaw AT et al. N Engl J Med 2014;370(13):1189-97. Case 6 (from the practice of Ms Tisch) • A 64-year-old woman diagnosed with Stage IIIA NSCLC underwent treatment with neoadjuvant chemotherapy followed by resection and chemoradiation therapy • Six months later metastases were detected • The patient’s disease progressed on several lines of therapy, and interim mutational testing revealed a HER2 insertion • She began treatment with vinorelbine/trastuzumab and had a significant clinical response and prolonged benefit but ultimately experienced clinical worsening and entered hospice • The patient repeatedly asked for help with assisted suicide, which she planned to use near the time of her death so that she would not suffer Pre- and Post-vinorelbine and trastuzumab treatment Prior to treatment Post treatment HER2 in Lung Cancers Agents Targeting HER2 Amplification and Protein Expression • • • • Trastuzumab Pertuzumab Lapatinib Ado-Trastuzumab Emtansine Trials of Investigational Agents Targeting HER2 Mutations • • • • Dacomitinib Afatinib Neratinib Neratinib + Temsirolimus Discussion Point Role of multiplex testing to identify other lung cancer mutations: Implications for clinical trial referral and nonprotocol care Options for Molecular Profiling • Actionable Analysis (EGFR, ALK, ROS) • SNaPshot (Iafrate MGH) – Genotyping of approx 100 key mutations • Extensive Mutation Analysis of COSMIC Genes – Foundation Medicine 400 – Sklar 409 • Whole Exome Sequencing (23,000 genes) • Whole Genome Sequencing