Sepsis: Clinical Spectrum and Management
advertisement
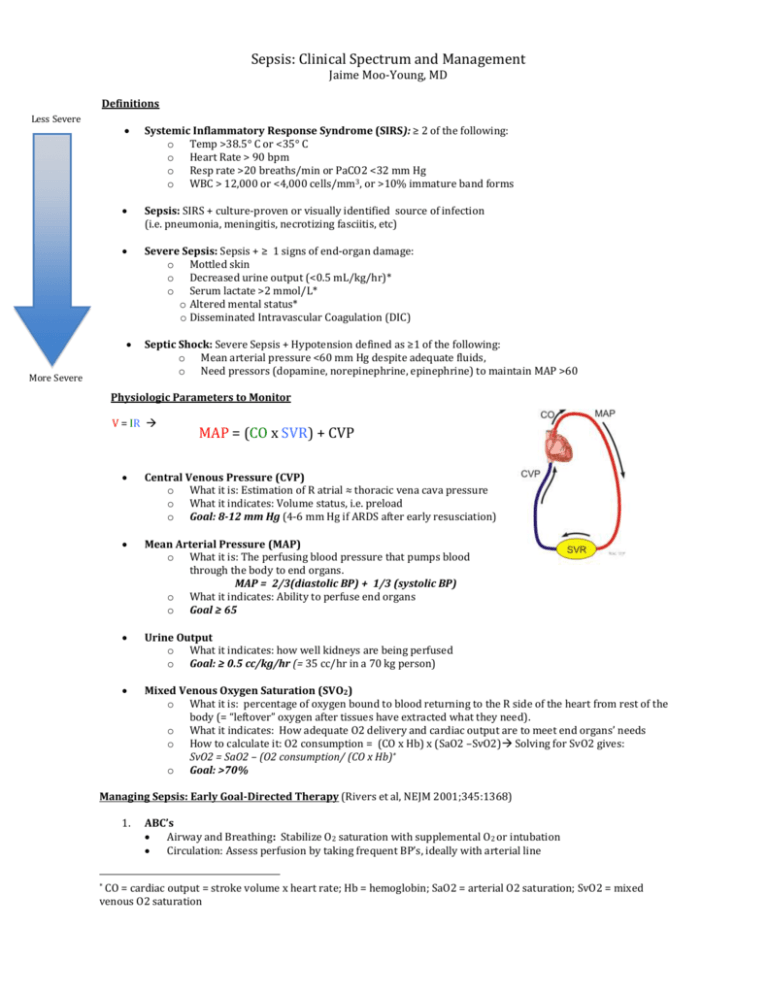
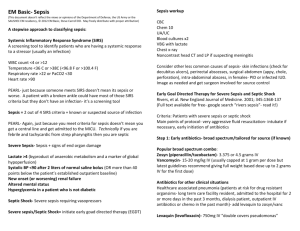
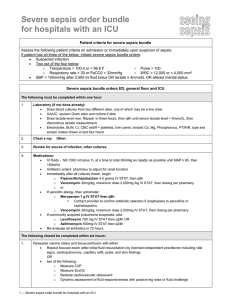
Sepsis: Clinical Spectrum and Management Jaime Moo-Young, MD Definitions Less Severe Systemic Inflammatory Response Syndrome (SIRS): ≥ 2 of the following: o Temp >38.5° C or <35° C o Heart Rate > 90 bpm o Resp rate >20 breaths/min or PaCO2 <32 mm Hg o WBC > 12,000 or <4,000 cells/mm3, or >10% immature band forms Sepsis: SIRS + culture-proven or visually identified source of infection (i.e. pneumonia, meningitis, necrotizing fasciitis, etc) Severe Sepsis: Sepsis + ≥ 1 signs of end-organ damage: o Mottled skin o Decreased urine output (<0.5 mL/kg/hr)* o Serum lactate >2 mmol/L* o Altered mental status* o Disseminated Intravascular Coagulation (DIC) More Severe Septic Shock: Severe Sepsis + Hypotension defined as ≥1 of the following: o Mean arterial pressure <60 mm Hg despite adequate fluids, o Need pressors (dopamine, norepinephrine, epinephrine) to maintain MAP >60 Physiologic Parameters to Monitor V = IR MAP = (CO x SVR) + CVP Central Venous Pressure (CVP) o What it is: Estimation of R atrial ≈ thoracic vena cava pressure o What it indicates: Volume status, i.e. preload o Goal: 8-12 mm Hg (4-6 mm Hg if ARDS after early resusciation) Mean Arterial Pressure (MAP) o What it is: The perfusing blood pressure that pumps blood through the body to end organs. MAP = 2/3(diastolic BP) + 1/3 (systolic BP) o What it indicates: Ability to perfuse end organs o Goal ≥ 65 Urine Output o What it indicates: how well kidneys are being perfused o Goal: ≥ 0.5 cc/kg/hr (= 35 cc/hr in a 70 kg person) Mixed Venous Oxygen Saturation (SVO2) o What it is: percentage of oxygen bound to blood returning to the R side of the heart from rest of the body (= “leftover” oxygen after tissues have extracted what they need). o What it indicates: How adequate O2 delivery and cardiac output are to meet end organs’ needs o How to calculate it: O2 consumption = (CO x Hb) x (SaO2 –SvO2) Solving for SvO2 gives: SvO2 = SaO2 – (O2 consumption/ (CO x Hb)* o Goal: >70% Managing Sepsis: Early Goal-Directed Therapy (Rivers et al, NEJM 2001;345:1368) 1. ABC’s Airway and Breathing: Stabilize O2 saturation with supplemental O2 or intubation Circulation: Assess perfusion by taking frequent BP’s, ideally with arterial line CO = cardiac output = stroke volume x heart rate; Hb = hemoglobin; SaO2 = arterial O2 saturation; SvO2 = mixed venous O2 saturation * 2. Fluid resusciation of circulation Isotonic crystalloid (NS or Lactated Ringer’s) as good as albumin Goals: get lactate <2, CVP >8, MAP ≥65, urine output ≥ 0.5 cc/kg/hr Most important step of sepsis mangament! May require >5L within first 6 hrs Do not delay fluids to determine infection source or place a line 3. Determine and Control Infection source Blood cultures x 2 sets, ideally before starting ABX Start empiric antibiotics within 1 hour of recognized sepsis o Use broad-spectrum (gram +, gram -) if source not immediately obvious o Consider fungemia in immunosuppressed pts o Avoid using 2 antibiotics from the same class (i.e. B-lactams) o Take pt’s allergies, antibiotic history, and resistance patterns into account Get urine cultures and CXR unless alternative source is obvious If evidence of sequestered infection (i.e abscess), drain it. 4. Determine and manage Volume status Insert central venous catheter where available, and transduce CVP. Surrogates for CVP: 1) Bedside ultrasound to estimate internal jugular filling pressure; 2) physical exam to estimate JVPgive fluids until JVP ≥ 8 If CVP <8 and MAP still ≤ 65, give more fluids until CVP at goal. If CVP >12 and MAP <65, start vasopressors If cannot measure JVP or CVP, minimal adequate fluid resusciation = 40-60 mL/kg of isotonic fluid 5. Start vasopressors if indicated. First line = norepinephrine. Preferred to dopamine due to arrhythmogenic effects Second line: May add vasopressin to norepi, but no data to show improved outcomes 6. Determine and manage tissue perfusion. Measure ScVO2 via central line Surrogates for ScVO2: 1) SvO2 from VBG; 2) Hemoglobin measurement Goal >70% If <70%, consider blood transfusion to goal Hb of 7 If cannot measure ScVO2 exactly, try to optimize SaO2, Hb, and CO Be cautious with blood transfusions, as can increase risk of ARDS * Time frame = within 6 hours for all the above steps. Shown to mortality by >40% !!** Adjuncts to Early Goal-directed Therapy Steroids: o Data to support corticosteroid administration in fluid and pressor-refractory shock is conflicting. o May transiently improve blood pressures but lead to more superinfection. Glycemic Control: o Data to support aggressive glycemic control to 80-110 mg/dL is controversial. o Risk of overly aggressive glycemic control can lead to hypoglycemic episodes and/or mortality risk o May consider keeping glucose <150 mg/dL Key Points The progression of SIRS to septic shock occurs along a continuum. Learn how to recognize the warning signs of SIRSseptic shock early so that you can intervene ASAP. When in doubt, give fluids early and generously (within 6 hours is key). Attaining hemodynamic goals within 6 hours can reduce mortality by >40%. Do not delay empiric antibiotics to place lines, draw cultures, or obtain other diagnostic data. In the absence of high-technology monitoring, physical exam findings are your friend. References: 1. Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 2001; 345:1368. 2. www.uptodate.com 3. Sabatine et al. Pocket Medicine, Fourth Edition. Wolters Kluwer, Lippincott Williams & Wilkins, 2010. 4. McGee, Steven. Evidence Based Physical Diagnosis. Philadelphia: Saunders, 2007.