Management of children with CKD in a DGH 2
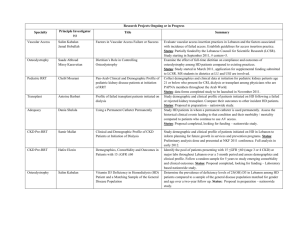
advertisement

Management of children with CKD in a DGH M Shenoy Consultant Paediatric Nephrologist RMCH Nephrology for the General Paediatrician Meeting Manchester CKD in a DGH • CKD • Tubulopathy • Peritoneal dialysis • Renal transplant recipient CKD eGFR Calculation • Schwartz formula 40 * ht (cm)/Pcreatinine Schwartz GJ, Haycock GB et al Pediatrics 1976 1. Child with CKD Stage III • 4 yr old, male child • Diagnosed to have dysplastic kidneys • Creatinine 95umol/l (eGFR 42ml/min/1.73m2) • Medications: Enalapril, one aphacalcidol • Admitted with febrile illness, poor intake • Diagnosis: Tonsillitis • Creatinine 144umol/l, eGFR now 27ml/min/1.73m2 What are the possible reasons for deterioration in kidney function in this child? • Infection • Dehydration • Medications – Captopril – Ibuprofen Management • Prevent dehydration • Omit ACEi during episodes of dehydration • Avoid nephrotoxic drugs – NSAID’s – Gentamicin, vancomycin, aciclovir • Adjust drug dose for eGFR Tubulopathy • RTA – Proximal • Cystinosis • Drug induced • Bartter syndrome • Nephrogenic DI 2. Child with tubulopathy • 12 year old boy with cystinosis • Admitted for tonsillectomy • Pre-op bloods – Na 134, K 3.5, HCO3 19, U 4.2, Cr 124, Ca 2.4, PO4 1.1 • Post op bloods – Na 136, K 2.8, HCO3 11, U 7.8, Cr 210, Ca 2.3, PO4 0.7 Tubulopathy • Fluids: not ‘maintenance’ • Continue regular medications and electrolyte supplements • Need 8-12 hourly bloods • Avoid nephrotoxic drugs Dialysis • Around 30 children on dialysis – Home PD 20, 6-7 nights/week – In centre 3-4/week HD 10 • Oliguric and non-oliguric • Dialysis access 3. Child on PD • 12 year old girl on PD, anuric • Admitted with abdominal pain • Mother reports cloudy effluent Fluids in an anuric child • Ask how much is their fluid allowance • Usually 600 – 1000ml/day • Excess fluids leads to hypertension and need for more dialysis Complications of PD catheter • Peritonitis – < 1 episode/14 patient months averaged over 3 years – Diagnosis: PD fluid WCC >100 – Treated with IP antibiotics for 2 weeks • Exit site infection • Catheter migration • Catheter blockage Renal Transplant • UK 125 paediatric transplants per year – Manchester ~15 • 75% living donor • ~60 children attending transplant clinic Renal transplant • Immunosuppression – Used to be ciclosporin, azathioprine and prednisolone – Now tacrolimus and mycophenolate mofetil Graft survival following first paediatric kidney only transplant 100 90 % g r a ft s u r v iv a l 80 70 5 yr survival 60 50 10 yr survival 20 yr survival 48 (38 - 58) p<0.0001 Living (n=714) 88 (85 - 91) p<0.0001 71 (65 - 76) p<0.0001 DBD 72 (70 - 74) 59 (57 - 61) 40 30 (n=2009) 20 10 0 0 5 10 15 years post-transplant 20 37 (33 - 40) Am J Transplant 2004; 4: 384-389 4. Child with kidney transplant • 6 year old boy with kidney transplant 2 years back • Admitted with febrile illness • Bloods: – Creat 135 (usually ~60) Reasons for reduced graft function • Infection – Bacterial, viral, PTLD • Rejection – Late rejection, usually compliance issues • Drug toxicity – Tacrolimus, NSAIDs • Obstruction Summary • Child with CKD – Attention to fluid balance and electrolytes – Avoid drug toxicity – Dialysis access is precious – Infection, rejection and drug toxicity in a transplant recipient – Discuss with Nephrologist