Renal Disease and Dialysis
advertisement
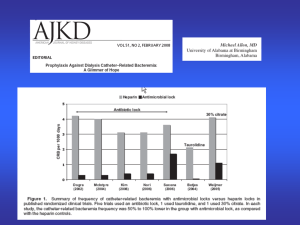
Renal Disease and Dialysis 101 Shalini Bumb August 2013 Objectives CKD Dialysis Access Eckel pearls Scenarios Chronic Kidney Disease Types of dialysis 1. 2. 3. 4. Hemodialysis (HD) Ultrafiltration (UF) Continuous Veno-Venous hemofiltration (CVVH) Peritoneal Dialysis Hemodialysis Semipermeable membrane Solute removal via passive diffusion ◦ Inversely proportional to the size (ie effective removal of K, urea, C; not of PO4) Ultrafiltration use of hydrostatic pressure gradient to induce convection (filtration of water) solvent drag (pulls dissolved solutes) across removal of excess fluid CVVH highly permeable membrane fluid and solute removal via ultrafiltration filtrate is discarded replacement fluid is infused similar to plasma (but no K, urea, Cr, PO4) used in ICU, runs 12-24h, through double lumen catheter less drastic fluid shifts Peritoneal Dialysis peritoneal membrane = partially permeable membrane dextrose dialysate diffusion and osmosis until equilibrium 3-10 dwells per night with 2-2.5 L per dwell Indications for Dialysis Acidosis Electrolytes Ingestions Overload Uremia Access Arteriovenous fistula (AVF) Graft Tunneled catheter Arteriovenous Fistula ◦ Highest patency ◦ Lowest risk of infection ◦ Low risk of thrombus ◦ Maturation time (3-4mo) ◦ Steal syndrome (poor blood supply to the rest of the limb) ◦ Aneurysm formation Arteriovenous Graft Easier to create Maturation time 3-6 weeks Poor patency (often requires thrombectomy or angioplasty) Infection Aneurysms Steal syndrome Tunneled Catheter Immediate use Bridge to AVF/AVG Poor flow (decreased HD efficiency) High infection risk Venous stenosis Thrombosis Dialysis Rx: Time: 2-5 hours Bath Blood flow rate: 400-450cc/min Dialysate flow rate: 500-800cc/min Anticoagulant Additives: ◦ Anemia (EPO, blood) ◦ Bone metabolism (vit D, calcitriol, etc) ◦ Meds (antibiotics) Dialysate Bath Common Admissions on Eckel Complications of missed HD ◦ SOB from fluid overload ◦ HTN crisis ◦ Hyperkalemia Line infections Access issues And everything else… Eckel Pearls: presentation 75 yo AAM with ESRD 2/2 DM (HD MWF via RUE AVF, at CDC East, nephrologist Dr. Wish, dry weight 82kg, oligouric) Eckel Pearls: history how did the last HD session go? complications since being started on HD? ◦ infections? ◦ multiple access points? medically compliant? get run sheets from dialysis center Eckel Pearls: physical exam Vitals: no BP in the arm of the access Volume status Access: ◦ Infection? ◦ Aneurysms ◦ Bruits/thrills Page 1 RN LK50: OMG’s K is 3.1. Can we replete? •Had dialysis 3rd shift. Finished 2hrs ago Labs in ESRD Get labs before or 4h after HD Only the H/H is accurate Floor RNs can’t use HD lines Can ask to have cultures drawn at HD from the line Page 2 RN LK20: New admit AMS on floor. Hard to arouse. Please eval ED presentation with abd pain Workup initiated since there are no beds… Pain meds: morphine 1mg, then 1mg, then 2 mg, then 3mg IVP Sent to the floor Medications in ESRD Antibiotics ◦ Renally dose ◦ Loading dose, then maintenance dose No lovenox dvt ppx, use heparin No morphine ◦ Hepatic metabolism – but active metabolites ◦ Limit the other opioids Dilaudid: hepatic metabolism – but metabolites can cause neuroexcitiation constipation/GERD : avoid magnesium/phosphate containing agents Page 3 RN: new admit OK. Called wound care for leg. After lunch you walk on over to the patient room. ESRD admitted for access. OK is doing ok. Vitals stable. Comfortable. Calciphylaxis Calcinosis cutis Page 4 RN LK20: Code white, WAA is hypoxic, 83% on RA. Now 92% on VM. Acutely SOB. Looks uncomfortable. Your co-NF points that one leg is bigger than the other. You ask, “have you had a blood clot before?” WAA nods yes. Hmmm….amongst other things, CTPE? Imaging in CKD Avoid contrast in CKD patients If you have to, prep ◦ volume expansion: isotonic IVFs 3 cc/kg x 1h before 1cc/kg x 6h after ◦ ? alkalinization: sodium bicarbonate ◦ ? acetylcysteine ◦ radiology can give you the protocol (treat empirically) Imaging in ESRD CT with contrast is ok MRI with gadolinium is NOT: ◦ Nephrogenic Systemic Fibrosis (NSF) ◦ IF you must: HD x 3 over 3 consecutive days, with the first right after Page 5 RN LK20: Lost access on GRR. Can you order a PICC? Finally, an easy question. CKD. Sure, why not? Access in CKD Avoid PICC/midlines in CKD stage 4-5 Try to preserve access Try for the feet/EJ But if you need to, order a midline PCP should refer CKD stage IV to nephrologists in anticipation of HD Don’t treat them lightly The end. Resources UpToDate Lavinia Negrea. “Dialysis Access.” Microsoft Powerpoint. August 2013. Claire Sullivan. “Intern Boot Camp: Renal Disease and Dialysis (ie surviving Eckel).” Date last modified 2012. Microsoft Powerpoint. August 2013. Van Stone, JC. Hemodialysis: Hemodialysis apparatus. In: Handbook of Dialysis Daugirdas, JT, Ing, TS (Eds), Little, Brown, Boston, 1994. p53. Yassine Mrabetis. “Hemodialysis Diagram." Online image. Dialysis Definition. Creative Commons Attribution-Share Alike 3.0, Wikepedia. August 2013. “Peritoneal Dialysis Diagram.” Online Image. Alniche: Types of Dialysis. Alniche Life Sciences Pvt. Ltd. August 2013. Po Ming Teng. “Aneurysm.” Online Image. Chronic renal failure and dialysis. Surgical-tutor.org.uk. August 2013. “Calciphylaxis.” Online Image. The UK Calciphylaxis Study. The Renal Association. August 2013. Jonathan Z. Li and William Huen. “Calciphylaxis with Arterial Calcification.” Online Image. 2007. N Engl J Med. August 2013. Shaofeng Yan. “Calciphylaxis Histology.” Online Image. 2006. Mihm’s Dermatopathology: Calciphylaxis. Martin C. Mihm, Jr. August 2013. “Nephrogenic Systemic Fibrosis.” Online Image. Skin & Allergy News: Nephrogenic Fibrosis Is Tied to Contrast Agents : Moderate- to end-stage renal disease patients are most susceptible to the scleroderma-like syndrome. International Medical News Group, LLC. August 2013. Michael Shaw. “They’re willing to throw in their kidneys.” Online image. 2008. New Yorker Cartoon. August 2013. Cartoons from www.lightersideofdialysis.com. August 2013.