NEW APHTA APHFTA (From Association of Private Hospitals in
advertisement

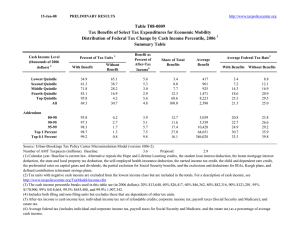
PRIVATE HEALTH SECTOR FOR QUALITY HEALTH CARE PRIVATE HEALTH SECTOR Trusted Partner in the delivery of Quality Healthcare Dr. Samwel Ogillo Program Manager Association of Private Health Facilities in Tanzania APHFTA 1 APHFTA- Association of Private health Facilities in Tanzania Established in 1994 Advocacy and Private Health Sector Development 500+ member facilities- All types of health service delivery Secretariat- Headquarters and 3 zonal offices 0ver 35 full time employed full time professional staff Projects: HIV/AIDS, NCD, FP, QI, Finance/Loans others Partner with MoHSW and DPs 2 Why include the private sector?: 1. Provides about 50% of basic health care in Africa - There is now convincing evidence that the private health sector provides more than 50% of basic health care in many African countries - The role of licensed drug store as a first point of care in many African countries is usually underestimated Role of the Private Sector Survey between 1995-2006 Urban and rural population receiving care from private for-profit provider of modern medicine Percent* 67 64 61 51 53 48 45 48 45 46 45 44 39 34 26 21 21 17 12 11 Source: WB Africa Development Indications 2006, team analysis 7 6 6 2 Average for 11 available SSA countries Why include the private sector?: 2. Many poor in the community access services from the Private facilities (WB & IFC study 2005) 3. Public health sector finances less than half of total health expenditure. Most is financed from out-of-pocket (WB & IFC study 2005) Percent lowest quintile receiving care from private for-profit provider Lowest quintile Highest quintile Lowest quintile Highest quintile 48 53 39 21 Cameroon Uganda Ghana Nigeria Ethiopia Kenya Uganda Nigeria 44 48 48 46 45 34 26 Most recent survey year available between 1995-2006 Source:WB Africa Development Indications 2006, team analysis 45 45 21 39 26 17 21 Cameroon 44 51 Average for Ghana 11 available SSA countries 45 48 Sierra Leone 53 61 Ethiopia 61 Madagascar 51 67 64 Kenya 67 64 Why include the private sector?: 4. The private sector already provides a significant amount of public health services - Most services are provided for free, though some authorities reluctant to go into any formal arrangement/ contract - Governments, NGOs are willing to join hands with Private Sector to serve better 4. The private health sector already plays an important role in the delivery of public health goods (The Dar Example) # PUBLIC AND PRIVATE HEALTH FACILITIES IN DAR- Free Public Services in 2007 (Source - DMO’s office) DISTRICT VACCINATION/ TB & Leprosy MNCH HIV/AIDS SERVICES Public Private Public Private Public Private TEMEKE 29 54 3 3 29 9 ILALA 21 34 18 8 22 19 KINONDONI 33 50 27 16 25 15 83 138 (38%) (62%) 48 27 (64%) (36%) 76 43 (64%) (36%) Why include the private sector?: 5. “The Private Health Sector can have a positive impact on the quality of care- and in many notable cases it is setting the benchmark for higher quality”- in a number of developing countries- IFC study- 2007 - - Modern Medical Technology- CT Scans, MRI, Heart Surgery, Advanced Surgery etc HIV/AIDS- ARVs first delivered by private health sector No question about high quality of care by private facilities compared to public in many countries 9 Barriers to achieving more 1. Lack of access to credit Lack of access to affordable Financing (Results in High Interest Rates by financial institutions) Situation worsened by Lack of policies that encourage investment in rural and sub-urban areas (No special incentives that encourage investing in such areas, e.g. tax relief) Barriers to achieving more 2. Unnecessary competition with NGOs and public sector Lack of planning means that public, private and NGO end up competing for the same clients, while in other areas there are no providers at all Situation worsened by DP money 11 Barriers to achieving more 3- Cumbersome registration procedures for facilities and products - While other businesses take less than two weeks to register, medical facilities and products take up to a year to register in many cases - Corruption cause of delay in many cases 12 Barriers to achieving more 4. Unnecessary barriers to accessing funds to which they are entitled – e.g. National Health Insurance Funds - In many countries, public facilities automatically benefit from NHI funds, while private facilities have to do more than required to get registered with the fund - Chocked again by poor terms/low prices 13 Barriers to achieving more 5. Double Standards: - Unrealistic quality standards that are unattainable in resource-poor settings - Not applied to public facilities - Used in some cases to “chock the private sector out of business” 14 There is light at the end of the tunnel Positive changes noted Policies in favor of PPPs Social Insurance schemes- are ready to work with private sector to serve the poor Governments, NGOs, DPs- include Private Sector in their strategies towards improving healthcare delivery Non-Healthcare private sector playing big role- FP, Diseases control 15 What would make things better for the Private Health Sector? Clear policies and guidelines that support private health sector investment in health, supported with legislative powers (Laws) PPP in healthcare: Contracting out of services to private health sector Provision of incentive packages to encourage investment in healthcare delivery, especially underserved areas Use of same yardstick in the enforcement of regulations related to health care provision Proper utilization of available resources in healthcare provision in both the private and public sector 16 Thank you for listening