Neuropharmacology
The Life of a Typical
Neurotransmitter
Precursors—”building blocks”
Synthesis—assembly of precursors into
neurotransmitter molecules
Transport to presynaptic terminal
Storage in presynaptic terminal
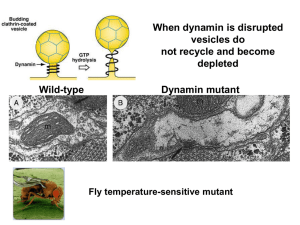
Release from terminal (exocytosis)
Binding to post-synaptic receptor
Inactivation
diffusion
reuptake
enzymatic degradation
Neurotransmitters
Criteria for Identification
Neurotransmitter
Criteria
1. Identity
2. Synthesis
Cell has precursors and enzymes
necessary for synthesis of n.t.
Neurotransmitter
Criteria
1. Identity
2. Synthesis
3. Release
Must be released from terminals;
(collect substance from cleft
after nerve stimulation)
Neurotransmitter
Criteria
1.
2.
3.
4.
Identity
Synthesis
Release
Receptors
Cross desensitization between
substance and suspected n.t.
Blockade of n.t. action by receptor
antagonists
Applicaton of suspected n.t.
mimics action of nerve stimulation
Neurotransmitter
Criteria
1.
2.
3.
4.
5.
Identity
Synthesis
Release
Receptors
Inactivation
Inactivation mechanism
enzymatic degradation
reuptake
Neurotransmitter
Criteria
1.
2.
3.
4.
5.
6.
Identity
Synthesis
Release
Receptors
Inactivation
Pharmacology
Same effect on ion channels;
p.s.p.’s have same reversal potentials
Same effect on membrane resistance
and potential
Applied substances must be effective
in physiological concentrations
Inhibition of degrading enzyme
prolongs action of both
Neurotransmitter
Criteria
1.
2.
3.
4.
5.
6.
Identity
Synthesis
Release
Receptors
Inactivation
Pharmacology
Receptor Subtypes
Drugs
1
2
3
a
4
b
Neurotransmitters
Receptor Subtypes
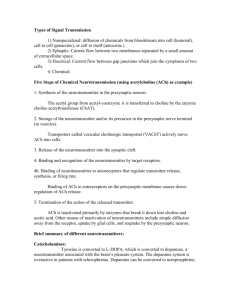
Acetylcholine Synthesis
Choline Acetyltransferase (ChAT)
Choline + Acetyl CoA
Acetylcholine + CoA
Degradation
Acetylcholine Esterase (AchE)
Acetylcholine
Choline + Acetate
Chemicals that Act
on ACh Systems
black widow spider venom
stimulates release of ACh
botulinum toxin
blocks release of ACh
curare
blocks ACh nicotinic receptors
insecticides
AChE inhibitors
atropine as antidote
blocks muscarinic receptors
Clinical Aspects
of ACh Systems
Alzheimer’s disease
loss of ACh neurons in
the basal nucleus of Meynert
Aricept—ACh agonist
Monoamines
single amine (NH2) group
Catecholamines (CAs)
dopamine (DA)
norepinephrine (NE, noradrenaline)
epinephrine (EPI, adrenaline)
Indoleamines
serotonin (5-hydroxy tryptamine, 5-HT)
Catecholamine synthesis
Serotonin synthesis
Dopamine Systems
Norepinephrine Systems
Serotonin Systems
Characteristics of
Monoaminergic Systems
Diffuse distribution of targets
Fine, unmyelinated axons
Metabotropic synapses
Functions of
Monaminergic Systems
“State” phenomena
sleep and arousal
hunger
mood
Amino Acid Transmitters
Excitatory Amino Acid
Glutamic Acid, or Glutamate
Inhibitory Amino Acids
Gamma Aminobutyric Acid (GABA)
Glutamic Acid
Decarboxylase (GAD)
Glutamic Acid
Glycine
GABA
Glutamate Receptor Subtypes
NMDA receptor binding sites
http://www.sumanasinc.com/webcontent/anisamples/neurobiology/
receptors.html
Glutamate
non-NMDA receptors
Na+ channels
open
removes
blockade
depolarization
NMDA receptors
Ca2+ channels
open
(Mg2+ blockade)
Ca2+ enters
when Mg2+
is removed
postsynaptic
effects
(learning)
Ca2+dependent
K+ channels
open
reinstates blockade
repolarization
a. Non-NMDA Na+ channels open, Na+
enters and depolarizes membrane
b. Mg2+ blockade of NMDA Ca2+ channels
removed by membrane depolarization;
Ca2+ enters
c. Ca2+ dependent K+ channels open;
membrane repolarized
depolarization
d. Mg2+ blockade reinstated
a
b c
d
NO
GABA receptor binding sites
Diffusible Gases
Nitric Oxide (NO)
Nitric Oxide
Synthase (NOS)
Arginine
NO + Citrulline
Carbon Monoxide (CO)
Heme Oxygenase
Heme
CO + biliverdin
Functions of
Diffusible Gas
Neurotransmitters
regulate blood flow
cerebral
peripheral (e.g. penis)
retrograde messenger
Hebb’s postulate of learning
(described for glutamate synapses
Peptide
Neurotransmitters
Often serve hormonal function
Substance P (P for “Peptide”)
Principal somatosensory transmitter
First peptide transmitter discovered
Gut hormones
e.g. angiotensin
neuropeptide Y
cholecystokinin
Releasing factors for hormones
e.g. thyrotropin releasing hormone
somatotrophin, somatostatin
corticotropin
Often violate “Dale’s Law” that a neuron releases one and
only one neurotransmitter—examples of co-localization.
Endogenous
Opiates
Morphine-like neurotransmitters
Endorphins and enkephalins
Important for control of pain
Also activate DA reward systems
released in response to intense physical
activity—e.g., runner’s high
Mechanisms
of Tolerance
1. Metabolic adaptation
2. Receptor regulation
3. Neural compensation
Addiction
• Physiological need for the drug
• May or may not include “craving”
• Craving is also referred to as
psychological dependence
• Repeated activation of DA reward system
(nucleus accumbens) leads to downregulation, decreased activity— the drug
is needed to restore normal activity.
• Prefrontal cortex inputs to nucleus
accumbens are important mediators of
psychological dependence.
• Antihistamines are examples of addiction
without craving
• Marijuana is an example of craving without
addiction
Withdrawal
Acute withdrawal—operation of compensated
nervous system in the absence of the drug
that produced the compensatory response
For drugs of abuse, typically anhedonia or
depression. My be severe, such as seizures.
Post-acute withdrawal—Less well understood
Reflects long-term changes in the nervous
system probably related to craving. Similar
to learning.
PAW also involves pre-frontal cortex
whci
Withdrawal
PAW also involves pre-frontal cortex, which is
responsible for regulating “impulsivity,” and
which provides glutaminergic input to the
nucleus accumbens.
Evidence suggests that glutamate
dysregulation is an important factor in
addiction and withdrawal, and is likely
involved in post-acute withdrawal,
psychological dependence and relapse.
Activation of DA “reward” systems common
denominator.
Basis of drug substitution in addicts.
(Also chocolate!)
Hallucinogens
Generally act on 5-HT systems
Lysergic acid diethylamide (LSD)
Psilocybin
Peyote
Methylenedioxyamphetamine (MDMA)
Ecstasy, XTC, etc.
Precise mechanisms of action unclear
LSD seems to act at 5-HT2 receptor
subtype
Less addictive than other classes of
abused drugs
Stimulants
Generally act on CA systems
Cocaine
Methamphetamine
Risk of addiction/craving high
activation of DA “reward systems”
Alcohol
Most commonly abused drug
Alcohol and barbiturates cross tolerant
Heroin
Heroin effective at opiate receptors in the brain
after being converted to morphine
Heroin, but not morphine, able to easily cross
blood-brain barrier, so heroin is drug of abuse
Common Prescription
Medications
Pain medications (Opioids)
Vicodin (hydrocodone + acetominephin)
OxyContin (oxycodone)
Percocet (oxycodone + acetominephin)
Darvocet (propoxyphene + acetominephin)
Darvon (fentanyl)
Dilaudid (hydromorphone)
Demerol (meperidine)
Lomotil (diphenoxylate)
Minor tranquilizers
Benzodiazepines(Valium, Xanax)
Stimulants
Adderall (3:1, d-:l-amphetamine)
Ritalin (methylphenidate)
Treatment of Addictions
Effective treatment multifaceted
1. Break cycle of addiction
in-patient treatment--detoxification
treatment of acute withdrawal
pharmacological intervention
e.g. nicotine patch or gum
2. Pharmacological maintenance
usually receptor blocker or
partial agonist—e.g. methadone, naloxon
3. Behavioral therapy
psychiatric counseling
group therapy—e.g. A.A. or N.A.
cognitive-behavioral therapy, etc.
learning to recognize and avoid
“triggers” for drug use
Treatment must be of adequate duration
Treatment of Addictions
What is “adequate duration?”
Typically, adequate duration means:
Several days of detoxification
• may include hospitalization with the use
of drugs to prevent harmful withdrawal
symptoms—e.g. use of
benzodiazepines in alcoholics to
prevent seizures
Several weeks to months of inpatient or
intensive outpatient rehabilitation
• highly structured environment
• psychotherapy
• goal is training in life-skills,
understanding the causes of abuse
Continued behavioral therapy of indefinite
perhaps lifelong, duration
• e.g. continued psychotherapy
• peer therapy—e.g. 12-step programs
Drugs that Act on
Ion Channels
tetrodotoxin
blocks voltage-sensitive Na+ channels
cocaine, local anesthetics
block voltage-sensitive Na+ channels
batrachotoxin
prevents inactivation of Na+ channels
tetraethyl ammonium
blocks voltage-sensitive K+ channels