Slides
advertisement
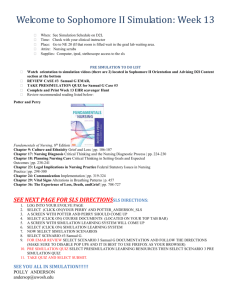
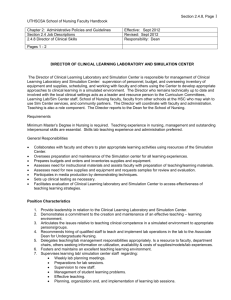
Retooling Health Assessment: It Takes More Than a Hammer Cheryl Wilson MSN, ARNP, ANP-BC Objectives Understand the gap between knowledge and skill Identify strategies to bridge knowledge and skill from Advance Health Assessment across to clinical courses Understand the continuum of simulated learning and how to apply in blended courses Who Am I? Advanced Registered Nurse PractitionerAdult Health Board Certified Instructor Graduate and Undergraduate programs Disclosure-provide noncompensated consultation as a SME to Shadow Health What were the challenges? Hybrid course only met 3 times a semester No simulation integrated into Health Assessment course Identified a gap between knowledge and skills Application of skills in the clinical setting Faculty challenges Use of simulation Faculty background and training Preparation for lab Ratio of faculty to students Consistency of lab experiences Modalities of Learning Task Trainers Digital Clinical Experience (DCE) Problem Based Learning (PBL) Clinical Reasoning exercises Case Studies Electronic Health Records (EHR) Observed Structured Clinical Exam (OSCE) Standardized Patients (SP’s) Digital Clinical Experiences Students interview the patient for a full health history Go through full physical exam of each system Documentation of findings Digital Clinical Experience Standardized experience Communication skills Physical exam skills Clinical judgment Problem Based Learning Case presentation in small groups Provide partial information in history – Students ask additional History questions – Discuss physical exam they would perform – 4-5 differential diagnosis – Match up signs and symptoms from case Observed Structured Clinical Exam Utilization of standardized patients Full health history Focused physical exam Differential diagnosis Final course competency-putting all the pieces together Continuum of Simulated Learning Why Simulation? – Provide opportunities to enhance critical thinking and clinical judgment – Ability to evaluate students effectively – Provide scenarios to enhance learning • Clinical situations possibly encountered in practice and how to work through clinical problems. Continuum OSCE Standardized Patients DCE High Fidelity Low Fidelity Task Trainers Faculty involvement Role of course coordinator Integration of simulation Digital clinical examination Facilitation of clinical reasoning Consistency of skills taught across all sections Pedagogical Background Development of expertise Clinical competence Benner (1984) From Novice to Expert Expert Proficient Competent Advanced Beginner Novice Benner, P. (1984) Training Provide faculty training in integration of the digital clinical experience – How to review results – Synthesize results – Troubleshoot student problems with software application Weekly schedule of all lab activities – Assigned to each faculty – Resource to prepare for upcoming lab sessions Documentation Integrated documentation of patient findings within the DCE – Model notes provided in grading rubric Documentation in EHR of Problem Based Learning group work Strategies Provide consistent training of all faculty in lab Integration of simulation throughout the course Inter-rater reliability of grading and evaluation Conclusion Re-tooling of the course to integrate simulation and strengthen diagnostic reasoning/clinical judgment skills. Utilization of multiple modalities of learning Training of faculty for reliability in evaluation and consistency of delivery Continuous evaluation of course to improve student learning outcomes References Benner, P. (1984). From Novice to Expert: Excellence and Power in Clinical Nursing Practice. Menlo Park: Addison Wesley. Fitzgerald, C., Kantrowitz-Gordon, I., Katz, J., & Hirsch, A. (2012). Advanced practice nursing education: Challenges and strategies. Nursing Research and Practice. doi:10.1155/2012/854918 Jerlock, M., Falk, K., & Severinsson, E. (2003). Academic nursing education guidelines: Tools for bridging the gap between theory, research and practice. Nursing and Health Sciences, 5, 219-228.