The Brain
advertisement

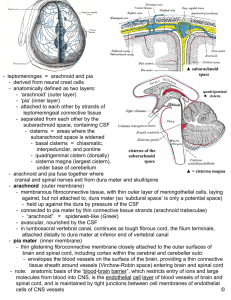
CURRENT TRENDS IN MANAGING SUBDURAL HEMATOMA INJURIES When is it Safe to Return to Contact Sports? Jamie Adams, MEd, ATC, CES Carolyn Dartt, MEd, ATC Ilona Barash, MD, PHD Objectives • Distinguish between different types of meningeal injuries in the brain • Discuss how subdural hematomas (SDH) effect contact athletes • Review and discuss current guidelines for return to play after SDH ANATOMY The Brain • Made up of 4 gelatinous lobes floating in cerebrospinal fluid (CSF) within the skull • Vascularized by the internal carotid and vertebral arteries, the internal jugular vein, the cerebral veins, external veins, basal vein, terminal vein, choroid vein and the cerebellar veins • The brain is covered by 3 meninges: • dura mater • arachnoid • pia mater From Left to Right: • Scalp • Periosteum • Skull • Dura Mater • Arachnoid • Pia Mater Dura Mater • Most superficial of the 3 meninges • Is a thick durable sac-like membrane consisting of large blood vessels • It is a fairly loose membrane comprised of dense fibrous tissues Arachnoid • Middle of the 3 meninges • Is named because of it's spider web-like appearance • Thin, transparent membrane • Considered important in the blood brain barrier Pia Mater • Deepest of the 3 meninges • In direct contact with the brain tissue and supplies the brain with nourishment through its capillaries • Very thin delicate tissue that follows all the contours of the brain 4 Types of Injuries Involving Bleeding Within the Skull • Epidural Hematoma • Subdural Hematoma • Subarachnoid Hemorrhage • Intracerebral Hemorrhage Intracerebral Hemorrhage • Bleeding in one or more of the lobes • Usually seen in traffic accidents or falls • Data have shown that traumatic intracerebral hemorrhages often expand over time • S&S often mimic stroke symptoms Subarachnoid Hemorrhage • Defined as bleeding between the arachnoid and pia mater membranes • Can happen spontaneously from an aneurysm rupture or from trauma • Symptoms include "thunderclap headache", loss of consciousness, vomiting and possibly seizures Epidural Hematoma • Is a collection of blood between the skull and the dura mater • ~15-20% are fatal • Most common cause is trauma; usually acceleration/ deceleration or transverse forces • Trauma causes tears to the arteries within the dura mater • Hematoma reaches maximum at ~6-8 hours after injury Epidural Hematoma S&S • Brief lucid period • Headache • Unconsciousness • Abnormal posturing • Abnormal pupil reactions • Weakness of the extremities on the opposite side from injury Subdural Hematoma • defined as a collection of blood between the dura mater and the arachnoid membrane • these injuries are usually associated with a traumatic brain injury (TBI); most often from shearing forces • results from injuring veins bridging between the dura mater and the other meninges • Signs and Symptoms (S&S) are often delayed because veins bleed slower than arteries Subdural Hematoma S&S • A history of recent head injury • Loss of consciousness or fluctuating • • • • • • • • • levels of consciousness Irritability Seizures Pain Loss of muscle control Altered breathing patterns Hearing loss or hearing ringing (tinnitus) Ataxia, or difficulty walking Blurred vision Deviated gaze, or abnormal movements • Numbness • Headache (either constant or • • • • • • • • fluctuating) Dizziness Disorientation Amnesia Weakness or lethargy Nausea or vomiting Loss of appetite Personality changes Inability to speak or slurred speech Management of Intracranial Hematomas • Epidural • Surgical • Thickness >30 cm3 regardless of the patient's GCS • Conservative • in patients with a GCS score greater than 8 without focal deficit • <30 cm3 thick • <15 mm thickness • <5 mm midline shift (MLS) • can be managed non-operatively with serial CT scanning and close neurological observation • Subarachnoid • Surgical • Rarely done in isolated traumatic SAH • If evaluation for underlying aneurysm is positive, this will often be treated • Conservative • In patients with a GCS score in the range of 13-15 • Monitoring with follow up scans to make sure bleeding is resolving • Monitor ICP and BP levels Management of Intracranial Hematomas • Subdural • Surgical • Thickness >10mm • Midline shift >5mm • If GCS score decreases 2+ points between injury and hospital admission • Asymmetric or fixed dilated pupils • ICP > 20 mmHg • Burr holes or craniotomy are the surgical procedures • Conservative • If GCS >9, monitor ICP • Small, no mass effect on CT • Risk of changing to chronic SDH • Reevaluate if neuro deterioration • If neuro deterioration occurs, repeat CT scans are indicated CASE STUDY CASE REPORT • 18 y/o MLAX athlete fell while skateboarding • Presented to ED with closed head injury • • • • 8 mm SDH and small focal SAH No acute cervical spine injury No skull fracture Athlete has no memory of fall • No previous history of concussions/TBI 27 Sep 2012 27 Sep 2012 • Initial Injury Oct 2012 • Last visit with personal neurosurgeon 1 Nov 2012 • Lacrosse PPE 1 Jan 2013 • Cleared to RTP by personal neurosurgeon • Initial visit with UCSD 17 Jan 2013 team physicians • Follow up 22 Jan 2013 MRI 7 Feb 2013 • RTP 22 Jan 2013 Case Report • Treatment • Rest • Personal neurosurgeon recommended no RTP as safest decision • If RTP is desired, at least 12 week waiting period with no high risk activities (non-contact drills/workouts ok) • Recommended waiting as long as possible to return to lacrosse • Team physicians and personal physicians discussed need for f/u MRI before clearance • MRI on 22 Jan 2013 showed that the SDH had resolved • Full RTP clearance as of 7 Feb 2013 • No further s/s since RTP Uniqueness • No clear current guidelines on return to contact sports after a subdural hematoma • Most relevant research was from around 1998 • This research recommended no RTP for at least 1 year • Discussion with several physicians of different specialties provided many different opinions on what was necessary to determine RTP timeline RETURN TO PLAY DISCUSSION Return to Play Guidelines After Head Injury Cantu 1998: • Conditions that contraindicate competition in contact sports • Persistent postconcussion symptoms • Permanent central neurologic sequelae from head injury (e.g., organic dementia, hemiplegia, homonymous hemianopsia) • Hydrocephalus • Spontaneous subarachnoid hemorrhage from any cause • Symptomatic neurologic or pain-producing abnormalities about the foramen magnum Cantu 1998 continued • No contact sports if operative intervention was required: • Concern about prolonged scarring of the pia-arachnoid • Loss of the normal cushioning effect of the CSF • “return to a collision sport may be permitted in selected cases 1 year or more after the injury if neurologic recovery is complete. Again, extreme deliberation and informed discussions with the athlete and his family is urged.” 1 Year Guideline • Davis et al 2010: • 31 yr. old boxer with SDH • No surgical intervention • Imaging included MRI/MRV/MRA and neurologic exam normal • Durand and Adamson 2004: • 1 year return to play guideline • No justifications were noted Nagahiro and Mizobuchi 2014 • Case reports of young Judo participants who returned to play after traumatic SDH, and had fatal recurrent SDH afterwards • “As most judo-related accidents happen in young inexperienced participants, even in a small subdural hematoma has been absorbed and neuroimaging returns to normal findings, in principle, children and adolescents must not be allowed to RTP.” AMSSM List Serve Survey Dr. Matthews Gammons: Vermont • “No evidence based guidelines. No expert based opinion guidelines that I have seen. We have had half a dozen over the last 5 years. All were out at least 3 months and had resolution (except hemosiderin) on imaging and normal neuro. Current thinking is this does not increase risk once resolved.” AMSSM List Serve Survey Dr. Jeffrey Radakovich: Washington • “I had an incoming freshman football player with a similar history who was asymptomatic with an essentially normal MRI by the time I saw him for a PPE. After discussions with several head injury experts including Dr. Cantu, we cleared him. The main issue was being sure there were no underlying structural issue that predisposed him to bleed such as an AVM. Prior to coming to see me he had had an MRA and I believe even a MR venogram. Would be worth considering MRA or does your radiologist feel confident that a vascular abnormality can be excluded with the MR?” AMSSM List Serve Survey Dr. Jennifer King: Hawaii • “I had a similar case, could not find guidelines, but discussed with colleagues and neurosurgeons; basic consensus was that as long as asymptomatic and bleed resolving, can RTP after 6 weeks from injury; both my kids did well.” Recommendations For Return to Play After Non-Operative Major Head Injury • A completely normal neurological exam • Advanced imaging after the event: • MRI: must be normal or perhaps only has some residual hemosiderin • Consider MRA/MRV • Must exclude any underlying predisposing factors for the initial bleed Recommendations For Return to Play After Non-Operative Major Head Injury • Informed Consent: • Long, involved discussion with the patient and family about all risks, benefits and alternatives • Time Frame? Unclear. • To be safe and within published guidelines, 1 year • General consensus seems to be sooner than that • Gradual Return to Play • Close monitoring of the athlete: • Concussion symptoms • Neurologic symptoms • Extra attention made to any repeat head injury Recommendations For Return to Play After Non-Operative Major Head Injury If there is any question about what to do, consult another specialist and get a second or third opinion: • Neurosurgeons • Neurologists • Primary Care Sports Medicine Specialists Our Case Conclusion • Cleared for play • Did great • No adverse outcomes (yet) • >2 years out • He and his family were excited to keep playing References • • 1. • • • • • • • • • • Garg RK, MD, Levine SR, MD. Traumatic intracerebral hemorrhage. Medlink Neurology. 2014. http://www.medlink.com/medlinkcontent.asp?page=home. 2. Bullock MR, MD, PhD., Chestnut R, MD, Ghajar J, MD, PhD., et al. Surgical Management of Acute Subdural Hematomas. Neurosurgery. March 2006 2006;58(3):S2-15-S12-24. 3. Ahmed E, Aurangzeb A, Khan S, et al. Frequency of conservatively managed traumatic acute subdural haematoma changing into chronic subdural haematoma. J Ayub Med Coll Abbottabad. Jan-Mar 2012 2012;24(1):71-74. 4. Phelan HA, Richter AA, Scott WW, et al. Does isolated traumatic subarachnoid hemorrhage merit a lower intensity level of observation than other traumatic brain injury? Journal of Neurotrauma. October 15, 2014 2014;31(20):1733-1736. 5. Cantu R. Return to play guidelines after a head injury. Clinical Journal of Sport Medicine. January 1998 1998;17(1):45-60. 6. Davis G, Marion D, Le Roux P, Laws E, McCrory P. Clinics in neurology and neurosurgery- extradural and subdural haematoma. Br J Sports Med. December 2010 2010;44(16):1139-1143. 7. Durand P J, Adamson G. On-the-field management of athletic head injuries. J Am Acad Orthop Surg. 2004 May-Jun 2004;12(3):191-195. 8. Giza C, Kutcher J, Ashwal S, et al. Summary of evidenc-based guideline update: evaluation and management of concussion in sports: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2013 Jun 11 2013;80(24):2250-2257. 9. Harmon K, Drezner J, Gammons M, et al. American Medical Society for Sports Medicine position statement: concussion in sport. Br J Sports Med. 2013 Jan 2013;47(1):15-26.