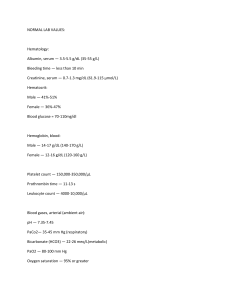
Adult and Elder II and Pharm Tutoring Session - Breast and Prostate Ca, BPH, and ED – Prepared by Fidel Lim, RN Case Scenario M.D. is a 60-year-old woman whose routine mammogram showed a 2.3 × 4.5 cm lobulated mass at the 3:00 position in her left breast. M.D. underwent a stereotactic needle biopsy and was diagnosed with infiltrating ductal carcinoma that was both estrogen and progesterone receptor positive. The staging workup was negative for distant metastasis. Her final staging was stage IIB. She had a modified radical mastectomy with lymph node dissection. The sentinel lymph node and 11 of 16 lymph nodes were positive for tumor cells. An implanted port was also placed during surgery for chemotherapy infusion. Medical-Surgical History – CAD, HLD, HTN, osteoarthritis, recurrent UTI, gout, and breast mass Allergy – Cipro – rashes Admission Vital Signs: BP - 96/64, HR – 105 bpm, 16, and 98.6° F (37 ° C). Weight is 140 lbs. and height is 5 ft, 5 in. BMI – 23.3 Social History: No toxic habits, divorced, no children. Works as a partner in a law firm. Mother died of breast cancer. Father lives in a nursing home. A sister lives out of town. Lab Results Complete Blood Count Normal Results WBC - 5,000 to 10,000/mm3 Hgb – Male (14 - 18 grams/dL), Female (12.0-16 grams/dL Hct - Male (42 – 52%), Female (37 – 47%) Platelets - 150,000 to 450,000/mcL Electrolytes Normal Sodium 135-145 mmol/L Potassium 3.5-5.0 (mEq/L) Chloride 95-105 mmol/L CO2 (Think HCO3) 19–25 mEq/L Results 146 3.8 100 22 Normal BUN 8-21 mg/dL Creatinine 0.6 to 1.2 mg/dL Glucose 65-110 mg/dL Calcium 9–11 mg/dL Results 30 1.1 120 7.0 10,500 11 33.2 391,000 Normal Magnesium 1.5-2 mEq/L Phosphate 2.5 to 4.5 mg/dL GFR >60 mL/min Albumin 3.5 to 5.5 g/dL Results 1.7 3.5 55 mL/min 3.7 Coags Normal INR Normal: 0.6 – 1.7 aPTT Normal: 25 – 35 seconds Results 1.0 30 1 Provider Orders OOB as tolerated Regular diet CBC, BMP in a.m. Empty Jackson Pratt every shift and PRN Incentive Spirometer 10X every hour while awake Meds (current orders) IV Lactated Ringers 125 mL/hour for 24 hours Acetaminophen 650 mg PO Q 6 hours for fever and pain <4/10 Heparin 5000 units SQ every 12 hours Piperacillin-Tazobactam 3.375 g IVPB every 6 hours for 2 days Ascorbic acid 500 mg PO BID Oxycodone and acetaminophen 5 mg/325 mg PO every 6 hours PRN for pain >4/10 Colchicine 0.6 milligram mg BID Aspirin 81 mg PO daily Ondansetron 4 mg PO every 8 hours for nausea/vomiting 1. Conduct a medication reconciliation. 2. Interpret the lab values and explain what possible manifestation is associated with the abnormal findings. 3. Around lunch time, as the nurse assisted the patient to get out of bed to chair, the patient becomes lightheaded and a little clammy. What should the nurse do first? 4. Explain the significance of the patient’s history of recurrent UTI. 5. A student nurse asked the primary nurse about the common risk factors for breast cancer. When should the RN say? 6. Describe some of the nursing care and self-management for patients who had modified radical mastectomy (e.g., immediate post-op and long-term). CASE STUDY PROGRESS M.D. has now completed three (out of 6) cycles of CAF (cyclophosphamide [Cytoxan], fluorouracil [5FU], and doxorubicin [Adriamycin]). Her last treatment with doxorubicin, cyclophosphamide, and 5fluorouracil was approximately 12 days ago. She comes to the emergency department with a 2-day history of fever, chills, and shortness of breath. On arrival, she is disoriented and agitated. Vital signs are 2 86/43, 119, 28, 103.6° F (39.8° C), Sa O 2 85% on room air. Chest x-ray demonstrates diffuse infiltrates in the left lower lung. Lab Results Complete Blood Count Normal WBC - 5,000 to 10,000/mm3 Hgb – Male (14 - 18 grams/dL), Female (12.0-16 grams/dL Hct - Male (42 – 52%), Female (37 – 47%) Platelets - 150,000 to 450,000/mcL Electrolytes Normal Sodium 135-145 mmol/L Potassium 3.5-5.0 (mEq/L) Chloride 95-105 mmol/L CO2 (Think HCO3) 19–25 mEq/L Results 146 3.9 105 24 Normal BUN 8-21 mg/dL Creatinine 0.6 to 1.2 mg/dL Glucose 65-110 mg/dL Calcium 9–11 mg/dL Results 40 1.5 93 8.0 Results 3,000 7.5 23 80,000 Normal Magnesium 1.5-2 mEq/L Phosphate 2.5 to 4.5 mg/dL GFR >60 ml/min Albumin 3.5 to 5.5 g/dL Results 2.0 2.5 3.0 Lactic acid - 2.4 mg/dL (normal: 0.5-1 mmol/L) Coags Normal INR Normal: 0.6 – 1.7 aPTT Normal: 25 – 35 seconds Results 1.3 30 7. Interpret M.D.'s lab results. 8. What treatment do you anticipate for M.D.? In another part of the hospital … S.M., a 56-year-old man who is being examined in the outpatient clinic for routine checkup. He reports that he has been feeling well and has no specific complaints, except for some trouble “emptying my bladder.” Vital signs (VS) at this visit are 148/88, 82, 16, 96.9° F (36.1° C). He had a CBC and complete metabolic panel (CMP) completed 1 week before his visit, and the results are normal, except for: Prostate-specific antigen (PSA) - 8.23 ng/mL (normal: Less than 4.0 ng/mL) 9. What is the significance of the PSA result? 3 10. What other specific examination will S.M. need to have along with the PSA? While obtaining your nursing history, you record a family history of prostate cancer or other genitourinary (GU) problems. S.M. reports frequency, urgency, and nocturia × 4; he has a weak stream and has to sit to void. These symptoms have been progressive over the past 6 months. He reports he was diagnosed with a large prostate a few years ago. Last month, he began taking saw palmetto capsules but had to stop taking them because they “made me sick.” 11. Why is S.M. having difficulty passing urine and are potential complications of urinary retention? 12. Commonly used medications for BPH are 5-alpha reductase inhibitors, such as finasteride (Proscar) and alpha 1 blocking drugs, such as tamsulosin (Flomax). How do these drugs differ? 13. The PCP ordered tamsulosin (Flomax) 0.4 mg/day PO. You enter S.M.'s room to teach him about this medication. What side effects will you tell S.M. about? Select all that apply. A. B. C. D. E. F. Dizziness Diarrhea Dry mouth Insomnia Heartburn Orthostatic hypotension 14. What would you expect S.M. to report if the medication was successful? CASE STUDY PROGRESS S.M. returns in 8 months to report that his symptoms are worse than ever. He has tried several different medications, but medication management failed, and he is told that he might benefit from transurethral resection of the prostate (TURP). 15. Describe the TURP procedure. 16. S.M. asked the nurse if he were to have a prostatectomy, “what would be complications?” 17. What self-management activities can S.M. do prevent the potential complications of prostatectomy? 4 CASE STUDY PROGRESS 10 months later, S.M. returns for a radical prostatectomy (perineal approach). He returns to the surgical unit returns with these initial postoperative orders shown below. 18. Which orders are appropriate for S.M.? (Select all that apply, and correct the inappropriate answers.) A. B. C. D. E. F. G. H. Vital signs per hospital protocol Notify physician if urinary output is less than 30 mL/hr OOB on his own Continuous bladder irrigation (CBI) Discontinue Foley catheter in 12 hours Oxybutynin (Ditropan XL) 10 mg PO every morning Docusate (Colace) 100 mg PO daily Morphine 4 mg IV push q4h prn pain 19. Describe standards of practice in the care of a patient with CBI. 20. Post-TURP, the patient was prescribed vancomycin 1 g IVPG every 12 hours for 3 days. The lab called to inform the RN that the vancomycin trough level of the patient is elevated. What should the nurse do next? CASE STUDY PROGRESS S.M. does not require any additional therapy after surgery. At his 6-month follow-up visit, he reports he can get an erection but has difficulty maintaining an erection for sexual relations. 5