Cases
advertisement

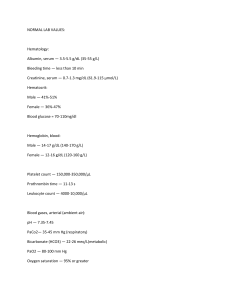
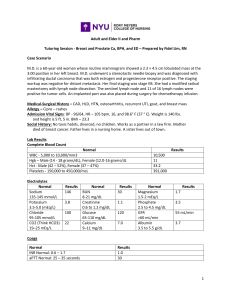
Cases case 1: Patient C is a female patient, 32 years of age, with a history of hypertension and asthma. Her current medications include albuterol (as needed via inhaler), atenolol 25 mg twice daily, and 25 mg hydrochlorothiazide. She is admitted to the hospital with a diagnosis of exacerbation of asthma secondary to bronchitis. She is treated with albuterol treatments every 3 hours, a cephalosporin antibiotic, and a prednisone taper. After 24 hours, Patient C complains of severe muscle cramps. A basic metabolic profile (Chem-7) is requested, which reveals normal renal function, a potassium level of 2.9 mEq/L? 1. What is the clinical condition, what do you think patient C suffer from? Based on what criteria was this diagnosis made 2. What further lab investigation you recommend in her case? 3. Make management for this patient & review her drugs? case2: 79-year-old female with a history of mild dementia presents with worsening confusion over the last 2 days. She lives in a nursing home and has recently been treated with antibiotics for a urinary tract infection. Her temperature is 38.1° C, pulse 90, respiratory rate 18, and blood pressure 118/60 mm Hg. She is disoriented and lethargic. Examination of the heart, lungs, and abdomen is unremarkable. Laboratory studies are as follows: Na 165 meq/L, K 4.6 meq/L, Cl 118 meq/L, HCO3 28 meq/L, BUN 31 mg/dL, Cr 1.1 mg/dL. Urine-specific gravity is 1.030 and urine osmolality is 700 mmol/kg. 1. What condition this patient suffers from? What is the cause of her condition? 2. What the Initial treatment for this patient should be? 3. What are the general causes could be implicated? case3: Patient R is a man, 56 years of age, with diabetes and hypertension. He is currently being treated with metformin 1 g twice per day, lisinopril 40 mg/day, and amlodipine 10 mg/day. His blood pressure is 146/83 mm Hg, and lab work reveals the following abnormalities: BUN 83 mg/dL, serum creatinine 4.1 mg/dL, and potassium 7.3 mEq/L. He is rushed urgently via emergency medical services to the local hospital, where an ECG is obtained immediately. Blood gases are sent to rule out lactic acidosis due to use of metformin in acute renal failure. The ECG shows widening of the QRS wave, and Patient R is showing signs of muscle weakness. He is treated emergently with calcium gluconate 10% 10 mL infusion while his ECG is monitored. 1. What is the clinical indication in his case, what do you think patient R suffer from? Based on what criteria was this diagnosis made 2. What further lab investigation you recommend in his case? 3. Make management for this patient & review his drugs? case4: 21-year-old woman with an eight-year history of juvenile onset diabetes was brought to the hospital in a coma. She had required 92 units of insulin daily to maintain her blood glucose concentration in an acceptable range and prevent excessive glucosuria. On admission she had a BP of 92/20 mmHg, a pulse of 122 beats/min, and deep respirations of 32/min. Lab data showed: ABG: Serum chemistry values PH pO2 Na+ Cl- =7.10 =90 mmHg =129 mmol/L =95 mmol/dL pCO2 HCO3 K+ Total CO2 =15 mmHg =4 mmol/L =6.4 mmol/L = 5mmol/L The serum was strongly positive for ketones. Eight units of regular insulin were given IV and 8 units/h were given by IV infusion pump. Her serum glucose concentration fell at a rate of approximately 100 mg/dL each hour. 1.What is the nature and etiology of the acid-base disturbance? How can you treat such condition? 2. Is there indication for a normal compensatory response? 3.What are serum ketones (ketone bodies)? How are they frequently detected? 4. Explain the abnormal serum potassium result. 5.Explain the serum sodium result. 6.What is the cause of her BP value upon admission?