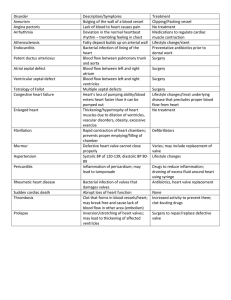
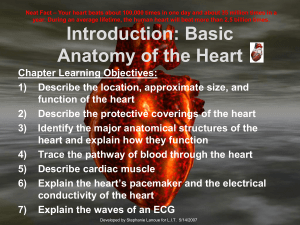
NUR314 Week 3: Heart and Neck Vessels Saturday, June 3, 2023 6:24 PM Cardiovascular System Highly complex Heart and closed system of blood vessels Heart and Great Vessels Heart Hollow, muscular, four chambered organ (atria/ventricles) Middle of thoracic cavity in the mediastinum Inverted cone or triangle from left 2nd-5th ICS Great Vessels Large veins and arteries leading directly TO and AWAY Superior and Inferior Vena Cava - return blood to the right atrium from the upper and lower body Pulmonary Artery - leaves RV and carries to Lungs Pulmonary Veins (2 from each lung) - returns O2 blood to LA Aorta - transports O2 blood from LV to the body Heart Wall Heart wall has numerous layers: Pericardium: tough, fibrous, double-walled sac that surrounds and protects hear Myocardium: muscular wall of heart Endocardium: thin layer of endothelial tissue that lines inner surface of heart chambers and valves Heart Chambers Four chambers: → Right Atrium (RA) → Left Atrium (LA) → Right Ventricle (RV) → Left Ventricle (LV) Separated by the Septum 2 Pumps: Right side pumps blood into the lungs Left side pumps blood into the body Valves There are 4 Heart valves. They allow for unidirectional flow of blood. They only one way. Prevents backflow of blood. Two Atrioventricular (AV) VALVES located at the ENTRANCE of the ventricles ▪ Tricuspid – between RA and RV rt y open one way. Prevents backflow of blood. Two Atrioventricular (AV) VALVES located at the ENTRANCE of the ventricles ▪ Tricuspid – between RA and RV ▪ Mitral/Bicuspid – Between LA and LV → Allows blood flow from atria to ventricles, snap shut when ventricles b to contract Two Semilunar (SL) VALVES located at the EXIT of each ventricle at the great vessel ▪ Pulmonic – exit RV and entrance to pulmonary artery ▪ Aortic – exit LV and entrance to aorta → Open during ventricular contraction, close when ventricles relax Heart Wall, Chambers and Valves Electrical Conduction of the Heart • Cardiac muscle cells – unique, automatic ability ► Generate electrical impulse and conduct it through the heart begin • • • • • • • Electrical Conduction of the Heart Cardiac muscle cells – unique, automatic ability ► Generate electrical impulse and conduct it through the heart Special sections of the myocardium – regulates the filling and emptying of the he chambers Sinoatrial (SA) node – posterior wall of the RA, near the junction of the vena ca (SVC, IVC - Superior/ Inferior Vena Cava) SA NODE IS THE PACEMAKER - Generates impulses at 60-100 per minute Current travels through the atria – to the AV node to the AV bundle in the interventricular septum Then to bundle branches to the myocardium of both ventricles RESULT: CONTRACTION of the Muscles ◊ Can be measured through an EKG Cardiac Cycle Refers to filling and emptying of the heart’s chambers Diastole (RELAXATION of the ventricles) – filling Lasts 2/3 of the cycle AV valves open, ventricles relax, blood rushes in Rapid early filling (PROTODIASTOLIC) Atria contracts (ATRIAL KICK) – last kick by the atria Systole (CONTRACTION of the ventricles) – emptying Lasts 1/3 of the cycle Pressure in Vent > Atria AV Valves close (S1) Beginning of systole & all four valves are closed and ventricles contract Higher pressure in ventricles and Aortic and Pulmonic valves open – Blood eject Pressure falls and valves close (S2), Ventricle relaxes eart avas ted Heart Sounds First heart sound (S1) – LUB SOUND Closure of AV valve—signals beginning of systole S1 Loudest at apex Correlates with pulse, with carotid Second heart sound (S2) – DUB SOUND Closure of semilunar valve—signals end of systole, beginning of Diastole S2 loudest at base Splitting of S2 – normal, occurs toward the end of inspiration in some people, he only in the pulmonic valve area Extra Heart Sounds: S3 Third heart sound (S3): Volume Overload S3: Ventricular Gallop (fluid causes extra sound) → use BELL over APEX ▪ Physiologic: Children, Young adults (<40 men. <50 women), Athletes, Pregnancy (3rd trimester). Disappears when patient sits up. eard S1 and S2 S3 S4 Descrip1on of Heart… Third heart sound (S3): Volume Overload S3: Ventricular Gallop (fluid causes extra sound) → use BELL over APEX ▪ Physiologic: Children, Young adults (<40 men. <50 women), Athletes, Pregnancy (3rd trimester). Disappears when patient sits up. ▪ Pathologic: Fluid overload. CHF, Hyperthyroidism, Anemia, Pregnancy (1s 2nd Trimester) ○ Occurs immediately after S2, when AV valves open and atrial blood first pours in ventricles. Extra Heart Sounds: S4 S4: Atrial Gallop (hardening of ventricle (pressure) causes sound) → use BELL over APEX • Physiologic: (hardly ever) 40-50 y/o after exercise. • Pathologic: HTN, CAD, Cardiomyopathy, obstruction of blood (aortic steno and ventricular hypertrophy) • S4 occurs just before S1 17 Extra Heart Sounds: Murmurs Gentle, blowing, swooshing sound that can be heard on chest wall Conditions that create turbulent blood flow and collision currents Conditions that can result in murmurs: • Velocity of blood increases • Viscosity of blood decreases • Structural defects in valves Murmurs Systolic murmur – may occur with healthy heart OR with heart disease, Usually with S1 Diastolic murmur – always heart disease Innocent – no pathological cause Functional – increased blood flow through the heart (pregnancy, anemia, fever, a children) of Heart… st & nto osis heard PQRSTU Questions Related t • What makes Provocati ve and in • What makes Palliative Quality • What does th Note: If the client str such as “aching,” “sta to Pain s your pain worse? s your pain feel better? he pain feel like? ruggles to answer this question, you can provide suggestions abbing,” “burning.” children) ▪ ▪ ▪ ▪ Characteristics of Sound All heart sounds are described by: Frequency or pitch: high or low Intensity or loudness: loud or soft Duration: very short for heart sounds; silent periods are longer Timing: systole or diastole 20 Developmental Competence uPregnant woman Developmental Competence Pregnant woman Blood volume increases by 30% to 40% during pregnancy. Despite increased cardiac output, arterial blood pressure decreases in pregnancy a result of peripheral vasodilation. Infants and children Fetal heart begins to beat after 3 weeks’ gestation. Inflation and aeration of lungs at birth produces circulatory changes. Aging adult Closely interrelated with lifestyle, habits, and diseases Lifestyle, smoking, diet, alcohol use, exercise patterns, and stress have an influen • What makes Palliative Quality • How bad is y Quantity Region • Where do yo • Point to whe Radiation • Does the pai • Do you feel t Severity (severity scale) Timing Treatmen t as a nce on • What does th Note: If the client str such as “aching,” “sta • How would y and 10 being Note: The severity sc provide evaluation o provide some sort of was effective. • • • • • • When did the What were y Where were Is the pain co If the pain is How long do • Have you tak • Have you trie • What do you Understa nding s your pain feel better? he pain feel like? ruggles to answer this question, you can provide suggestions abbing,” “burning.” your pain? ou feel the pain? ere you feel the pain. in move around? the pain elsewhere? you rate your pain on a scale of 0 to 10, with 0 being no pain g the worst pain you’ve ever experienced? cale is an important assessment of pain and when used can of a treatment’s effectiveness. After eliciting a baseline, you may f pain control intervention and then reassess the pain to see if it e pain start? you doing when the pain started? you when the pain started? onstant or does it come and go? intermittent, when did it last occur? oes the pain last? ken anything to help relieve the pain? ed any treatments at home for the pain? u think is causing the pain? Inflation and aeration of lungs at birth produces circulatory changes. Aging adult Closely interrelated with lifestyle, habits, and diseases Lifestyle, smoking, diet, alcohol use, exercise patterns, and stress have an influen coronary artery disease. Pumping Ability Cardiac output: In resting adult, heart normally pumps between 4 and 6 L of bloo minute throughout body CO= HR x SV Heart can alter its cardiac output to adapt to metabolic needs of body. Preload and afterload affect heart's ability to increase cardiac output. Preload: venous return that builds during diastole According to Frank-Starling law, greater the stretch, the stronger the heart's contraction. • This increased contractility results in an increased volume of blood ejected, increased stroke volume. Afterload: opposing pressure ventricle must generate to open aortic valve against higher aortic pressure • Resistance against which ventricle must pump its blood Neck Vessels nce on od per t Hemodynamic Changes with Aging Pressure/pulse changes uPressure/pulse changes Isolated systolic HTN: Increase in systolic BP due to thickening and stiffening o arteries Left ventricular wall becomes thicker but the overall size of the heart does not ch Pulse pressure increases. No change in resting heart rate or cardiac output at rest Ability of heart to augment cardiac output with exercise is decreased. Dysrhythmias Presence of supraventricular and ventricular dysrhythmias increases with age. Ectopic beats common in aging people; usually asymptomatic in healthy older pe may compromise cardiac output and blood pressure when disease present Tachyarrhythmias may not be tolerated as well in older people. Electrocardiogram changes: Occur as result of histologic changes in conduction system; these changes includ □ Prolonged P-R interval (first-degree AV block) □ Prolonged Q-T interval □ QRS interval unchanged □ Increased incidence of bundle branch block Cardiac Disease and Aging Adult Incidence of coronary artery disease increases sharply with advancing age and accounts for about half of deaths of older people. ▪ Hypertension and heart failure also increase with age ▪ Lifestyle habits play a significant role in the acquisition of heart disease. Increasing the physical activity of older adults associated with a reduced risk for of the hange. eople, de: death Incidence of coronary artery disease increases sharply with advancing age and accounts for about half of deaths of older people. ▪ Hypertension and heart failure also increase with age ▪ Lifestyle habits play a significant role in the acquisition of heart disease. Increasing the physical activity of older adults associated with a reduced risk for from cardiovascular diseases and respiratory illnesses - Both points underscore need for health teaching as an important treatment parameter. ○ ○ ○ ○ ○ Culture and Genetics CVD: most common underlying cause of death globally Risk increased with race, ethnicity, gender, socioeconomic status, and educationa - Recommend favorable lifestyle: no current smoking, no obesity, physical ac at least once a week and a healthy diet - Consider access to care Risk factors - Identification, early treatment, and health promotion: uConsider access to care HTN Smoking Serum cholesterol Physical activity Sex and gender differences- leading cause of death in women Subjective Data – Review of Systems - CV Chest pain ► PQRSTU Dyspnea 27 Subjective Data – Review of Systems - CV uChest pain Exertional or at rest, constant or intermittent ► PND (Paroxysmal nocturnal dyspnea ) – occurs with heart failure, affects ADLs Orthopnea # of pillows used when supine Cough death al ctivity s Orthopnea # of pillows used when supine Cough u# of pillows used when supine uCough Duration, frequency, productive Fatigue Onset, time of day Edema Any swelling of hands or feet, does it resolve at night Nocturia Get up at night, how long? frequency Past Cardiac History HTN, high cholesterol, heart disease, rheumatic fever, surgery Family Cardiac History HTN, CAD, sudden death at an early age Cardiac risk factors Nutrition, smoking, alcohol, exercise, medication Infants, Children and Pregnant Women Infants Maternal health: How was mother’s health during pregnancy? Feeding pattern: Any cyanotic changes during nursing or crying? Growth and activity: Meeting developmental outcomes? Children Growth and activity: Meeting developmental outcomes? Evidence of any chest pain? History of respiratory infections Significant family history—genetic abnormalities Growth and activity: Meeting developmental outcomes? Evidence of any chest pain? History of respiratory infections Significant family history—genetic abnormalities uHistory of respiratory infections Pregnant women HTN during pregnancy? Associated clinical symptoms—proteinuria, weight gain, edema? Experiencing faintness or dizziness? Additional History for Aging Adult Medical history • Review presence of comorbidities. Medication profile history • Rx or OTC • Aware of side effects • Compliance with therapy uAware of side effects uCompliance with therapy Environment • Impact on ADLs Preparation and Equipment Preparation To evaluate carotid arteries, a person can be sitting. To assess jugular veins and precordium, the person should be supine with head chest slightly elevated. Ensure woman’s privacy by keeping her breasts draped. Equipment Marking pen Small centimeter ruler Stethoscope with diaphragm and bell endpieces Alcohol wipe to clean endpiece uu d and Marking pen Small centimeter ruler Stethoscope with diaphragm and bell endpieces Alcohol wipe to clean endpiece uu Physical Exam Carotid Arteries Inspect Palpate Auscultate for bruits Jugular Veins INSPECT Pulsation 2 ruler test Hepatojuguloreflux - consists of a distention of the neck veins when pressure is applied over the l - an indication that the right ventricle cannot accommodate an increased veno return Precordium 2 uPrecordium Inspect anterior chest for heaves, lifts, & apical pulse Palpate: heaves, lifts, thrills, apical pulse Percussion: Deferred Auscultation: - Bell: murmurs, S3 - Diaphragm: S1, S2, S3, S4 - Apical Pulse Neck Vessels: Palpation and Auscultation Palpate carotid artery ○ Palpate only one carotid artery at a time to avoid compromising arterial bloo brain. ○ Feel contour and amplitude of pulse, normal strength 2+. ○ Findings should be same bilaterally Auscultate carotid artery. liver ous od to brain. ○ Feel contour and amplitude of pulse, normal strength 2+. ○ Findings should be same bilaterally Auscultate carotid artery. ○ Assess for presence of carotid bruit. ○ Avoid compressing the artery which can create an artificial bruit. ○ Keep neck in neutral position and lightly apply stethoscope at angle of jaw, midcervical area, and base of neck uAuscultate carotid artery. uAuscultate carotid artery. uAssess for presence of carotid bruit. The Physical Exam: Great Vessels Jugular veins Inspect the jugular venous pulse Estimate the jugular venous pressure Palpate for hepatojugular reflux Precordium Inspect anterior chest: ○ Arrange tangential lighting to accentuate any flicker of movement. ○ Observe for any possible pulsations. Palpate apical impulse: ○ Note location, size, amplitude and duration ○ Palpate across precordium to assess for any possible pulsations Auscultation: Identify auscultatory areas associated with valves. Sound radiates with blood flow direction; valve areas are: Second right interspace: aortic valve area Second left interspace: pulmonic valve area Left third to fourth lower interspace: tricuspid valve area Fifth interspace at around left midclavicular line: mitral valve area Note rate and rhythm: describe characteristics Identify S1 and S2 Listen for extra heart sounds: describe characteristics. Listen for murmurs: Timing, loudness, pitch, pattern, quality, location, radia posture and change of position. uSecond left interspace: pulmonic valve area uLeft third to fourth lower interspace: tricuspid valve area ation Listen for extra heart sounds: describe characteristics. Listen for murmurs: Timing, loudness, pitch, pattern, quality, location, radia posture and change of position. uSecond left interspace: pulmonic valve area uLeft third to fourth lower interspace: tricuspid valve area uSecond left interspace: pulmonic valve area uLeft third to fourth lower interspace: tricuspid valve area uNote rate and rhythm: describe characteristics uIdentify S1 and S2. uListen for extra heart sounds: describe characteristics. uListen for murmurs: Timing, loudness, pitch, pattern, quality, location, radiation posture and Developmental Competence: Infants Transition from fetal to pulmonic circulation occurs in immediate newborn perio • Heart rate may range from 100 to 180 beats per minute (bpm) immediately a birth Note any extracardiac signs that may reflect heart status • Skin, liver size, and respiratory status Murmurs in the immediate newborn period do not necessarily indicate congenita disease seen due to shunt closure. • Murmurs are usually grade 1 or 2, systolic, no other signs of heart disease a disappear in 2 to 3 days. • Absence of murmurs in the immediate newborn period does not ensure a he heart. • Best to listen frequently and to note and describe any murmur according to ation n od after l heart and ealthy disease seen due to shunt closure. • Murmurs are usually grade 1 or 2, systolic, no other signs of heart disease a disappear in 2 to 3 days. • Absence of murmurs in the immediate newborn period does not ensure a he heart. • Best to listen frequently and to note and describe any murmur according to characteristics. Children Note any extracardiac or cardiac signs that may indicate heart disease. ▪ Poor weight gain, developmental delay, persistent tachycardia, tachypnea, dyspnea on exertion, cyanosis, and clubbing - Note that clubbing of fingers and toes usually does not appear until late first year, even with severe cyanotic defects. Palpate apical pulse • Be aware of location by age. • Rhythm remains characterized by sinus dysrhythmia • Physiologic S3 is common in children. Children Heart Murmurs uNote that clubbing of fingers and toes usually does not appear until late in first y even with severe cyanotic defects. Innocent (or functional) - Very common through childhood - Some say they have 30% occurrence, and some say nearly all children may demonstrate murmur. Patient teaching: ○ Need to believe that this murmur is just a “noise” and has no pathologic significa ○ Knowledge through education to prevent overprotection and limit activity for chi Pregnant Woman Vital signs increase in resting pulse rate of 10 to 15 bpm and drop in BP from no pre- pregnancy level. Palpation of apical impulse is higher, and lateral compared with normal position. Heart sounds: Changes due to increased volume and workload Aging Adult and ealthy e in year, ance ild ormal . pre- pregnancy level. Palpation of apical impulse is higher, and lateral compared with normal position. Heart sounds: Changes due to increased volume and workload Aging Adult Gradual rise in systolic blood pressure common with aging; widening of pulse pressure—be alert for orthostatic hypotension Left ventricular wall thickness increase. Presence of supraventricular and ventricular dysrhythmias increases with age. uAge-related ECG changes occur due to histologic changes in the conduction sys u Health Promotion and Patient Teaching Appropriate aspirin therapy Blood pressure control Cholesterol control Smoking cessation Lifestyle changes : - Diet - Physical activity - Weight control Differential Diagnosis of Chest Pain Cardiovascular ◊ Ischemic: Angina pectoris, Prinzmetal or variant angina, and acute coronary syndrome (ACS) ◊ Non-ischemic: Pericarditis, mitral valve prolapse, aortic dissection, and secondary pulmonary HTN Pulmonary ◊ Pulmonary embolism, pneumonia, and pneumothorax Gastrointestinal ◊ Gastroesophageal reflux, esophageal spasm, cholecystitis, and pancreatitis Dermatologic ◊ Herpes Zoster . stem. y Gastrointestinal ◊ Gastroesophageal reflux, esophageal spasm, cholecystitis, and pancreatitis Dermatologic ◊ Herpes Zoster Musculoskeletal/neurologic ◊ Costochondritis and chest wall muscle strain Psychogenic ◊ Depression and anxiety Abnormal Findings: Abnormal Pulsations: Precordium Thrill at the base Lift (heave) at the left sternal border Volume overload at the apex Pressure overload at the apex Lift (heave) at the left sternal border Volume overload at the apex Pressure overload at the apex Heart and Neck Vessels Examinatio on