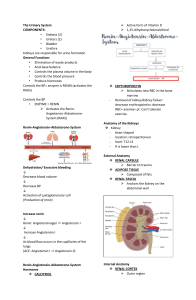
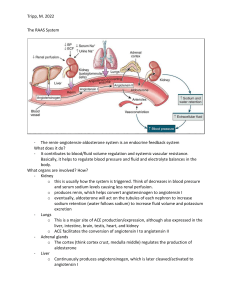
ANTI-HYPERTENSIVES Krisi Amsden, DNP, RN ATI: Chapter 20 Frandsen: Chapter 26 HTN Overview • Common, chronic disorder affecting more than 100 million adults in the United States • Hypertension the risk of – MI, HF – Cerebral infarction and hemorrhage – Renal disease BP Regulation Mechanisms • • • • • Pages 509 – 511 Box 26.1 Neural Hormonal Vascular Vascular Remodeling BP Regulation: Neural • • • SNS stimulation – Chronotropy – Inotropy Activated by vasomotor center in the brain – Baroreceptors – Chemoreceptors Blunted response with antihypertensives = orthostatic hypotension Hypotension SNS activation – Production Epinephrine/Norepinephrine Vasoconstriction Stimulation of beta-adrenergic receptors in the heart Increased BP, CO, tissue perfusion BP Regulation: Hormonal (RAAS) BP LOW Renin secreted from kidneys Renin stimulates increased conversion of angiotensinogen to angiotensin I Angiotensin I converted to angiotensin II by angiotensin-converting enzyme (ACE) Angio II causes vasoconstriction & stimulates release of aldosterone Aldosterone causes Na and H2O retention B/P rises Renin release is inhibited BP Regulation: Vascular • Vasoconstrictors: – Angiotensin II – Endothelin 1 – Platelet-derived growth factor – Thromboxane A2 • Vasodilators: – Nitric oxide (NO) – Prostacyclin BP Regulation: Vascular Remodeling • Thickening of the blood vessel wall = narrowing of the blood vessel lumen. • Less flexible – Unable to respond as well to vasodilating substances. Hypertension • Persistently high blood pressure that results from abnormalities in regulatory mechanisms – Systolic pressure greater than 140 mm Hg – Diastolic pressure greater than 90 mm Hg • Primary: 90% to 95% of known cases • Secondary: may result from renal, endocrine, or CNS disorders or from medications HTN Pharm Therapy • Keep B/P less than 140/90 • Two main actions: – Decrease volume of circulating blood – Reduce systemic vascular resistance (SVR) • Remember…B/P = CO x SVR (CO = HR x SV) Principles of Therapy • JNC 8 – Patients ≥ 60, otherwise healthy – GOAL ˂ 150/90 – Patients 30-59, otherwise healthy – GOAL ˂ 140/90 – Lifestyle modifications • JNC 10 – Patients ≥ 65, otherwise healthy – GOAL ˂ 140/90 – Patients ˂ 65, otherwise healthy – GOAL ˂ 130/80 – Lifestyle modifications Drug Selection • First line agents: – Thiazide diuretics – ACE/ARBs – CCBs • Choice dependent on numerous factors, including age, ethnicity, concomitant CV/kidney disorders. HTN Management Guidelines • Factors to be considered: age, ethnicity, concomitant CV disorders. • Start medications in lowest available dose. • Change medication groups instead of increasing the dose if 1st medication is ineffective. • Many patients require 2+ medications for adequate BP control. • Medications are titrated and dispensed according to individual response. • Patient Teaching Box: 26.4 (Page 521) Antihypertensive Medications (Table 26.1, Page 515) Angiotensinconverting enzyme (ACE) inhibitors Angiotensin II receptor blockers (ARBs) Antiadrenergics Calcium channel blockers Diuretics Direct vasodilators ACE Inhibitors ACE Inhibitors (-prils) • Angiotensin-Converting Enzyme Inhibitors • MOA: Block the conversion of angiotensin I to angiotensin II (potent vasoconstrictor) – Decreased aldosterone production = reduced retention of Na and H2O • Metabolism highly dependent on genetics and ethnicity • Current guidelines: ALL nonblack individuals, including those with DM or CKD, should receive ACEI as part of their drug therapy. • Not as effective in African American populations ACE Inhibitors (-prils) captopril (Capoten)* benazepril (Lotensin) enalapril (Vasotec) fosinopril (Monpril) ramipril (Altace) Lisinopril (Zestril) ACE Inhibitor MOA on RAAS BP LOW Renin secreted from kidneys Renin stimulates increased conversion of angiotensinogen to angiotensin I Angiotensin I converted to angiotensin II by angiotensin-converting enzyme (ACE) Angio II causes vasoconstriction & stimulates release of aldosterone Aldosterone causes Na and H2O retention B/P rises Renin release is inhibited Side/Adverse Effects • Dry, persistent cough – May warrant D/C • First dose orthostatic hypotension • ANGIOEDEMA • Hyperkalemia • Worsening renal function…check BUN/Cr frequently A: Angioedema C: Cough E: Electrolytes Nursing Implications • • • • • BBW: Not to be used during pregnancy – TERATOGENIC – Cautious use in women of childbearing age QSEN Safety (p. 519): ACE + K sparing diuretics or foods high in K increases risk for hyperkalemia – Foods high in K: bananas, oranges, salt-substitutes, potatoes, almonds BP checks – orthostatic hypotension (worsened with 1st dose) – Check BP for 2 hours after 1st dose – Take first dose at bedtime – Change positions slowly – Avoid hot showers/saunas Monitor BUN/Cr baseline and routinely Do not take captopril with meals, if possible – 1 hr before or 2 hrs. after meals ARBs ARBs (-tans) • Angiotensin II Receptor Blockers • MOA: Blocks vasoconstricting and aldosterone secreting effects of angiotensin II at various receptor sites. – Increases renal flow and enhances excretion of chloride, calcium, magnesium, and phosphate. • Well-tolerated with less AE than ACEI – Less profound effect on K – No dry cough – Can take with/without meals • AE: Angioedema, impaired renal function (BUN/Cr) • BBW: Women of childbearing age/Pregnancy - TERATOGENIC ARBs (-tans) losartan (Cozaar) irbesartan (Avapro) valsartan (Diovan) olmesartan (Benicar) ARB MOA on RAAS BP LOW Renin secreted from kidneys Renin stimulates increased conversion of angiotensinogen to angiotensin I Angiotensin I converted to angiotensin II by angiotensin-converting enzyme (ACE) Angio II causes vasoconstriction & stimulates release of aldosterone Aldosterone causes Na and H2O retention B/P rises Renin release is inhibited Calcium channel blockers CCBs (-pines) • Calcium Channel Blockers • MOA: Inhibit the influx of calcium ions across cardiac and smooth muscle cells, resulting in relaxation and vasodilation. • Negative inotrope • Also used in treatment of CAD/angina – Prinzmetal angina CCBs (-pines) amlodipine (Norvasc) nicardipine (Cardene) felodipine (Plendil) diltiazem (Cardizem) verapamil (Calan) nifedipine (Procardia) Indications for Use • HTN, Angina, CAD • SVT Dysrhythmias (diltiazem) • Subarachnoid hemorrhage/cerebral aneurysm…..Nimotop (nimodipine) • Raynaud’s phenomenon • Hypertrophic cardiomyopathy Side/Adverse Effects • Generally well-tolerated • CV effects: – Slowed HR/contractility – Hypotension – Peripheral edema of hands, ankles, feet – Pulmonary edema – Worsened in patients with HF – QSEN Safety: Anginal exacerbation (abrupt withdrawal) • Other: H/A, drowsiness, fatigue, dizziness, flushing, palpitations, nausea, abdominal pain. Drug/Food Interactions • Do not give with grapefruit juice…inhibits first pass liver metabolism…will have higher serum levels and lead to toxicity • Increased serum levels of (-statin) drugs • Don’t give in IV form with beta blockers at the same time • Can increase serum digoxin levels – Digoxin + CCB = risk of heart blocks Beta blockers Beta Blockers (-lols) • MOA: Inhibits Beta1 and/or Beta2 receptors • Work on the SNS (sympathetic nervous system) – Decreasing overall stimulation – Negative inotrope and chronotrope effect – Decreased renin release from kidneys • Decreases the 3 Cs!! + 1 more…. And maybe +1 more Beta Blockers (-lols) • Types: – Selective – drugs that inhibit only one type of beta receptor • Beta1 only: cardioselective • Beta2 only: block lung receptors – Nonselective: Block both – Alpha AND BetaBlockers Beta Blockers (-lols) atenolol (Tenormin) bisoprolol (ApoBisoprolol) metoprolol (Lopressor) carvedilol (Coreg) propanolol (Inderal) Indications for Beta Blocker Use • • • • Hypertension Angina Dysrhythmias Hypertrophic Cardiomyopathy • Glaucoma (topical) • Tremors & Anxiety • Vascular Headaches (migraines) • Adjunct use in: – Thyrotoxicosis – Pheochromocytoma Side/Adverse Effects • • • • Primarily extensions of their pharmacologic activity CV effects: – Negative chronotropy (Bradycardia!) – Hypotension – Heart failure exacerbation – BBW: Anginal exacerbation (with abrupt withdrawal) Non-CV effects: – Bronchospasm – Depression exacerbation – Decline in sexual function – Weakness/Fatigue (why??) – Masking of hypoglycemia Remember these are all “high alert” drugs! – Second nurse should check calculations for correct dosing when giving IV Contraindications/Cautious Use • AV Block • Bradycardia • Uncompensated Heart Failure…and use cautiously with all HF • Asthma, COPD – use cardio-selective drugs only • Cautious use with DM, MG, depression Nursing Implications • • • • • Check HR!!! – Hold and notify HCP for a HR ˂ 60 bpm – Apical pulse x 1 FULL minute – Teach patient how to check their pulse daily Check B/P!!! – Hold and notify HCP for SBP < 90 mmHg IVP given over 2.5 minutes. – Continuous telemetry – 2nd RN verification – BP monitoring every 5 minutes – Supine/HOB flat Daily weights, check for edema Wean drugs off over 1-2 weeks Drug – Drug Interactions • Careful with CCBs….added bradycardic effect! • Anti-diabetic agents: mask s/sx of hypo- and hyperglycemia • Cocaine: reduce or cancel effects of beta blockers • MAOIs (monoamine oxidase inhibitors): can cause hypertensive crisis • OTC drugs Combined alpha and beta blockers • carvedilol (Coreg) and labetalol (Normodyne) • MOA: Same as nonselective beta blockers, but work on alpha-receptors too = increased vasodilation • May have more orthostatic hypotension – Supine/HOB flat with IVP administration! • carvedilol (Coreg) is used primarily for CHF, but works for HTN as well • carvedilol (Coreg) can increase Digoxin levels • carvedilol (Coreg) may also cause drug-induced SLE Anti-adrenergics Centrally-acting Alpha Agonists • • • • • • Alpha2 Receptor Agonists MOA: Stimulates alpha2 receptors in the brain, which blocks SNS activity and leads to the release of less norepinephrine and a reduction of sympathetic outflow from the vasomotor center. – Decreases BP Other indications for use: chronic pain treatment. clonidine (Catapres) – Can be PO or a weekly TTS patch – May slow HR Adverse effects: orthostatic hypotension, bradycardia, decreased sexual function, drowsiness, rebound HTN (taper off slowly) Since these work on decreasing activity in the CNS, watch out for other CNS depressants! Peripherally-acting Alpha-Adrenergic Blockers • Alpha1-Adrenergic Blockers • MOA: Block peripheral alpha1-adrenergic receptors, resulting in blood vessel dilation and decreased PVR. • Peripheral acting – AE firstdose phenomenon – Orthostatic hypotension – 1-3 hours after 1st dose – Give first dose at bedtime to prevent. doxazosin prazosin terazosin Direct Renin Inhibitors • aliskiren (Tekturna) • MOA: Decreased plasma renin activity and inhibits conversion of antiotensinogen to angiotensin I. • Contraindicated with ACE/ARB and CKD • Not to be taken with high-fat meal – absorption of drug effected 75% • AE: Angioedema/Hyperkalemia Diuretics • Thiazide: 1st line drug class for HTN. • All decrease plasma and extracellular fluid volumes causing decreased preload…which causes decreased CO and decreased SVR Thiazides: (hydrochlorothiazide) Loop: (furosemide) K-sparing: (spironolactone) K-sparing Diuretics • MOA: Block aldosterone (thereby sparing potassium!) • Examples: – spironolactone (Aldactone) – eplerenone (Inspra) • Nursing Implications: Electrolytes! I&O Direct Vasodilators • MOA: Directly relax smooth muscle in the blood vessels, resulting in dilation and decreased PVR. • Effective in HTN emergencies and management of HF. • BBW: minoxidil – anginal exacerbation – preceipitated pericardial effusion • Watch for drug-induced Lupus Erythematosus, Na retention (edema), tachycardia nitroprusside hyralazine minoxidil dopamine (Intropin) • Opposite of previous drugs • vasopressor…makes B/P and CO rise • Can also be given at a low “renal” dose to improve renal and mesenteric blood flow…to improve kidney perfusion (1-2mcg/kg) • Given in ICU • SE: HA, nausea, angina, HTN, Tachycardia Final Tid-Bits….. • Patients may be on several classes of drugs to achieve a therapeutic B/P • More classes = more difficulty controlling B/P • Never give 2 of the same class without clarifying order!!! • Patient Teaching – What do your patients need to know to take their medications safely?? What if… • The antihypertensive drugs your patient received have bottomed out his B/P to 70/40. What would you do?