Newer Antihypertensive Drugs BushraAbdul Hadi Philadelphia University
advertisement

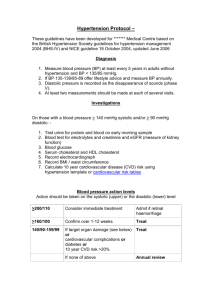
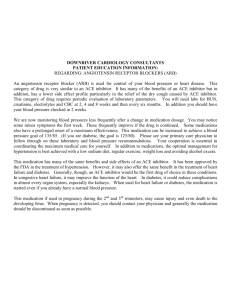
Newer Antihypertensive Drugs BushraAbdul Hadi Philadelphia University Hypertension: A Significant CV and Renal Disease Risk Factor CAD CHF LVH Stroke Hypertension Morbidity Renal disease Disability Peripheral vascular disease National High Blood Pressure Education Program Working Group. Arch Intern Med. 1993;153:186208. “Older generation drugs used to bring down the B.P. fairly well at reasonable cost.” Then, Why do we need new drugs ? • Observational and limited controlled trials then showed marginal benefits of BP lowering for CVAs and IHD • Unfriendly dosing schedule • Unpleasant side effects Vasculopathy continuum CAD Risk Factors CKD CHF CVA PAD Endothelial Dysfunction HTN Metabolic syndrome Na+ Handling Sympathetic N system RAAS Hypertension Genetics Environment Psycho-social HTN : Old and New • • • • Diuretics Reserpine Guanethidine Alpha Methyl Dopa ACE Inhibitors Angiotensin Receptor Blockers Beta Blockers Central Alpha Agon. Calcium Channel Blockers Diuretics Direct Vasodilators Aldosterone Anta. NEP Blockers Potential Pathogenic Properties of Angiotensin II Heart – Myocardial hypertrophy – Interstitial fibrosis Coronary Arteries – Endothelial dysfunction with decreased release of nitric oxide – Coronary constriction via release of norepinephrine – Formation of oxygen-derived free radicals via NADH (nicotinamide adenine dinucleotide) oxidase – Promotion of inflammatory response and plaque instability – Promotion of low-density lipoprotein cholesterol uptake Adapted from Opie and Gersh. Drugs for the Heart, 2001. Potential Pathogenic Properties of Angiotensin II (continued) Kidneys – – – – – Increased intraglomerular pressure Increased protein leak Glomerular growth and fibrosis Increased sodium reabsorption Decreased renal blood flow Adrenal Glands – Increased formation of aldosterone Coagulation System – Increased fibrinogen – Increased PAI-1 (plasminogen activator inhibitor-1) relative to tissue plasminogen factor Adapted from Opie and Gersh. Drugs for the Heart, 2001. The Renin-Angiotensin-Aldosterone (RAA) System Kidneys Liver secretes secrete angiotensinogen renin Blood Adrenal cortex secretes aldosterone Renin Angiotensinogen Growth factor stimulation Angiotensin converting enzyme (ACE) Angiotensin I Sympathetic activation Angiotensin II Vascular smooth muscle constriction Aldosterone NA+ retention H2O retention K+ excretion Mg+ excretion RAA System Pathways to Target Receptor Sites Na+ Angiotensinogen K+ Aldosterone Adrenal Renin Other Chymase Angiotensin I CE Bradykinin Vascular Angiotensin II Inactive Myocardial Renal CNS ACTH LIFE: Primary and Select Secondary Outcomes Adjusted* Losartan Atenolol (n=4,605) (n=4,588) RR (%) p-value Primary composite† 508 588 -13 .021 CV mortality 204 234 -11 .21 Stroke 232 309 -25 .001 MI 198 188 +7 .49 383 431 -10 .13 Total mortality * For degree of LVH and Framingham risk score at randomization † Number of onset patientsDM with event ‡ a first primary New 241 319 -25 <.001 ‡ In patients without diabetes at randomization (losartan, n=4,019; atenolol, Adapted from B Dahlöf et al. Lancet. 2002;359:995-1003. n=3,979) HOPE: Risk Reduction of CV Events Associated with ACEI (RAS Inhibition) Treatment 0 MI, Stroke, CV Death (primary end point) CV Death MI Stroke All-cause Death Risk Reduction (%) -5 -10 -15 -20 -25 -30 -35 -22 (P<.001) -16 (P=.005) -20 (P<.001) -26 (P<.001) -32 (P<.001) Adapted from The Heart Outcomes Prevention Evaluation Study Investigators. Effects of an angiotensinconverting enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J Med. 2000;342:145-153. Mechanism of Action of Angiotensin II Receptor Antagonists Angiotensinogen Bradykinin ACE inhibitors Alternate pathways Angiotensin I Angiotensin II Inactive peptides AIIRAs ? AT1 receptor ? Vasodilation Attenuate growth and disease progression Val-HeFT Results • Overall mortality was similar in the two groups • 13% RRR (p=.009) in combined end point • Predominantly because of a 27% decrease in hospitalization for HF in the valsartan group • Subgroup analyses: – Valsartan had a favorable effect in patients receiving neither an ACE inhibitor nor a betablocker – Valsartan had a favorable effect in patients receiving an ACE inhibitor or a beta blocker – Valsartan demonstrated a statistically nonsignificant trend towards an adverse outcome in ADA Guidelines on Management of Diabetic Nephropathy Hypertensive Type 2 Diabetic Patients* ARBs are the initial agents of choice Type 1 Diabetics with or without hypertension* ACEIs are the initial agents of choice If one class is not tolerated the other should be substituted * With microalbuminuria and clinical proteinuria. Adapted from American Diabetes Association. Diabetes Care. 2002;25:S85-S89. Progression to Death, Dialysis, or Transplant (%) Effect of ACE Inhibition on Nephropathy in Type 1 Diabetes 40 30 Placebo 20 * 10 0 0 1 2 Follow-up (y) * P=.006 vs placebo. Adapted from Lewis EJ et al. N Engl J Med. 1993;329:1456-1462. 3 4 Captopril ACE Inhibitors and ARBs • • • • • • Captopril Enanlapril Lisinopril Ramipril Perindopril Quinapril Losartan Irbesartan Candesartan Valsartan Telmisartan Olmesartan Aliskiren Proven role of Beta Blockers in Various Indications - Hypertension - Diabetes Mellitus - CHF - CAD Effect of Beta-Blockers on mortality following myocardial infarction 23 No diabetes mellitus, all Diabetes mellitus, all 20 17 15 10 13 10 10 7 5 0 No diabetes mellitus, no beta-blocker No diabetes mellitus, beta-blocker Diabetes mellitus, no beta-blocker Diabetes mellitus, beta-blocker Kjekshus J et al. Eur Heart J 1990; 11: 43-50 1 year-mortality (%) 25 Survival rate 1.00 0.95 0.90 0.85 0.80 With ß-blockers Without ß-blockers P= 0.0001 0.75 1 2 Year 3 4 5 Jonas et al. Am J Cardiol 1996; 77: 1273 et seqq. Usefulness of beta-blocker therapy in patients With Diabetes Mellitus and CAD (BIP) Effect of Beta-Blockers on Mortality in Heart Failure Patients Trial End Point Risk Reduction, % (95% CI) US Carvedilol Combined end point: risk of hospitalization or death 38% lower risk (18%-53%) P< 0.001 CIBIS-II (bisoprolol) All-cause mortality 34% lower risk P< 0.0001 MERIT-HF (metoprolol) All-cause mortality 34% lower risk (0.53– 0.81) P=0.0062 after adjusted interim analysis BEST (bucindolol) All-cause mortality 8.5% lower risk P=NS COPERNICUS (carvedilol) All-cause mortality 35% lower risk* Clinical Trial *Preliminary data from XXII Congress of the European Society of Cardiology Effects of Metoprolol CR and Placebo on Neurohormonal Activation Placebo 250 225 225 200 175 182 200 165 175 150 128 125 105 150 125 100 100 75 75 50 Metoprolol 250 35.9 38.9 50 25 25 0 0 Plasma Angiotensin Aldosterone renin ng/ml II pg/ml pg/ml Baseline 24 weeks The Resolvd Investigators. 1999. NS * 147 129 113 99 * 34.3 30.9 Plasma Angiotensin Aldosterone renin ng/ml II pg/ml pg/ml Baseline 24 weeks *P<0.05 NS: Non Significant Effect of -Blocker in Heart Failure Mega-trials on: metoprolol, bisoprolol, carvedilol & bucindolol. Consistent good results in mild / moderate HF. Significant ↓ in rate of hospitalisation. Fair improvements in symptoms & QOL. Improvements in hemodynamics of HF & remodeling. Results in severe HF are not uniform. Bucindolol in BEST showed no benefits. Sub-analysis of CIBIS-II (Bisoprolol) & MERIT-HF: ↓ benefits in more severe HF. COPERNICUS: significant benefits in severe HF. Lipophilic beta blockers are an ideal choice in patients at high risk of SCD, prior MI, HT,CHF Beta Blockers • • • • • Propranolol Atenolol Metoprolol( Sustained Release) Bisoprolol Carvedilol ALLHAT Diuretics Because of the superiority of thiazide-type diuretics in preventing one or more major forms of CVD and their lower cost, they should be the drugs of choice for first-step antihypertensive drug therapy. Hydrochlorthiazide Metolazone Furosemide Torsemide Amiloride Calcium Channel Blockers Very effective in lowering BP Safe OD or BID Dose No significant outcome benefits Peripheral edema Nifedipine(Long Acting) Amlodepine Verapamil Nicardepine Lercanidipine Felodepine Miscellaneous • Direct Vasodilators – Dihydrallazine – Minoxidil – Prazosin • Central Alpha Agonists – Clonidine – Moxolidine • Aldosterone antagonists – Spironolactone – Eplerenone • Indapamide Benefits of Lowering BP Average Percent Reduction Stroke incidence 35–40% Myocardial infarction 20–25% Heart failure 50% U.S. Department of Health and Human Services National Institutes of Health National Heart, Lung, and Blood Institute National Heart, Lung, and Blood Institute National High Blood Pressure Education Program The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) Blood Pressure Classification BP Classification Normal SBP mmHg <120 DBP mmHg and <80 Prehypertension 120–139 or 80–89 Stage 1 Hypertension Stage 2 Hypertension 140–159 or 90–99 >160 or >100 Compelling Indications for Individual Drug Classes Compelling Indication Initial Therapy Clinical Trial Basis Heart failure THIAZ, BB, ACEI, ARB, ALDO ANT ACC/AHA Heart Failure Guideline, MERIT-HF, COPERNICUS, CIBIS, SOLVD, AIRE, TRACE, ValHEFT, RALES BB, ACEI, ALDO ANT ACC/AHA Post-MI Guideline, BHAT, SAVE, Capricorn, EPHESUS THIAZ, BB, ACE, CCB ALLHAT, HOPE, ANBP2, LIFE, CONVINCE Postmyocardial infarction High CAD risk Compelling Indications for Individual Drug Classes Compelling Indication Initial Therapy Clinical Trial Basis Options THIAZ, BB, ACE, ARB, NKF-ADA Diabetes Guideline, UKPDS, CCB ALLHAT Chronic kidney ACEI, ARB NKF Guideline, disease Captopril Trial, RENAAL, IDNT, REIN, AASK Recurrent stroke THIAZ, ACEI PROGRESS prevention Cardiovascular Diseases • Cerebrovascular disease –Indication for treatment, except immediately after ischemic cerebral infarction. • Coronary artery disease –Benefits of therapy well established. • Left ventricular hypertrophy –Antihypertensive agents (except direct vasodilators) indicated. –Reduced weight and decreased sodium intake beneficial. Cardiovascular Diseases (continued) • Cardiac failure –ACE inhibitors, especially with digoxin or diuretics, shown to prevent subsequent heart failure. • Peripheral arterial disease –Limited or no data available. New Features and Key Messages For persons over age 50, SBP is a more important than DBP as CVD risk factor Starting at 115/75 mmHg, CVD risk doubles with each increment of 20/10 mmHg throughout the BP range. Persons who are normotensive at age 55 have a 90% lifetime risk for developing HTN. Those with SBP 120–139 mmHg or DBP 80–89 mmHg should be considered prehypertensive who require health-promoting lifestyle modifications to prevent CVD. JNC-VII New Features and Key Messages (Continued) Thiazide-type diuretics should be initial drug therapy for most, either alone or combined with other drug classes. Certain high-risk conditions are compelling indications for other drug classes. Most patients will require two or more antihypertensive drugs to achieve goal BP. If BP is >20/10 mmHg above goal, initiate therapy with two agents, one usually should be a thiazide-type diuretic. Preventable CHD Events from Control of Hypertension in US Adults (Wong et al., Am Heart J 2003; 145: 888-95) (cont.) • The greatest impact (absolute numbers) from control of hypertension occurs in men, older persons, and those with isolated systolic hypertension • The greatest proportion of preventable CHD events from control of hypertension occurs in women • Optimal control of blood pressure could prevent more than one third of CHD events in men and more than half of CHD events in women Evolution of Antihypertensive Therapies Effectiveness Tolerability 1940’s 1950 1960’s 1957 -blockers Direct vasodilators Peripheral sympatholytics Ganglion blockers Veratrum alkaloids 1970’s 1980’s ARBs ACE inhibitors Thiazides diuretics Central 2 agonists Calcium antagonistsnon DHPs blockers 1990’s Calcium antagonistsDHPs 2001 VPIs Others We are still evolving towards finding an Ideal Antihypertensive Preventable CHD Events from Control of Hypertension in US Adults (Wong et al., Am Heart J 2003; 145: 888-95) 56 60 PAR% / NNT 50 39 37 40 31 30 20 21 21 19 11 10 0 Men PAR% Women PAR% Treatment to <140/90 mmHg Men NNT Women NNT Treatment to <120/80 mmHg PAR% = population attributable risk (proportion of CHD events preventable), NNT = number needed to treat to prevent 1 CHD event ; <0.01 comparing Compelling Indications for Certain Drug Classes HTN with CAD Beta blockers: cardioprotective (reinfarction, arrhythmias and sudden death) ACE inhibitors: MI with systolic dysfunction- heart failure and mortality improved Aliskiren is a novel, completely nonpeptide, orally active renin inhibitor that blocks the first and rate-limiting step of the reninangiotensin system Alagebrium, an advanced glycation end product (AGE) crosslink breaker, has been shown to reduce SBP in patients with uncontrolled systolic hypertension, progestin drospirenone and 17beta-estradiol (DRSP/E2), developed for postmenopausal hormone replacement therapy, has been shown to lower both clinic and ambulatory SBP in postmenopausal women Pathophysiology of Heart Failure Cardiac injury Increased load Activation of RAA System, SNS, and cytokines Reduced systemic perfusion Altered gene expression Growth and remodeling Ischemia and energy depletion Apoptosis Necrosis Cell death Adapted from: Eichhorn EJ, Bristow MR. Circulation. 1996;94:2285-2296. Direct toxicity Pathogenesis of HT Reasons are mulitfactorial.. Vasoconstriction Renin Angiotensin II Angiotensin I Increased Na+ & water reabsorption Summary