Pediatric Cardiac Disorders: Congenital & Acquired Heart Disease
advertisement
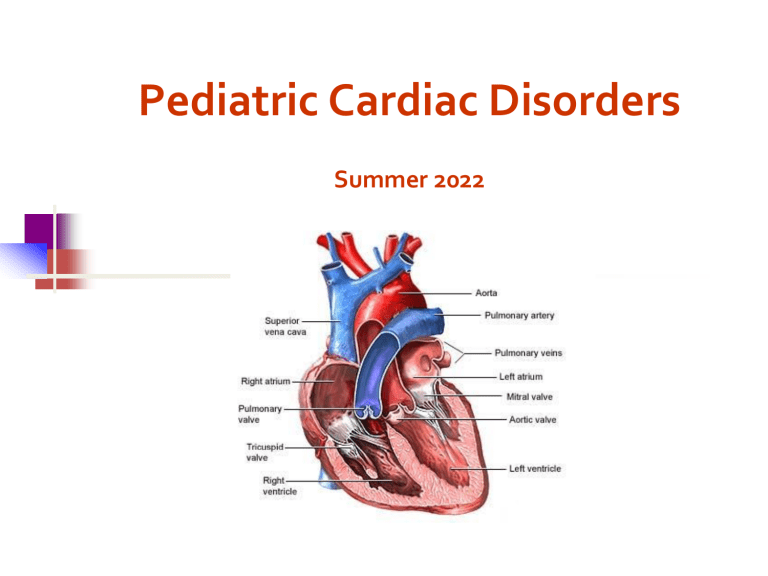
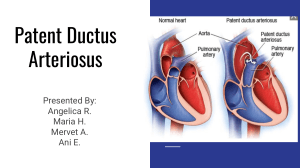
Pediatric Cardiac Disorders Summer 2022 Review of the Heart Normal cardiac anatomy and physiology Muscular pump divided into four chambers Upper chambers are atria Lower chambers are ventricles Atria are the filling chambers Ventricles are the pumping chambers Two atrioventricular (AV) valves (Tricuspid & Mitral), two semilunar valves (Pulmonic & Aortic) Mechanical contraction of the heart begins with electrical stimulation Copyright © 2018 Elsevier Inc. All rights reserved. 2 Fetal Circulation Intrauterine to Extrauterine 1. Infant takes first breath and the lungs inflate __decreased___ pulmonary vascular resistance Increased pulmonary blood flow & the pulmonary artery pressure increases. 2. Increased pressure in left atrium, decreases pressure in right atrium closure of foramen ovale 3. The ductus arteriosus and ductus venosus close related to pressure changes and blood oxygen levels. Fun Fetal Circulation Video https://www.youtube.com/watch?v=3IkAnVZp O5Y Other helpful videos: Fetal circulation: https://www.youtube.com/watch?v=-IRkisEtzsk Circulation right after birth https://www.youtube.com/watch?v=jFn0dyU5wUw RECAP: Transitional and Neonatal Circulation Major changes in the circulatory system occur at birth after the first breath. Gas exchange is transferred from the placenta to the lungs. Fetal shunts close. Resistance to flow in the pulmonary system decreases as systematic resistance increases. Pulmonary vascular resistance decreases. Marked increase in pulmonary blood flow follows. Copyright © 2018 Elsevier Inc. All rights reserved. Oxygen Saturation What is oxygen saturation? Fraction of O2 saturated hemoglobin relative to total hemoglobin in the blood What is normal oxygen saturation levels? 95-100% What values indicate hypoxemia? Why is it important for the nurse to know the oxygen saturation levels? Congenital Heart Disease Left-to-right shunting lesions Patent ductus arteriosus Atrial septal defect Ventricular septal defect Atrioventricular septal defect Obstructive or stenotic lesions Pulmonary stenosis Aortic stenosis Coarctation of the aorta Copyright © 2018 Elsevier Inc. All rights reserved. Congenital Heart Disease (Cont.) Cyanotic lesions with decreased pulmonary blood flow Tetralogy of Fallot Tricuspid atresia Pulmonary atresia with intact ventricular septum Cyanotic lesions with increased pulmonary blood flow Truncus arteriosus Hypoplastic left heart syndrome Transposition of the great arteries Copyright © 2018 Elsevier Inc. All rights reserved. Patent Ductus Arterious Atrial septal defects Ventricular septal defects Patent Ductus Arteriosus 1. Blood shunts from aorta (left) to the pulmonary artery (right) 2. Returns to the lungs causing increase pressure in the lung 3. Congestive heart failure PDA Treatment Medical Management Medication Indomethacin - given IV. Inhibits prostaglandins by inhibiting cyclooxygenase. (When levels of prostaglandins are decreased, the ductus closes) Used mainly in preterm infants. Surgery - video-assisted thoracoscopic Ligate the ductus arteriosus PDA Treatment Cardiac Catheterization Insert coil – tiny fibers occlude the ductus arteriosus when a thrombus forms in the mass of fabric and wire Atrial Septal Defect 1. Oxygenated blood is shunted from left to right side of the heart via defect 2. A larger volume of blood than normal must be handled by the right side of the heart hypertrophy 3. Extra blood then passes through the pulmonary artery into the lungs, causing higher pressure than normal in the blood vessels in the lungs congestive heart failure ASD Treatment Medical Management Cardiac Catheterizaton Medications – digoxin Amplatzer septal occluder Open-heart Surgery ASD Treatment Device Closure – Amplatzer septal occluder During cardiac catheterization the occluder is placed in the Defect Ventricular Septal Defect 1. Oxygenated blood is shunted from left to right side of the heart via defect 2. A larger volume of blood than normal must be handled by the right side of the heart hypertrophy 3. Extra blood then passes through the pulmonary artery into the lungs, causing higher pressure than normal in the blood vessels in the lungs congestive heart failure VSD Treatment Surgical repair with a patch inserted Pulmonic Stenosis Aortic Stenosis Coarctation of Aorta Pulmonic Stenosis Narrowing of entrance that decreases blood flow Increases preload causes right ventricular hypertrophy Obstructive or Stenotic Lesions Treatment: Medications – Prostaglandins to keep the PDA open Cardiac Catheterization Balloon Valvuloplasty Surgery Valvotomy Aortic Stenosis The aortic valve is thickened and rigid Stenosis creates left ventricular hypertrophy Left ventricle may not be large enough to eject a normal cardiac output. Aortic Stenosis Symptoms Poor peripheral perfusion, feeding difficulties, CHF Treatment Balloon valvoplasty Surgery Coarctation of the Aorta 1. Narrowing of Aorta causing obstruction of left ventricular blood flow 2. Left ventricular hypertrophy Signs and Symptoms 1. What are B/P findings support the diagnosis? Elevated B/P 2. What is different when assessing pulses? Absent leg pulses (hallmark) and a difference in blood pressure between the arms and legs. High in arms and low to normal blood pressure in legs. 3. Why would the patient C/O leg pains? Poor peripheral perfusion 4. What causes nose bleeds? Elevated B/P Treatment Goals of management are to improve ventricular function and restore blood flow to the lower body. Medical management with Medication A continuous intravenous medication, prostaglandin (PGE-1), is used to open the ductus arteriosus allowing blood flow to areas beyond the coarctation. Baloon Valvoplasty Surgery for Coarctation of Aorta 1. Resect narrow area 2. Anastomosis Tetralogy of Fallot Tetralogy of Fallot (TOF) Four defects are: 1. 2. 3. 4. TOF Signs and Symptoms 1. Failure to thrive 2. Squatting 3. Lack of energy 4. Infections 5. Polycythemia 6. Clubbing of fingers 7. Cerebral abscess 8. Cardiomegaly Think Like a Nurse What is the relationship between polycythemia and a cardiac disorder? What is the worst possible complication to anticipate based on the polycythemia? What nursing interventions are included when planning care for this child? When you see the RBC’s elevated – what other lab work would you want to check? What lab work would need to be trended? Ask Yourself ? Laboratory analysis on a child with Tetralogy of Fallot indicates a high RBC count. The polycythemia is a compensatory mechanism for: a. Tissue oxygen need b. Low iron level C. Low blood pressure d. Cardiomegaly Hypercyanotic Episode / “tet” spells Cyanosis/ hypoxia suddenly worsens in response to activity, such as crying, feeding, or having a bowel movement. Signs - The infant becomes very short of breath with tachypnea and hyperpnea, and may lose consciousness. Treatment – calming, knee-chest position, oxygen, morphine , and beta-blockers p. 1088 Treatment Open-heart Surgical interventions Blalock – Taussig or Potts procedure – increases blood flow to the lungs. Something the Lord Made View the Movie Trailer About Blalock procedure to treat Tetralogy of Fallot https://www.youtube.com/watch?v=eUf OvjNTM2M • • Truncus Arteriosus Transposition of Great Vessels These present the greatest risk to survival Truncus arteriosus A single arterial trunk arises from both ventricles that supplies the systemic, pulmonary, and coronary circulations. A vsd and a single, defective, valve also exist. Entire systemic circulation supplied from common trunk. Transposition of Great Vessels Aorta arises from the right ventricle, and the pulmonary artery arises from the left ventricle - which is not compatible with survival unless there is a large defect present in ventricular or atrial septum. artery aorta Review of CHD A 3-month-old has been diagnosed with a VSD. The flow of blood through the heart with this type of defect is: A. Right to left B. Equal between the two chambers C. Left to right D. Bypassing the defect Acquired Heart Diseases Infective endocarditis Dysrhythmias Rheumatic fever Kawasaki disease Hypertension Cardiomyopathies High cholesterol levels Copyright © 2018 Elsevier Inc. All rights reserved. A systemic inflammatory (collagen) disease of connective tissue that usually follows a group A beta-hemolytic streptococcus infection. This disorder causes changes in the entire heart (especially the valves), joints, brain, and skin tissues. Rheumatic Fever - Assessment Major Carditis Arthritis Chorea Erythema marginatum Subcutaneous nodules Jones Criteria Minor Arthralgia Fever Laboratory Findings: Erythrocyte sedimentation rate C-reactive protein Prolonged PR interval p. 1109 Fig 46.2 What is most common sign? Most serious? What additional laboratory tests help to confirm the diagnosis of Rheumatic Fever ? C-Reactive Protein and Erythrocyte Sedimentation Rate (ESR) Rheumatic Fever Treatment Antibiotic Therapy Anti-inflammatory agents – steroids Antipyretics – aspirin Rest Heat and cold to joints Discharge Teaching Antibiotic therapy - be sure to complete all medication Streptococcal Prophylaxis for the Child with Rheumatic Fever Damaged valves can become further damaged with repeated infections Streptococcal prophylaxis is lifelong if there is actual valve involvement Intramuscular penicillin, administered monthly, is the drug of choice Alternatives include oral penicillin twice daily or oral sulfadiazine once a day Multisystem vasculitis – inflammation of blood vessels in the body, especially the coronary arteries, with antigen-antibody complexes Kawasaki Disease Mucocutaneous lymph node syndrome Acute, febrile, exanthematous (maculopapular) illness Generalized vasculitis of unknown etiology Major cause of acquired heart disease Cause remains unknown Coronary artery aneurysms are seen in 20– 25% of children left untreated Copyright © 2018 Elsevier Inc. All rights reserved. Signs and Symptoms / Treatment Three Phases of clinical manifestations: Acute Subacute Convalescent What is one of the most common symptoms used to diagnose Kawasaki disease? • • • • Temp: > 101.3 F, lasts more than 3 days Extremely red eyes with thick discharge Rash on main part of body and in genital area Red, dry, cracked lips and an extremely red, swollen tongue (Strawberry Tongue) Acute Phase – 1-10 days Fever, often higher than 101.3 F, lasting one - two weeks Extremely red eyes (conjunctivitis) without thick discharge Red, dry, cracked lips and an extremely red, swollen tongue ("strawberry" tongue) Rash on the main part of the body (trunk) and in the genital area Swollen, erythema on the palms of the hands and the soles of the feet Swollen cervical lymph nodes Kawasaki Disease Images Erythematous rash of Kawasaki disease. (From Lookingbill, D.P., & Marks, J.G., Jr. [1992]. Principles of dermatology [2nd ed., pp. 223]. Philadelphia: Saunders.) Copyright © 2018 Elsevier Inc. All rights reserved. Subacute Phase 11-25 days Irritability Anorexia Desquamation of the skin on the hands and feet, especially the tips of the fingers and toes, often in large sheets Arthritis and Arthralgia Arrhythmias Thrombocytosis -Coronary aneurysms Convalescent Phase Day 26 - until the erythrocyte sedimentation rate returns to normal Nursing Care Give Medications Promote comfort and hydration Aspirin Intravenous Immunoglobulin Lubricate the lips Cool compresses or sponge baths Keep skin cool and dry Small feedings of soft, non-acidic foods, and liquids that are not too hot Facilitate joint movement Passive Range of Motion exercises Kawasaki Disease Which phase of Kawasaki is this child exhibiting? Inflamed, Cracked, Peeling Lips Strawberry tongue Kawasaki Disease Hint: Heart Failure What is wrong with the heart? Unable to circulate blood sufficient to maintain metabolic demands of the body Heart Failure Why does the pump fail? Etiology and Pathophysiology Heart Failure What does the body do to compensate for this congestion and heart failure? See box on p. 1083 Heart failure What is the effect on: Heart rate Contractility Afterload Kidneys Preload Compensatory Mechanisms Brain O2 Renal blood flow GFR Increase heart rate Stimulation of renin, Angiotension system Afterload Na and H2O Intravascular volume vasoconstriction Systemic vascular resistance Myocardium stretches Increase contractility Hypertrophy Preload Early Signs of CHF The earliest signs are often subtle: Infants: tachypnea, difficulty feeding Children: Dyspnea, tachypnea, decreased energy What are the most common signs that the family or nurse would report? 1. 2. 3. Clinical Manifestations Signs of respiratory distress Wheezing, rales and rhonchi Tachycardia Extremities cool, capillary refill >2 seconds Diaphoretic, sweating, hypotension Hepatomegaly Edema with fluid weight gain Failure to thrive Exercise intolerance Clinical Manifestations cont’d Difficulty feeding, poor weight gain Mild tachypnea, tachycardia Cardiomegaly Galloping rhythm Poor perfusion, edema Liver and spleen enlargement Mottling, cyanosis, pallor Copyright © 2018 Elsevier Inc. All rights reserved. Goal of Treatment Stroke volume (SV): Liters/min blood ejected from heart with each heartbeat. Cardiac Output (CO): SV X HR = CO Treatment of Heart Failure Medication Therapy Digitalis – strengthens force contractility and decreases heart rate. Beta Blocker - increases contractility ACE-inhibitors - blocks release of angiotensionaldosterone; arterial vasodilator / afterload reducing agent Diuretics - enhance renal secretion of sodium and water by reducing circulating blood volume and decreasing preload, pulmonary congestion. CHF is B(eta blockers) A(ce inhibitors) D(iuretics) Digitalis Digitalization Obtain baseline ECG before initiating Digoxin Given in divided doses over 12-18 hrs Check serum electrolytes Assess vital signs and quality of peripheral pulses Maintenance Given daily, usually in two divided doses Take pulse for one full minute prior to each dose Therapeutic vs. Toxicity Therapeutic range – 0.8 to 2.0 ng/ml Toxicity **EKG changes – arrhythmia Slow pulse- bradycardia Vomiting – very rare in infants Nursing Care How would the nurse recognize digitalis toxicity in an infant or child? Bradycardia, decreased appetite, N/V, diarrhea, dyspnea What are the pulse rate criteria in administration of digitalis? <90 bpm infant <70 bpm child Digitalis Why are we so concerned with the potassium levels when the child is on digitalis therapy? Can increase risk of digitoxin toxicity p. 1083 Nursing implications with Other Medications Diuretics – furosemide (Lasix) ACE inhibitors – Captopril, Enalopril Action – enhance renal secretion of sodium and water decreasing preload and pulmonary congestion Monitor vital signs Intake and output Electrolytes Action – promotes vasculature relaxation / vasodilation; increases renal blood flow thereby, decreases release of aldosterone/angiotensin – decreasing preload. It also reduces peripheral vascular resistance, reducing afterload. Monitor vital signs – check for signs of hypotension Beta Blockers – Inderal Slow the heart rate - assess vital signs Treatment of Heart Failure What is the type of Diet most commonly ordered? Nursing care: Measure intake and output – weighing diapers, weigh daily Observe for changes in peripheral edema and circulation If ascites present – take serial abdominal measurements to monitor changes. Skin care Turning schedule Promote rest Provide Oxygen Feeding the child with HF Feed the infant or child in a relaxed environment; frequent, small feedings may be less tiring Hold infant in upright position; may provide less stomach compression and improve respiratory effort If child unable to consume appropriate amount during 30-minute feeding q 3 h, consider nasogastric feeding Monitor for increased tachypnea, diaphoresis, or feeding intolerance (vomiting) Concentrating formula to 30 kcal/oz may increase caloric intake without increasing infant’s work Educating Parents Signs and symptoms of heart failure Increased cyanosis Dehydration Infection Dysrhythmias Decreased nutritional intake Copyright © 2018 Elsevier Inc. All rights reserved. Review An infant with heart failure is receiving digoxin. What should the nurse assess prior to administrating the medication? A. Pulse oximetry B. Apical pulse rate C. Breath Sounds D. Liver function tests Cardiac Catheterization Invasive procedure that can be 1-Diagnostic • • Measure oxygen saturations and pressure in the cardiac chambers and great arteries Evaluate cardiac output 2-Therapeutic 3-Interventional Cardiac Catheterization This process involves passing a catheter through the femoral vein or artery into the heart. Performed to evaluate heart valves, heart function and blood supply, or heart abnormalities in newborns. Cardiac Catheterization Pre-care: History and Physical Lab work – EKG, ECHO cardiogram, CBC NPO Vital signs Preprocedural teaching Best Nursing Action Situation: During post-procedure assessment every 5-15 minutes, the nurse notes bleeding at the insertion site. What should the nurse do first? Apply pressure on the insertion site for 10-15 minutes What additional interventions should be implemented post-procedure? Post Cardiac Catheterization Care Post Cardiac Catheterization Care Childs leg stabilized keeping it extended Cardiac Anomalies - Treatment The Child Undergoing Cardiac Surgery Preoperative preparation Postoperative management Monitoring cardiac output Supporting respiratory function Monitoring fluid and electrolyte balance Promoting comfort Healing and recovery Copyright © 2018 Elsevier Inc. All rights reserved. Review A 7-year-old child is recovering from a severe sore throat. The caregiver states that the child now has chest pain, in addition – the child is noted to have swollen joints, nodules on the fingers, and a rash on the chest. The likely cause of this is_______________________. Thank you! Resources: McKinney (2018). Ch. 46, p. 1077-1104; 11081112. Please contact Dr. Vicki Johnson at vicki.johnson@austincc.edu with any questions regarding this information.