Pediatric Cardiology Key Concepts: Chapter 40
advertisement
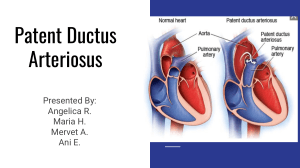
Chapter 40 ■■■ Key Concepts • • • • • • • • • • • • • • At birth, when the umbilical cord is cut and the neonate’s first breath occurs, the ductus venosus closes with the foramen ovale and the ductus arteriosus closes shortly thereafter. Pulmonary vascular resistance decreases and systemic vascular resistance increases. The infant’s heart rate averages 120 to 130 beatsmin and decreases throughout childhood, reaching the adult rate in adolescence. Conversely, the infant and child’s BP is significantly lower than the adult’s, increasing as the child ages. Check the infant’s apical pulse prior to digoxin administration and hold the dose if the heart rate is less than 90. Poor weight gain, failure to thrive, and increased fatigability commonly occur with congestive heart failure. Clubbing of the fingernails occurs as a result of chronic hypoxia in the child with severe CHD. Children with cardiac conditions resulting in cyanosis often have baseline oxygen saturations that are relatively low due to the mixing of oxygenated blood with deoxygenated blood. Document the presence of a murmur by grading its intensity (I--IV), describing where it occurs within the cardiac cycle, and noting the location where the murmur is best heard. CHD should be suspected in the cyanotic newborn who does not improve with oxygen administration. Cardiac catheterization post-procedure care focuses on evaluation of the child’s vital signs and condition of the pressure dressing, as well as assessment of the distal pulses bilaterally for presence and quality. Congenital heart disorders resulting in decreased pulmonary blood flow (tetralogy of Fallot, tricuspid atresia) lead to cyanosis. Disorders with increased pulmonary blood flow (patent ductus arteriosus, ASD, and VSD) may result in pulmonary edema if the defect is severe. A decrease in the lower extremity pulses or BP as compared with the upper extremities may be indicative of coarctation of the aorta. It is important to remain calm when an infant or child demonstrates a hypercyanotic spell. Place the child in a knee-chest position, administer oxygen andor morphine or propranolol, and supply intravenous fluids. Children with certain congenital heart defects andor heart failure require additional calories in order to display adequate growth. • • • • • Children with hypertrophic cardiomyopathy, certain congenital heart defects, valve dysfunction, or prosthetic valves require prophylaxis for bacterial (infective) endocarditis when undergoing procedures or invasive dental work. Hypertension in the child or adolescent often leads to long-term health consequences such as cardiovascular disease and left ventricular hypertrophy. Kawasaki disease may result in severe cardiac sequelae, so these children need ongoing cardiac follow-up to screen for development of problems. It is important to screen for hyperlipidemia in high-risk children. Abrupt cessation of chest tube output, accompanied by an increase in the heart rate and increased filling pressure, may indicate cardiac tamponade.