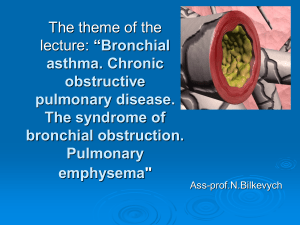
Asthma Overview: Causes, Symptoms, and Treatment
advertisement

ASTHMA What is it? Asthma is a chronic inflammatory disorder of the bronchial mucosa, which leads to bronchial hyperresponsiveness, constriction of the airways, and reversible airflow obstruction. Causes: Pathophysiology - Episodic attack of bronchospasm, bronchial inflammation, mucosal edema, and increased mucous production. Early asthmatic response (first 30 mins) Vasodilation Increase capillary permeability Mucosal edema bronchospasm Tenacious mucous secretion Exposure to allergens, viral infection, pollution, smoking, or extreme temperatures. Inflammatory Mediators: Mast cells, during inflammation, release histamine, prostaglandins, leukotrienes, and bradykinins > recruitment of neutrophils, lymphocytes, basophils, and eosinophils. Late asthmatic response (4-8 hrs) Symptoms: - Usually asymptomatic between attacks - Expiratory wheeze on auscultation, rapid onset, difficult expiration, nonproductive cough, dyspnea., tachypnea, tachycardia - Pulsus paradoxus (BP decreases with inspiration but increases with expiration) - Status asthmaticus (does not respond to bronchodilators and corticosteroids > Life-threatening) Inflammatory response (recruitment of WBCs) Airway scarring Increased bronchial hyperresponsiveness Impaired mucociliary function Decreased Treg cells Treatments: - Beta2-agonist bronchodilators and oxygen - Leukotriene antagonists - Immunotherapy (monoclonal antibodies to IgE) Complications: - Status asthmaticus - Acute respiratory failure Nursing Considerations: - Educate patients regarding allergens, irritants, and peak flow meters Environment should be free of allergen-laden Monitor for exacerbation, respiratory failure, and status asthmaticus Monitor breathing pattern, auscultate lungs every 4 hrs, and monitor pulse ox. Daily monitoring with peak flowmeter is high recommended.