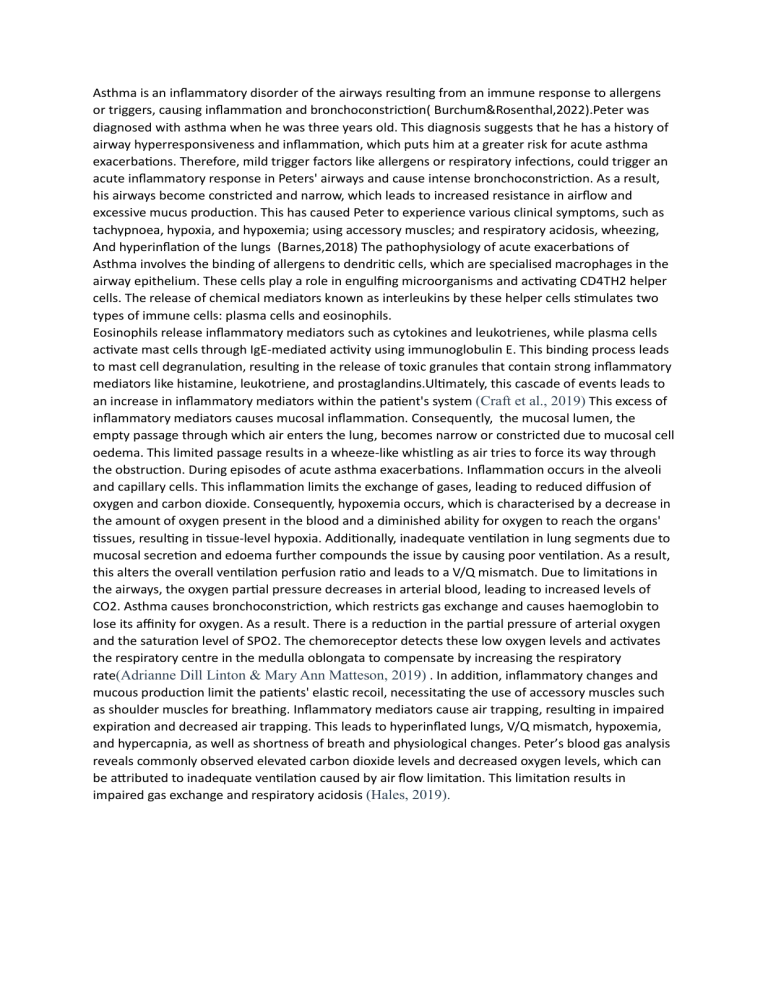
Asthma is an inflammatory disorder of the airways resulting from an immune response to allergens or triggers, causing inflammation and bronchoconstriction( Burchum&Rosenthal,2022).Peter was diagnosed with asthma when he was three years old. This diagnosis suggests that he has a history of airway hyperresponsiveness and inflammation, which puts him at a greater risk for acute asthma exacerbations. Therefore, mild trigger factors like allergens or respiratory infections, could trigger an acute inflammatory response in Peters' airways and cause intense bronchoconstriction. As a result, his airways become constricted and narrow, which leads to increased resistance in airflow and excessive mucus production. This has caused Peter to experience various clinical symptoms, such as tachypnoea, hypoxia, and hypoxemia; using accessory muscles; and respiratory acidosis, wheezing, And hyperinflation of the lungs (Barnes,2018) The pathophysiology of acute exacerbations of Asthma involves the binding of allergens to dendritic cells, which are specialised macrophages in the airway epithelium. These cells play a role in engulfing microorganisms and activating CD4TH2 helper cells. The release of chemical mediators known as interleukins by these helper cells stimulates two types of immune cells: plasma cells and eosinophils. Eosinophils release inflammatory mediators such as cytokines and leukotrienes, while plasma cells activate mast cells through IgE-mediated activity using immunoglobulin E. This binding process leads to mast cell degranulation, resulting in the release of toxic granules that contain strong inflammatory mediators like histamine, leukotriene, and prostaglandins.Ultimately, this cascade of events leads to an increase in inflammatory mediators within the patient's system (Craft et al., 2019) This excess of inflammatory mediators causes mucosal inflammation. Consequently, the mucosal lumen, the empty passage through which air enters the lung, becomes narrow or constricted due to mucosal cell oedema. This limited passage results in a wheeze-like whistling as air tries to force its way through the obstruction. During episodes of acute asthma exacerbations. Inflammation occurs in the alveoli and capillary cells. This inflammation limits the exchange of gases, leading to reduced diffusion of oxygen and carbon dioxide. Consequently, hypoxemia occurs, which is characterised by a decrease in the amount of oxygen present in the blood and a diminished ability for oxygen to reach the organs' tissues, resulting in tissue-level hypoxia. Additionally, inadequate ventilation in lung segments due to mucosal secretion and edoema further compounds the issue by causing poor ventilation. As a result, this alters the overall ventilation perfusion ratio and leads to a V/Q mismatch. Due to limitations in the airways, the oxygen partial pressure decreases in arterial blood, leading to increased levels of CO2. Asthma causes bronchoconstriction, which restricts gas exchange and causes haemoglobin to lose its affinity for oxygen. As a result. There is a reduction in the partial pressure of arterial oxygen and the saturation level of SPO2. The chemoreceptor detects these low oxygen levels and activates the respiratory centre in the medulla oblongata to compensate by increasing the respiratory rate(Adrianne Dill Linton & Mary Ann Matteson, 2019) . In addition, inflammatory changes and mucous production limit the patients' elastic recoil, necessitating the use of accessory muscles such as shoulder muscles for breathing. Inflammatory mediators cause air trapping, resulting in impaired expiration and decreased air trapping. This leads to hyperinflated lungs, V/Q mismatch, hypoxemia, and hypercapnia, as well as shortness of breath and physiological changes. Peter’s blood gas analysis reveals commonly observed elevated carbon dioxide levels and decreased oxygen levels, which can be attributed to inadequate ventilation caused by air flow limitation. This limitation results in impaired gas exchange and respiratory acidosis (Hales, 2019).