Asthma - Stony Brook University School of Medicine
advertisement
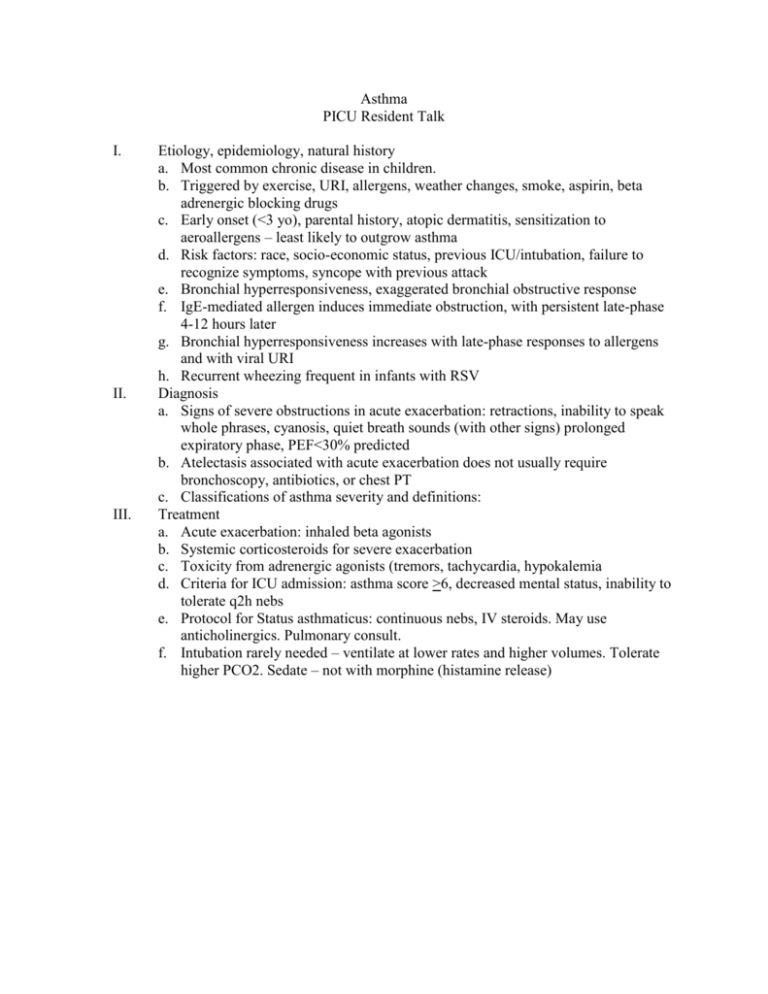
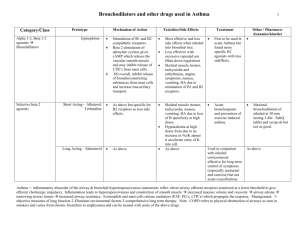
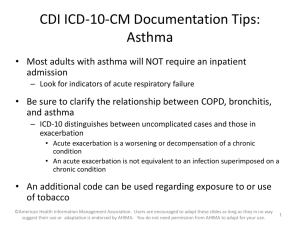
Asthma PICU Resident Talk I. II. III. Etiology, epidemiology, natural history a. Most common chronic disease in children. b. Triggered by exercise, URI, allergens, weather changes, smoke, aspirin, beta adrenergic blocking drugs c. Early onset (<3 yo), parental history, atopic dermatitis, sensitization to aeroallergens – least likely to outgrow asthma d. Risk factors: race, socio-economic status, previous ICU/intubation, failure to recognize symptoms, syncope with previous attack e. Bronchial hyperresponsiveness, exaggerated bronchial obstructive response f. IgE-mediated allergen induces immediate obstruction, with persistent late-phase 4-12 hours later g. Bronchial hyperresponsiveness increases with late-phase responses to allergens and with viral URI h. Recurrent wheezing frequent in infants with RSV Diagnosis a. Signs of severe obstructions in acute exacerbation: retractions, inability to speak whole phrases, cyanosis, quiet breath sounds (with other signs) prolonged expiratory phase, PEF<30% predicted b. Atelectasis associated with acute exacerbation does not usually require bronchoscopy, antibiotics, or chest PT c. Classifications of asthma severity and definitions: Treatment a. Acute exacerbation: inhaled beta agonists b. Systemic corticosteroids for severe exacerbation c. Toxicity from adrenergic agonists (tremors, tachycardia, hypokalemia d. Criteria for ICU admission: asthma score >6, decreased mental status, inability to tolerate q2h nebs e. Protocol for Status asthmaticus: continuous nebs, IV steroids. May use anticholinergics. Pulmonary consult. f. Intubation rarely needed – ventilate at lower rates and higher volumes. Tolerate higher PCO2. Sedate – not with morphine (histamine release)