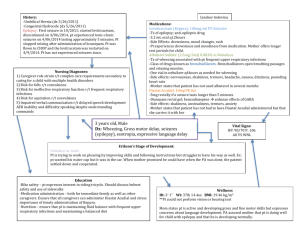
Care plan example
advertisement

ASSESSMENT Relevant Data Age 7 Male Weight 26.8 kg PMHX- asthma Allergies – eggs, milk, dairy and nuts Presented in ED with SOB, cough, fever, wheezing. X3 days. Assessment on Day 1 Vitals – 0800h T 36.5 AX HR 154 Resps 23 BP 95/58 SpO2 96% 2L Oxygen NP Pain – 0/10 Alert and oriented X 3 Cap refill less than 2 seconds. Patient using abdominal muscles to assist with respirations, intercostal indrawing. No nasal flaring or tracheal tug noted. Pt. able to speak full sentences between breaths. Occasional dry, nonproductive cough Air entry very diminished ANALYSIS Nursing Diagnosis Ineffective breathing pattern r/t inflamed bronchial passages, and respiratory muscle fatigue AEB shortness of breath, coughing and accessory muscle use. PLAN Expected Outcomes Goal: The patient will demonstrate breathing pattern within normal limits and no longer require supplemental oxygen. Expected Outcomes: The patient will: 1. Report ability to breathe comfortably by end of shift 2. Patient will require less frequent ventolin treatments by 24 hours postadmission PLAN IMPLEMENTATION EVALUATION Of Expected Outcomes Interventions Rationale Effectiveness of Interventions 1. Monitor respiratory rate, depth, and ease of respirations q4h and prn Monitoring trends in respiratory status will demonstrate improvements or worsening respiratory status. (Wilson & Smith, 2004 as cited in Ackley & Ladwig, 2010) Respiratory rate went from mildly tachypneic at 23 breaths per minute to 18 breaths per minute which is in the normal range for this client’s age Goal partially met. 2. Note abdominal breathing, use of accessory muscles, nasal flaring, retractions, irritability, confusion or lethargy q4h These symptoms signal increasing respiratory difficulty and increasing hypoxia (Jones & Smith, 2008 as cited in Ackley & Ladwig, 2010) At the beginning of the shift, the client was using abdominal muscles to breathe and had intercostal indrawing. This subsided over the course of the shift. 2. Air entry improved (less tight, less wheezy) during shift therefore less ventolin needed 3. Monitor Sp02 continuously and blood gases as ordered. Oxygen saturation less than 90% (normal 95100 %) or a partial pressure of oxygen of less than 80% (normal 80-100%) indicates significant oxygenation problems (Berry and Penard, 2002; Grape, 2002). Over the course of the shift, the client was able to be weaned from 2L/min of oxygen via nasal prongs to 1L/min and maintain his saturations greater than 94% Wheezing had decreased during the shift, 1. Patient did report feeling “better” by end of shift 3. accessory and abdominal muscle use not evident by end of shift 4. respiratory rate normalized (“tight”) throughout all lung fields with inspiratory and expiratory wheezing bilaterally to bases. Wheezing coarser to right lower lobe. Abdomen soft, nondistended, bowel sounds present x 4 quadrants. Vitals – 1200h T 36.6 HR 137 Resps 18 BP 105/57 Sp02 97% 1L Oxygen NP Pain 0/10 Pt. no longer using abdominal muscles to breath. No intercostal indrawing, no tracheal tug or nasal flaring. Pt able to speak in full sentences between breaths. Air entry improved (“less tight”) with mild wheezing on inspiration and expiration bilaterally to bases. Wheezing remains increased to right side. Air entry much improved and less wheezy post-ventolin treatments Patient reports feeling better No other changes from previous assessment. 3. Respiratory rate will return to normal limits for age within 24 hours of admission 4. Air entry will be clear and equal bilaterally to all lobes by day 2 of admission 5. No nasal flaring, tracheal tug, or accessory muscle use noted by day 2 of admission 6. SpO2 will be greater than 94% on room air by day 2 of admission 4. Auscultate breath sounds every 4 hours and when required, noting decreased or absent sounds, crackles, or wheezes. 5. Administer oxygen as required. 6. Position patient in an upright or semiFowler’s position when awake 7. Administer medications such as bronchodilators or inhaled steroids as ordered These abnormal lung sounds can indicate a respiratory pathology associated with an altered breathing pattern. (Ackley & Ladwig, 2004) Oxygen therapy helps decrease dyspnea through reduction in the central drive mediated via peripheral chemoreceptors in the carotid body (Meek, 1999). An upright position facilitates lung expansion. (Ackley & Ladwig, 2004) Appropriate and timely use medications can decrease the risk of exacerbating ineffective breathing (Ackley & Ladwig, 2004) especially after each ventolin treatment. Air entry also improved becoming less tight over the course of the shift Able to wean oxygen from 2L/min to 1L/min during shift Head of bed remained elevated to high-Fowler’s position during day Ventolin was ordered q2h on admission. During course of shift went to q4h and then ordered on a prn basis. from 23/min to 18/min 5. patient remained on oxygen at end of shift 6. frequency of ventolin treatments changed from q2h to q4h to prn