File - Jessica Lynn Anderson
advertisement

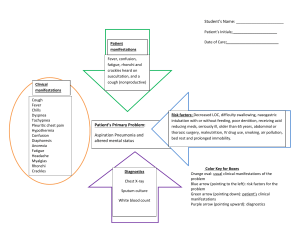
Student: Jessica Anderson Azusa Pacific University GNRS 575 MATERNAL, NEWBORN, WOMEN’S HEALTH CARE MAP Admission Primary Nurse: Date: Letty 9/17/13 Date of Care: 9/19/13 HISTORICAL INFORMATION Patient’s Initials: D.L. Age: 29 years BP range(on prentatal records) ALLERGIES: Room Number: 330 Sex: Female BP’s were never under 150/99 No Known Allergies Admitting Diagnosis: Unit: Ht 4’9” Postpartum Wt BMI Lbs 161lbs. kg 73.029 kg 33.66 kg/m^2 Pregnant (37 weeks and 3 days), Vaginal Bleeding History Of Present Illness: Chronological account of patient’s current illness with pertinent +’s and –“s included and correct medical terminology used. D.L. came into the clinic for an appointment and had minimal bleeding. After she left the clinic and went home she noticed an increase in the amount of bleeding. The patient noted that she had filled two pads within an hour. An hour later she filled three more pads within an hour. She decided to come into the hospital and was admitted. The patient had pregnancy induced hypertension with a history of her BP’s never being lower than 150/99. When admitted on 9/17/13 the patient was 37 weeks and 3 days. There is good fetal movement. The patient’s water was broken at 0239 on 9/18/13. The patient was only 3cm dilated and 60% effaced. Due to the heavy amount of bleeding, the patient was said to have an abruption of the placenta and that the patient needed a C-section. Past Medical History: Major illness, surgeries, traumas, known allergies. The patient had a thyroidectomy in 2008. D.L. has developed gestational diabetes during this pregnancy, which is her first pregnancy. Social/Family History: Family medical and mental health history, composition of family, living conditions, safety issues, habits, etc. D.L. had her family at the bedside. Her husband was present and very attentive and supportive. Her mother and other relatives were present and at her bedside. The patient is a scheduling counselor for a firm and her husband works in accounting. They have a home and have already started preparing for the baby. The patient’s father has a history of diabetes. The patient does not smoke or do drugs. She drinks occasionally when she is not pregnant. OB History: Past pregnancies, obstetrical complications in previous or current pregnancies, etc. G1/T1/P0/A0/L0 This is the patient’s first pregnancy. She has pregnancy-induced hypertension with this pregnancy. PATHOPHYSIOLOGY/PHYSIOLOGY Include a brief description of your patient’s disease process. This should be told in a narrative “story” form. If your patient has had an essentially “normal” process you must highlight the normal physiology that occurs in this type of patient (i.e. normal postpartum physiology for a postpartum patient). For a patient who has a pathophysiologic process occurring, include the pathophysiological changes that occur in the current diagnosis(es) and explain how the concurrent diagnoses affect the priority diagnoses. For all patients: (1) Explain usual/expected treatment (2) Highlight what diagnostic tests, treatments, or teaching are currently being done for your patient. Pregnancy-induced hypertension (PIH) is high blood pressure that occurs after the first half of the pregnancy (or 20th week) for the first time and when the blood pressure returns to normal within 12 weeks of delivery. High blood pressure is having a blood pressure 140/90 or over for an extended period of time. It is pregnancy-induced hypertension and not preeclampsia when there are no signs of proteinuria. This patient was a first time mom and sometimes first time moms can be at a higher risk. PIH is a concern because this means that there is an increased resistance in the blood vessels and this can cause a hindrance in the blood flow to important organs, one of them being the placenta. Another concern with PIH is that it can cause placental abruption, in which the placenta tears away from the uterus. This causes hemorrhaging and major complications for the baby because the baby relies on the placenta for survival. This patient was able to have a C-section when her placenta abrupted because the baby was viable at 37 weeks and 4 days (Davidson, London, & Ladewig, 2012). Expected tests for a woman with pregnancy-induced hypertension (PIH) includes regular blood pressure monitoring, urine testing, liver and kidney tests and frequent weight measurements. Treatment for PIH can include bedrest, hospitalization, magnesium sulfate, fetal monitoring, continued laboratory testing of urine and blood, delivery of the baby when possible (Davidson, London, & Ladewig, 2012). This patient had frequent blood pressure readings and the BP’s never went under 150/99 during her pregnancy. While she was in the hospital she was receiving magnesium sulfate through an IV to help with her hypertension and prevent any seizures that might occur. She was kept on the IV for 24 hours after the delivery. The baby was delivered via cesarean when the placenta abrupted. DIAGNOSTICS/LABORATORY/TREATMENT DATA List all labs Prenatal: Blood type Rh factor HIV 1+2 HbsAg (HepB) GBS Rubella IGG Current: WBC (103cells/mm3) Normal value range for your patient’s age (9/4/13) ABO - /+ Non-reactive Non-reactive Negative Immune Most Recent (Date) Previous Recent (Date) O + Non-reactive Non-reactive Negative Immune (9/17/13) Before Birth 500012,000/microliter 130,000-400,000 9,000/microliter Interpretation of abnormal labs (tie into pathophysiology of illness) Not available Not available Platelets 148,000 Not available (mm3) Hemoglobin 12-16 g/dL 12.1 g/dL Not available (g/dL) Hematocrit 38%-47% 38.6% Not available (%) *Values for normal found in the table (Davidson, London, & Ladewig, 2012, p. 327). Imaging: Ultrasound at 20 weeks Results: Showed girl with an enlarged clitoris All Ordered Medical Treatments and Nursing Activities): C-section Results and Rationale: Magnesium Sulfate Monitoring Blood pressure post C-section The patient’s placenta had abrupted and the patient was only 3cm dilated and 60% effaced. The C-section went smoothly and delivered a healthy baby boy. In cases of moderate to severe placental separation, a cesarean birth is done (Davidson, London, & Ladewig, 2012, p. 677). The patient was placed on magnesium sulfate to prevent seizures and help with the patient’s blood pressure. A woman who has received magnesium sulfate antepartally will continue to receive the infusion for about 24 hours postpartum (Davidson, London, & Ladewig, 2012, p. 469). The patient’s blood pressure is 127/75. If preeclampsia does not develop and blood pressure returns to normal by 12 weeks postpartum, the diagnosis of gestational hypertension may be assigned (Davidson, London, & Ladewig, 2012). IV Solutions/Additives: Maintenance Rate: 50mL/hr Magnesium Sulfate 50mL/hr Lactated Ringer Nursing Responsibilities: Monitor the IV lines and the site. Monitor the patient for any seizures. Monitor the IV lines and the IV site. NURSING PROCESS APPLICATION Note: You may NOT use “PAIN” as a diagnosis for your labor or PP patients more than once in the semester! Problem/ Nursing Dx (Physical) 1. 2. 3. 4. Impaired skin integrity related to a cut in the skin as evidenced by an incision in the patient’s abdomen and staples holding the incision together. Goal: The patient’s incision will not become infected or show dishescences during her stay at the hospital. Interventions: Rationales: Assess the general condition of the skin. 1. “Assessment provides a basis for interventions. Healthy skin varies among individuals but should have good turgor, feel warm and dry to the touch, be free of impairment, and have quick capillary refill” (Gulanick & Myers, 2011, p.179). Monitor site of skin impairment at least once a 2. “Systematic inspection can identify impending day for color changes, redness, swelling, problems early” (Ackley & Ladwig, 2011, p. warmth, pain or other signs of infection. 770). Do not position the client on site of skin 3. “Continue to turn/reposition the individual impairment and turn and position the client regardless of the support surface used (Ackley every 2 hours to prevent further skin damage. & Ladwig, 2011, p. 770). Encourage adequate nutrition and hydration. 4. “Optimizing nutritional intake, including calories, fatty acids, protein, and vitamins, is needed to promote wound healing” (Ackley & Ladwig, 2011, p. 770) Evaluation of Interventions The interventions were successful in meeting the goal. The patient’s (If not met or partially met wound did not become infected or show dishescense. Proper explain why): assessment, positioning and nutrition were helpful in preventing infection. Problem/Nursing Diagnosis (Psychosocial) 1. 2. 3. Risk for anticipatory grieving related to ambiguous genitalia as evidenced by the mother stating “we thought the baby was going to be a girl, but it ended up being a boy” and “we already bought all the stuff for a girl”. Goal: The patient will verbalize that she has come to terms with the gender of her baby by the end of the shift. Interventions: Rationales: Identify behaviors that are suggestive of the 1. “Mourning is associated with the grieving process. behavioral manifestations of grief. Grief is an individual and exquisitely personal experience” (Gulanick & Myers, 2011, p. 87). Identify the availability of support systems for the 2. “Social support has been shown to help patient. bereaved individuals” (Ackley & Ladwig, 2011, p. 412). Concentrate on improving communication and 3. “Communication within the family has provide an environment for families to connect with been shown to be a major predictor of one another. grief because it is an important 4. component in the ability to share grief and express feelings about the loss in a supportive environment” (Ackley & Ladwig, 2011, p. 412). Discuss spirituality with the patient and her spouse. 4. “Researchers have found a striking correlation between good spiritual health and good physical health. Spiritual well-being may improve the quality of life in clients” (Ackley & Ladwig, 2011, p. 412). Evaluation of Interventions The interventions were successful in helping the patient come to (If not met or partially met terms with the gender of her baby. The patient stated “I guess this explain why): just means we need to buy all new things” and “he is such a cute little boy”. The patient and her husband were very open when talking about their new little boy and stated how they have people from their church that are praying for them and their new baby. Problem/Nursing Diagnosis (Knowledge Deficit) 1. 2. 3. 4. Knowledge deficit related to breastfeeding as evidenced by the baby not latching onto her breast and the patient saying “he does not latch well onto my right breast”. Goal: The patient will demonstrate correct breastfeeding techniques for a good latch by the end of the shift. Interventions: Rationales: Provide time for the patient to express expectations 1. “Lactation consultants and nurses play a and concerns and give emotional support. key role in the establishment of breastfeeding” (Ackley & Ladwig, 2011, p. 187) Teach the patient to have a quiet atmosphere 2. “A calm quiet environment assists the without interruption. Promote comfort and patient with concentrating more relaxation to reduce pain and anxiety. completely” (Gulanick & Myers, 2011, p. 117). “ Discomfort and increased tension are factors associated with reduced letdown reflex and premature discontinuance of brestfeeding” (Ackley & Ladwig, 2011, p. 187). Teach the patient to monitor infant behavioral cues 3. “Infant behaviors contribute to oxytocin and responses to breastfeeding. release and let-down, contribute to effective feeding, indicate effective breastfeeding, manifest satiety, and indicate adequacy of the feeding while contributing to positive maternal-infant attachment” (Ackley & Ladwig, 2011, p. 187). Provide the necessary instructions and resources to 4. “Evidenced-based guidelines and find a technique that works for this mother and her systematic reviews support the use of baby boy. professionals with special skills in breastfedding” (Ackley & Ladwig, 2011, p. 187). Evaluation of Interventions The interventions were successful in helping the patient learn and (If not met or partially met demonstrate a good latch for her baby. She was assisted in trying explain why): new positions to feed her baby and the football hold was found to be the most effective way for her to breastfeed on both her breasts. MEDICATIONS ALLERGIES: No Known Allergies Medication Strength/ Frequency Mechanism of Action Why is the patient on the medication Side effects Nursing responsibilities Colace 100mg BID Stool softener Diarrhea -Observe for diarrhea Motrin 600 mg q6h Relief from mild to moderate pain The patient just had surgery and had not had a bowel movement. The patient is taking it for pain post-cesarean. -Monitor patients level of pain -Monitor the patient for reaction Magnesium Sulfate 50mL/hr Blocks neuromuscular transmission To help prevent seizures Headache, dizziness, insomnia, nausea, constipation, agranulocytosis, pancytopenia, aplastic anemia Weakness, dizziness, magnesium intoxication, depressed reflexes Labetalol 200mcg Every morning Lowers blood pressure Patient had pregnancy induced hypertension Bronchospasm, dyspnea, nausea, vomiting -Monitor the patient for any of the side effects -Assist the patient with any ambulation -Monitor the patient’s blood pressure and take a new blood pressure before administering. Student reflection: This week was a bit of an adjustment period as it was not as fast paced as Labor and Delivery, but also because I did not know what my role was in caring for postpartum women and their babies. It took me a couple hours in the morning of following around my nurse and interacting with the patients to finally feel more confident in my abilities as a postpartum nurse. Having no experience of my own in being a mother, I felt a few steps behind the others in the clinical group, but I found my love for talking with people and years of experience with kids and babies helped out greatly when connecting with the patients. The moment I felt most proud was at the end of the day when I was helping to clean up a baby and then swaddle him. The new dad stepped up behind me and asked if he could watch how I swaddled the baby boy. Even though it was just swaddling a baby, I felt like I did have something to contribute and was able to help out a first time dad who just wanted to learn how to wrap his new baby. I learned that there is so much I have to contribute and to share with these new parents. Watching and listening to my nurse instruct my patient on how to breastfeed more effectively, helped me to learn how I can help another mom in the future. Next week I hope to continue meeting the patient’s needs in anyway I can, whether it be through time spent with them talking or teaching them. Spiritual reflection: This week during clinical I felt like I had a slower start to making a spiritual connection with my patient. Due to the fact that I was working with my nurse’s three patients and also helping other patients, I felt that I did not spend as much time in my patient’s room as I usually like. During the time I was able to spend with my patient, I talked with her and her husband about their support system and the big transition this was going to be for them as first time parents. We talked about the church they were involved with and how many of the people were praying for them and their new baby. They seemed to have a very firm foundation in Christ and it was neat to see that even during this transition period and the surprise that they had when they discovered their baby was a boy, they both felt very supported by their church body. One thing that I missed doing with this couple was taking the time to pray with them before I left for the day. I usually make time for it before I leave for the day, but I failed to do it with this couple. Often times I forget the power prayer can have. Recently in bible study, my bible study teacher said, “Many times we say we are going to pray for people, but then we forget or we do not follow through. I think the reason so many of us brush prayer aside is because we forget the power it has to change our life and those around us” (Personal Communication, 2013). I like this quote from O’Brien that says, “Prayer, whether formal or informal, may be central to healing the sick. Healing prayer has been described as bringing oneself and a situation of disease before God, with at least one other person to listen, discern, speak and respond, so that healing in relation to or with God can take place” (O’Brien, 2011, p. 153). My priority for this coming week is to spend time in prayer with my patient. References Ackley, B. J. & Ladwig, G. B. (2011). Nursing diagnosis handbook: An evidence-based guide to planning care (9th ed.). St. Louis, MO: Mosby Elsevier. Davidson, M., London, M., & Ladewig, P. (2012). Old's maternal-newborn nursing & women's health across the lifespan. Upper Saddle River, NJ: Pearson. Gulanick, M. & Myers, J. (2011). Nursing care plans: Diagnoses, interventions, and outcomes. Philadelphia, PA: Elsevier. Karch, Amy M. (2013). Lippincott’s nursing drug guide. Rochester, New York: Lippincott Williams and Wilkins. Lehne, R.A. (2013). Pharmacology for nursing care (8th ed.). St. Louis, MO : Saunders Elsevier. McCance, K.L, Huether, S.E., Brashers, V.L. & Rote, N.S. (2010). Pathophysiology: The biologic basis for disease in adults and children (6th ed.). Maryland Heights, MO: Mosby Elsevier. O’Brien, M. E. (2011). Spirituality in nursing: Standing on holy ground, (4th ed.). Boston, MA: Jones & Bartlett. Potter, P.A. & Perry, A.G. (2012). Fundamentals of nursing (8th ed.). St Louis, MO: Mosby Elsevier. Azusa Pacific University GNRS 575 Grading Criteria Sections Criteria Historical Information Possible Points 20% Demographics and specified growth and BP parameters Diagnosis (es) All info present 2 Patient’s current priority diagnosis (es) 2 History of Present Illness Chronological account of patient’s current illness with pertinent positive’s and negative‘s included and correct medical terminology used. Major illness, surgeries, traumas, known allergies, and birth history (if appropriate) included. Family medical and mental health Hx, composition of family, living conditions, safety issues, smoking in home History complete and correctly documented. 4 Past Medical History Social/Family History Obstetric History Pathophysiology Laboratory and Diagnostic Tests Medical Treatments Problems or Nursing Diagnoses with 1 goal for each followed by interventions and evaluation criteria Pathophysiology 25% (1) Pathophysiological changes that occur in the current diagnosis (es), (2) Explain how the concurrent diagnoses affect the priority diagnoses. (3) Explain anticipated treatment. (4) Highlight what diagnostic tests, treatments, or teachings are currently being done for your patient. Laboratory Values/Medical Treatments15% Most recent and previous most recent lab test results with all abnormal results explained. Medical treatments listed and all rationales included. Goals and Rationale for Treatment, Medications, & APA 40% Two priority-nursing diagnoses listed with goals and related interventions: there must be 1 physiologic and 1 psycho-social, Include rationale for all interventions. Must be individualized to the patient’s needs with evaluation of the effectiveness of the interventions included. Medications Drug Class/MOA, onset and duration, side effects, dosage/ routes, and nursing responsibilities included. APA Incorporates the entire writing process using resources. APA style followed consistently, less than two APA errors are seen with page format. Paper is written in a scholarly style. All sources are correctly written in the in-text citation and on the References page. Total Points 4 4 4 25 10 5 10 (diagnosis) 10 (goals) 10 (int/ rationale) 5 5 100 Points Earned