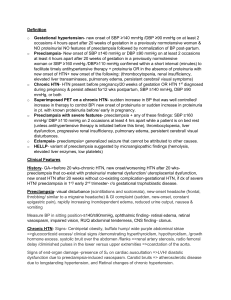
Pregnancy Induced HTN(Preeclampsia) Diagnosis: Urinalysis, Pap smearabnormal cervix, HbA1C, Proteinuria+,Znormal platelet Labs: CBC, urine specific gravity-1.005, O blood typing, glucose 72 H&H WBC, 1hr glucose test, HSV, Low Platelet, liver enzymes, negative ketone Patient Presentation A, P.W. 38year Old Female Gravida2Para0 admitted 4/8/21 presented to the L& D for Scheduled Induction. GA: 37 wk2, on full code, weight 233Ib, BMI at 36.61. She has sulfa antibiotics as allergies. Her PMH include GHTN, HSV, Low lying Placenta, anemia, abnormal pap smear, Past SurgicalTherapeutic abortion, umbilical hernia repair and wisdom tooth extraction. Health Assessment: Neuro: A&Ox4, visual impairment, headache, CNS irritability. Cardio: S1, S2, no murmurs, capillary refill 2+ HTN with elevated BP 163/92 after 20th week of pregnancy, Paulse 87, +2 dependent edema, and facial puffiness s, hands, and leg swelling.no chest tightness, noted fatigue no nausea and vomiting, fetal well-being, with normal FHR fetus is active. Respiratory: Chest symmetry, lungs sound clear bilaterally, RR16, O2 98% FHR manually or electronically checked.GI /GU: Epigastric pain subtle, urine oliguria and straw color, Proteinuria in urine and liver enzymes leading to causes organ damage and potential for seizure, Skin: weight gain, peripheral edema, edema of hands and feet, deep tendon reflexes 2+, ankle clonus subtle. reproductary: breast engorged with striae, perinium at 2cm. IV patent at 2o gauge # 1Nursing Diagnosis Risk for Maternal Injury r/t eclamptic seizure as evidenced by BP of 163/ 92 and diagnosis of preeclampsia on BP and p/c ratio before 36th wks. Intervention: Put Patient on bed rest and seizure precautions- by providing bed alarms and side rails. -seizure precautions-reduced stimulation-bed restdim light Raise head of bed, Monitor Level of consciousness, Monitor headache or irritation caused by cerebral ischemia. Monitor Patient BP to reduce to 120/70.Delivery of Fetus only cure for Patient condition. Outcome: Patient will be free of irritation, visual disturbances, or headache/changes in mental status during shift. Implementation of safety measures and prevent ion of injury during shift. Patient’s BP to normalize to 120/70 and test of Protein during shift. Evaluation: Patient was free from signs of irritation r/t cerebral ischemia and Patient did not experience visual disturbances during shift. Patient was alert and oriented for the shift, Patient was safe from injury during shift with BP at 120/70 mmHg to reduce incidence of stroke. Protein Test was negative on her urine for the shift. Pathophysiology: The progressive pregnancy induced hypertension promotes, vasoconstriction and vasospasms of blood vessels particularly epithelial cells of the arteries which constricts and contribute to hypoxia of maternal organ tissues -brain, kidney, liver heart. The reduced uterine blood flow reduces placental perfusion, hypoxia resulting in reduced gas exchange and impaired nutritional functioning of the placenta. Maternal syndrome results in maternal complication of HELLP syndrome affecting the blood and liver. Risk Factors: First Pregnancy, Maternal age, African decent, obesity at BMI, Family Hx of HTN, low socio-economic Background, underlying Disease, #2 Nursing Diagnosis: Altered Tissue Perfusion r/t interruption of blood flowprogressive vasospasm of spiral arteries evidenced by changes in fetal activities/heart rate secondary to preeclampsia based on proteinuria before 36 weeks. Intervention:1. evaluate fetal growth, monitor t fetal activity2. assess fetal response to BPP criteria3 check fetal FHR manually /electronically4. Give betamethasone IM 7 days before delivery for fetal lung development 5. assess maternal plasma volume Outcome: Patient demonstrate normal CNS reactivity on NST during shift, Patient is free of late decelerations during shift, Patient monitored for progressive full term during shift. Evaluation: Patient did not exhibit late decelerations during shift. Patient has no decrease in FHR on contraction as she progresses on labor during shift. Key: Red-Assessment Blue- medication Brown-Patho Tx-Green Medication: Antihypertensive to reduce BP, baby Aspirin- reduces the risk of heart attack due to blocked arteries and stroke. Fexofenadine HCL is an antihistamine, iron for energy, Vit C,65125mg, Valacyclovir (Valtrex)500mg to Tx HSV, Betamethasone given for Fetal lung development. Lactated Ringers 1,000ml bolus, infusion at 100mls/hr Stadol PRN for L&D. #3 Nursing Diagnosis: Risk for Preterm delivery r/t to best /only cure of preeclampsia. Intervention:1 NST baseline 140,2. Fetal Assessment place Patient on continuous FHR monitor.3. Administer Betamethasone for lung development .4 Assess fetal movement 4. Have mother do fetal kick.5 Introduction of Epidural by 5cm dilation as per client request to manage pain at labor. Outcome: Fetus will display moderate variability during shift. Fetal will not have late decelerations or abnormal heart rate during shift. Contractions progress in frequency and intensity before end of shift Evaluation: Fetus displayed moderate variability during shift, Fetal did not have late decelerations nor abnormal heart rate during shift. Fetal monitored for progressive growth & term delivery during shift. Treatment: 1. Bed rest.2. Neuro checks, Vitals q4Reduce salt intake.3Give antihypertensive medications4. Provide Magnesium therapy to prevent seizures and limit complications Have Calcium Gluconate at hand,.5. Induction for preterm delivery of baby by 37th weeks the major solution to preeclampsia. Cytotec, Oxytocin, LR, Methylerg onovine, Hem abate, Zofran, Cefazolin, and other scheduled medications for Labor and postpartum administration. Patient Education: Teach Patient understanding of disease process and appropriate treatment plan. Teach Patient about lifestyle/behavior changes as indicated. Teach importance of patient promptly reporting signs/symptoms of CNS involvement Reference NANDA International & Herdman, T. H. (2012). NANDA International Nursing diagnoses: Definitions and classification 2012-14. Wiley-Blackwell Ricci, S., Kyle, T., & Carman, S. (2009). Nursing Management During the Postpartum Period. In Maternity and pediatric nursing (4th ed.). Lippincott Williams & Wilkins Roberts, J. M., & Gammill, H. S. (2005). Preeclampsia. Hypertension, 46(6), 1243-1249. https://doi.org/10.1161/01.hyp.0000188408.49896.c5