Maternity Exam #2 Study Guide: Fetal Well-being & High-Risk Pregnancy
advertisement

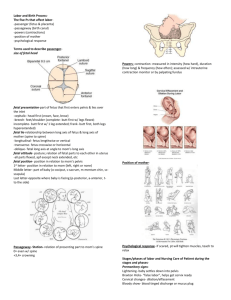
Study Guide for Maternity Exam #2 Summer 2022 Please use the textbook, PowerPoints, and the Maternity ATI to assist you with your studying. See if you can answer these questions after you review. Chapter 10: Assessments/ fetal Well Being and High-Risk Pregnancy What are the benefits of ultrasound? o An ultrasound test uses high-frequency sound waves, inaudible to the human ear, that are transmitted through the abdomen via a device called a transducer to look at the inside of the abdomen. With ultrasound, the echoes are recorded and transformed into video or photographic images of your baby. How is contraction stress test done? o A contraction stress test (CST) is performed near the end of pregnancy to determine how well the fetus will cope with the contractions of childbirth. The aim is to induce contractions and monitor the fetus to check for heart rate abnormalities Contractions may be brought on by an IV dose of Oxytocin or by stimulation of nipples o Enables identification of fetal risk for asphyxia o Fetal monitor is used o Fetal heart rate response to contractions is noted o Healthy fetus usually tolerates contractions What is amniocentesis as well as the nursing care? o Procedure used to obtain amniotic fluid o Allows for testing of amniotic fluid o These tests can provide information about genetic disorders o Done at 15-20 weeks o Rhogam for Rh- moms and Rh+ babies What is amniotic fluid analysis used for? o May be used in screening for the following Down syndrome (trisomy 21) Trisomy 18 and neural tube defects (NTDs) Can provide information about fetal lung maturity What are some risks associated with chorionic villus sampling? sampling of placental tissue Can be performed transabdominally or transcervically Performed between 10 and 12 weeks Performed for first trimester diagnostic studies Advantages o Allows for early detection of fetal disorders o Short waiting time for results Nursing Care: o Administer Rh immune globulin to ALL RH NEGATIVE WOMEN Disadvantages: Increased risk of injury to fetus Inability to detect neural tube defects Risk of leakage of amniotic fluid Risk of intrauterine infection Risk of Rh alloimmunization Miscarriage/preterm labor What is the difference between a reactive NST or non-reactive NST? o Reactive NST: Baseline HR 110-160bpm Two accelerations of FHR in 20min lasting 15s abrupt increase absence of deceleration o Non-reactive NST Chapter 11: Maternal endocrine, metabolic disorder and substance abuse. What is GDM and what is the confirmatory testing for GDM? o Gestational Diabetes Mellitus (GDM) Routine fasting done 24-28 weeks o Routine fasting done 24-48 weeks 1 hour glucose challenge test (GCT) 3-hour glucose tolerance test (GTT) Two abnormal results considered GDM GDM A1 diet controlled GDM A2 medication controlled (Glyburide or insulin) What are the care management of diabetes? o Antepartum Diet Exercise Self-monitoring of blood glucose Pharmacologic therapy Fetal surveillance o Intrapartum Blood glucose monitored hourly in labor Infusion of regular insulin Every 4 hr.: early; every 2 hrs.: active o Postpartum Will return to normal glucose levels after birth Likely to recur in future pregnancies What is the insulin requirement during the 1st trimester? o reduced, due to an increase in insulin production & glucose transfer to fetus o 2nd: need increases o 3rd: increase, level off a 36w What are the effects of diabetes on the fetus? o macrosomia - big baby (>8.8lbs) o neonatal hypoglycemia o IUFD o birth defects Define hyperemesis gravidarum. o Hyperemesis gravidarum is excessive, prolonged vomiting accompanied by the following: Weight loss Electrolyte imbalance Nutritional deficiencies Ketonuria What is the management of hyperemesis gravidarum? o Assessment: Assess severity Weight, V/S, presence of ketonuria Psychosocial assessment: role of anxiety o Management: Intravenous (IV) therapy for correction of fluid and electrolyte imbalances Medications Enteral or parenteral nutrition as a last resort Review maternal PKU. o Inborn error of metabolism caused by an autosomal recessive trait that creates a deficiency in the enzyme phenylalanine hydrolase, which impairs the body’s ability to metabolize foods with protein o If unrecognized, can cause cognitive impairment o Prompt diagnosis and therapy with a phenylalanine-restricted diet significantly decreases the incidence of cognitive impairment. o Women with PKU should be advised against breastfeeding because their milk contains a high concentration of phenylalanine. o Prevention Identification of women in reproductive years who have disorder Screening at the first prenatal visit Breastmilk tested for PKU o Infants born to women with this disorder are either homozygous or heterozygous for the trait. Infants tested for PKU and fed special formula if necessary Chapter 12: Hypertensive disorders and hemorrhagic disorders: Review the classification of hypertensive disorder. o Gestational HTN Onset of HTN without proteinuria or other system findings diagnostic for preeclampsia after week 20 of pregnancy Systolic BP >140, Diastolic BP >90 Resolves by 12 weeks postpartum o Preeclampsia Pregnancy-specific condition in which hypertension and proteinuria develop after 20 weeks of gestation in a previously normotensive woman In the absence of proteinuria, preeclampsia may be defined as hypertension along with one of the following: Thrombocytopenia Impaired liver function New development of renal insufficiency Pulmonary edema New-onset cerebral or visual disturbances o Eclampsia (Toxemia) Onset of seizure activity or coma in a woman with preeclampsia No history of preexisting pathology 50% of eclamptic women develop the condition while pregnant Women can develop eclampsia in the immediate postpartum period o Chronic HTN Hypertension present before pregnancy or diagnosed before week 20 of gestation o Chronic HTN w superimposed preeclampsia Women with chronic hypertension may acquire preeclampsia or eclampsia Can be difficult to diagnose o HELLP Syndrome What is preeclampsia? o Pathophysiology remains unclear but the placenta is at the root cause Key features involve uterine spiral arteries Failure to transform from thick-walled muscular vessels to thinner sac-like flaccid vessels, which increases blood volume capacity of the vessels Maternal vasospasm: decreased perfusion to all organs, including decreased placental perfusion Increased platelet activation by endothelial cells More sensitive to pressor agents Decreased renal perfusion (pg. 657) Low-dose ASA (acetylsalicylic acid) may result in modest risk reduction PEC also affects the growing fetus What are the risk factors for getting preeclampsia? o Risk factors: HTN, DM, kidney disease, autoimmune disease Hx of preeclampsia First pregnancy New paternity Age Race Obesity Multiparity Signs and symptoms as well management of preeclampsia. o S/S: Headaches Epigastric pain Right upper quadrant abdominal pain Visual disturbances o Management: Identifying and preventing preeclampsia No reliable test or screening tool has been developed Low-dose aspirin (60 to 80 mg) may help certain high risk women Potential biomarkers being investigated Tyrosine kinase (sFLt) and serum placental growth factor Abnormal uterine artery Doppler velocimetry in the first or second trimester of pregnancy Assessment and nursing diagnoses Accurate measurement of BP Assessment of edema, although the presence of edema is no longer included in the definition of preeclampsia Deep tendon reflexes (DTR’s) Assess for hyperactive reflexes (clonus) Proteinuria: ideally determined by evaluation of a 24-hour urine collection Mild gestational hypertension and preeclampsia without severe features Goals of therapy are to ensure maternal safety and deliver a healthy newborn close to term. Home care Maternal and fetal assessment Activity restriction Diet Review Magnesium sulfate as well as it's antidote. o To prevent seizure, respiratory depressant, affinity w kidneys Measure I&Os q hour, foley, dropping -- toxicity Monitor RR, o Contraindications: Pulmonary edema End-stage renal disease Myasthenia gravis Hypocalcemia o Antidote: calcium gluconate What is the difference between preeclampsia and eclampsia? o Preeclampsia o Eclampsia onset of seizure activity or coma in a woman with preeclampsia What is HEELP syndrome? o Laboratory diagnosis for a variant of severe preeclampsia that involves hepatic dysfunction Hemolysis (H) Elevated liver enzymes (EL) Low platelets (LP) o HELLP syndrome occurs in 0.5% to 0.9% of all pregnancies. o 10% to 20% of women who have preeclampsia with severe features develop it. o Result of arteriolar vasospasm, endothelial cell dysfunction with fibrin deposits, and adherence of platelets in blood vessels o The clinical presentation is often nonspecific; most women with the disorder report the following: History of malaise Influenza-like symptoms Epigastric or right upper quadrant abdominal pain Symptoms worsen at night and improve during the daytime. Chapter 12: Hemorrhagic disorders: What are the different types of spontaneous abortion and its management? Review cervical incompetence and the management. o Cervical Insufficiency: painless dilation of cervix, without contractions Etiology Passive and painless dilation of the cervix during the second trimester May be either acquired or congenital o Diagnosis o o o o o o Speculum/digital pelvic exams; transvaginal U/S Cervical funneling Women presents with: Advanced effacement & dilation Bulging or hourglass membranes Backache Unsure of Causes: Congenital Hormonal Acquired Medical Therapies for high-risk patients include: Serial sonograms, Progesterone supplementation, Antibiotics Cerclage Procedures: McDonald procedure a purse-string technique is placed high up in the cervix and then tied closed. (12,3,6,9 and tied at 12 o’clock) Shirodkar procedure places a submucosal band at the level of the internal os. Abdominal Cerclage: band is placed around cervix through abdomen. (pg. 675) Care management Cerclage: may be placed either prophylactically or as a therapeutic or rescue procedure after cervical change has been identified Removed by 36 weeks of gestation Follow-up care Bed rest for a few days following cerclage Watch for and report signs of preterm labor, rupture of membranes, and infection. What is ectopic pregnancy? o Ectopic pregnancy: the fertilized ovum is implanted outside the uterine cavity; also called “tubal pregnancies” Incidence and etiology Clinical manifestations Typically s/s occur 6 to 8 weeks after the last normal menstrual period The three most classic symptoms are the following: 1. Abdominal pain 2. Delayed menses 3. Abnormal vaginal bleeding (spotting) Ectopic pregnancy Diagnosis: Difficult differential diagnosis: numerous disorders share similar signs and symptoms Quantitative β-hCG levels and transvaginal ultrasound examination; progesterone level How is ectopic pregnancy managed? o Tubal pregnancy management o Medical management: methotrexate: folic acid antagonist that interferes with the proliferation of trophoblastic cells o Surgical management: Laparoscopic linear salpingostomy, to gently evacuate the ectopic & preservation of tube Laparoscopic salpingectomy (removal of the tube) o Follow-up care Review hydatidiform mole and the management. o Hydatidiform mole (molar pregnancy) Type of gestational trophoblastic disease GTD is the pathologic proliferation of trophoblastic cells o Benign proliferative growth of the placental trophoblast in which the chorionic villi develop into edematous, cystic, avascular transparent vesicles that hang in a grapelike cluster o Incidence and etiology Occurs in 1 in 1000 - 1500 pregnancies in the United States Cause is unknown o Types Complete: no embryonic or fetal parts Partial: often have embryonic or fetal parts and an amniotic sac o Clinical manifestations Anemia from blood loss, excessive nausea, and vomiting (hyperemesis gravidarum), and abdominal cramps o Diagnosis Transvaginal ultrasound and serum hCG levels o Care management: suction curettage o Nursing interventions o Follow-up care Contrast between placenta previa and placental abruption. o Placenta Previa - Placenta improperly implants low in the uterus or over the cervix Low-lying: Placenta implanted in lower segment, close to the internal os but not covering it. Marginal: Edge of placenta is at the margin of the internal os. Partial: Internal os is partially covered by placenta Total Placenta previa: Internal os is covered completely. PAINLESS Bright Red Vaginal Bleeding! Cause: unknown but associated with: previous previa, multiparity, increasing age, placenta accreta, prior cesarean or other uterine surgery. NO vaginal exams, confirm diagnosis by ultrasound Monitor vaginal bleeding, pain & uterine contractions, vital signs, FHR IV access, complete lab work, Type & Cross matched for 2-4 units RBC’s Incidence and etiology 1 in 200 pregnancies Maternal and fetal outcomes Major complication is hemorrhage Fetal death (caused by preterm birth) Stillbirth, malpresentation, fetal anemia, intrauterine growth restriction (IUGR) Care management Expectant management Home care Active management o Placental Abruption (abruptio placenta; Couvelaire uterus) - premature separation of placenta from normal implanted placenta. Symptoms: Pain, Rigid Abdomen, Vaginal bleeding, Uterine Irritability 1% of all pregnancies, 15% of perinatal mortality. (Occurs in 1 in 75 to 1 in 226 pregnancies) Three types: Marginal: partially separation, vaginal bleeding, tenderness Central: concealed bleeding, Extreme abdominal tenderness Complete: total separation, rigid, board-like abdomen, increasing in size Classification systems: Grades 1 (mild 10-20%) Grades 2 (moderate 20-30%), 3 (severe >50%) Detachment of part or all of placenta from implantation site after 20 weeks of gestation Maternal hypertension is a primary risk factor Greater frequency with: smokers, PROM, multiple gestation, advanced maternal age (AMA), cocaine use, Chorioamnionitis, & hypertension. Other causes: Domestic violence, trauma to abdomen, fibroids, fetal growth restriction, short cord, & high parity Review clotting disorders in pregnancy such as DIC. o Disseminated intravascular coagulation (DIC) Pathologic form of diffuse clotting that consumes large amounts of clotting factors, causing widespread external bleeding, internal bleeding, or both; a condition in which blood clots form throughout the body, blocking small blood vessels. Symptoms may include chest pain, shortness of breath, leg pain, problems speaking, or problems moving parts of the body Never a primary diagnosis: Result of other acute or traumatic event Care Management & Nursing Intervention Correction of the underlying causes Abruption, HELLP, S-PEC, Anaphylactoid syndrome, PPH & w other clotting problems o Placenta Accreta Accreta: Chorionic villi attach directly to the myometrium of the uterus (most common) Adherence may be total, partial or focal 1 in 3500 births Increta: the myometrium is invaded Percreta: the myometrium is penetrated Treatment: IR (interventional radiology) & Hysterectomy Chapter 12-2: STIs: o Review all the STIs; the management of the STIs and ways to prevent them. o What are the primary and secondary means to prevent STI? o Primary prevention: Primary prevention the most effective way of reducing STIs in women o Secondary prevention: Prompt diagnosis and treatment can prevent personal complications and transmission to others o Review PID and its symptoms. o Pelvic Inflammatory Disease (PID) Symptoms Bilateral sharp, cramping pain in lower quadrants Fever greater than 101°F, chills Mucopurulent cervical or vaginal discharge Irregular bleeding Cervical motion tenderness during intercourse Malaise, nausea, vomiting Screening and diagnosis History CDC routine criteria Management Prevention Hospitalization Education Treatment Intravenous (IV) fluids, pain medication, IV antibiotics PO medication once acute symptoms resolve Treat sexual partner o Also review HPV, HSV, HIV and TORCH infections. o Human papillomavirus (HPV) (Condylomata acuminata) (Condylomata acuminata) Affects 20 million Americans Most prevalent viral STI seen in ambulatory health care settings Previously named genital or venereal warts More frequent in pregnant women Screening and diagnosis: History of known exposure Physical inspection Pap smear Viral screening and typing for HPV are available but not standard practice. Management Removal Medications Counseling o Herpes simplex virus (HSV) Transmission is nonsexual o Herpes simplex virus 2 (HSV-2) Transmitted sexually Initial infection characterized by multiple painful lesions, fever, chills, malaise, and severe dysuria Chronic and recurring disease for which there is no known cure Systemic antiviral medications partially control the symptoms Maternal infection with HSV-2 can have adverse effects on mother and fetus Neonatal herpes Most severe complication of HSV Most mothers lack history of HSV Given Acyclovir (Valtrex) @36w for suppression o Human immunodeficiency virus (HIV) Transmission of HIV occurs primarily through exchange of body fluids Severe depression of the cellular immune system associated with HIV infection characterizes AIDS Symptoms: fever, headache, night sweats, malaise, generalized lymphadenopathy, myalgia, nausea, diarrhea, weight loss, sore throat, and rash Screening and diagnosis Antibody testing Detection Counseling for HIV testing Counseling before and after HIV testing is standard nursing practice today HIV testing offered early in pregnancy Perinatal transmission decreases Consider confidentiality and documentation Pretest and posttest counseling Notification of results HIV and pregnancy HIV counseling and testing should be offered to all women at their initial entry into prenatal care as part of routine prenatal testing unless the woman opts out of the screening (CDC, 2010c). Perinatal transmission has decreased because of antiretroviral prophylaxis. Decreases transmission to 1% to 2% Intrapartum zidovudine (AZT IV) Cesarean birth is recommended for those patients with a high viral load. o TORCH Infections A group of infections capable of crossing the placenta and adversely affecting the fetus: Toxoplasmosis no cat litter, garden w gloves on Other infections (e.g. Hep, HIV) Rubella virus Cytomegalovirus Herpes Simplex Virus (HSV) Chapter 13: Processes, Phases and Stages of labor/ Birth Know the 5 P’s. o Passenger Presentation - the fetal part that enters the pelvis first (cephalic, breech, shoulder) Lie (the orientation of the long axis of the fetus to the long axis of the woman) Attitude - relation of body parts to another. Normal: flexion; head to chest arms and legs over thorax. Position - location of fixed reference point on the presenting part in relation to the four quadrants to the maternal pelvis o Passageway o Powers - contractions o Position of mother o Psychology What consists of the birth passageway, passengers & powers? o Passage - birth canal o Passengers - fetus and placenta o Powers - contractions What is the classic pelvis? o Deeply curved sacrum and blunt ischial spines Know the 3 phases & 4 stages of labor & delivery. o 1st Labor Stage Latent Phase Physiologic Changes o regular, mild contractions begin and increase in intensity and frequency o cervical effacement and dilation begins o 1-3cm Psychological Changes o relief that labor has begun o high excitement with some anxiety Active Phase Physiologic Changes o Contractions increase in intensity, frequency, and duration o cervix dilates from 4-7cm (epidural offered) o fetus begins to descend into pelvis Psychological Changes o fear of loss of control o anxiety increases Transition Phase Physiologic Changes o intensifying contractions 2 min lasting about 60s apart o cervix dilates 8-10cm o fetus descends rapidly into birth passage o rectal pressure o N/V Psychological Changes o anxiety o irritability o eager to complete birth experience o needs to have a support person or nurse at bedside o 2nd Labor Stage Physiologic Changes Begins with complete cervical dilation and ends with birth of infant Psychological Changes May feel a sense of purpose May feel out of control, frightened, and irritable Cardinal Movements of Labor Every Darn Fool In Egypt Eats Raw Egg Engagement Descent Flexion Internal rotation Extension Restitution External Rotation Expulsion o 3rd Labor Stage Physiologic Changes Placental separation: Uterus contracts and placenta begins to separate Placental delivery: Woman bears down and delivers placenta – physician may put slight traction on cord to assist delivery of placenta Quick sweep for cord - cord clamp for tight cord Psychological Changes Woman may feel relief at completion of birth Woman usually focused on welfare of infant and may not recognize that placental expulsion is occurring o 4th Labor Stage Physiologic Changes increased pulse, decreased bp -- redistribution of blood from uterus and blood loss uterus remains contracted and located between umbilicus and symphysis pubis shaking chill urine retention due to decreased bladder tone and possible trauma Psychological Changes euphoria and energy thirsty and hungry What are the CARDINAL MOVEMENTS of labor? o o o o o o o Descent flexion internal rotation extension restitution external rotation expulsion How does the baby’s position & presentation affect delivery? o Breech Complete Frank Footling o Occiput Anterior (OA) o Occiput Posterior (OP) - severe pain o Transverse Know the nursing care/ responsibilities at different stages. o 4th Stage: keep eye on bladder (will impede fetal head descent), straight cath; full bladder will cause postpartum hemorrhage, palpate bladder (should be nonpalpable), eat and drink as tolerated What does SROM, PROM & AROM stand for? o Spontaneous/Premature/Artificial Rupture of Membrane What are your nursing interventions after amniotomy or ROM? o Chucks, Monitor FHR What are the forces of labor and the signs of labor? Contractions & Pushing Signs of Labor o Lightening o Braxton Hicks contractions (irregular) o Contractions increase in frequency and duration ○ Cervical changes o ROM o Loss of 1-3 lbs o Nesting - sudden energy burst o Blood show Review the different types of pelvises. o o o o Anthropoid Gynecoid Platypelloid Android Chapter 13: Nursing Care during labor Nursing care during the 3 phases & 1 stage of labor includes assessments, nursing interventions. o Assessments Database Assessment Physical examination Leopold's maneuvers What is the nurse’s responsibility during admission and throughout the labor process? Include position changes, comfort measures as discussed in previous chapters. o Establish a therapeutic relationship Make family feel welcome Determine family expectations Convey confidence Respect cultural values o Assess the condition of the mother and fetus o Notify birth attendant GPAL fundal height and EDB contraction pattern VE results cervical dilation and effacement Fetal presentation and position FHR Maternal V/S identified abnormalities o o o o pain or anxiety Consent forms anesthesia, vaginal birth/C-section, blood transfusion, HIV test, if woman wants sterilization, newborn care, and circumcision Laboratory tests (Hct, mid-stream urine, HIV) Establish an intravenous (IV) access (18 gauge) Enema (if ordered) What are the signs of placental separation after delivery of the baby? o Signs: Globular abdomen (spherical) Lengthening of cord Sudden gush of blood Sudden urge to push placenta out (within 5-30min of delivery of baby, if not placental retention) Chapter 14: Pain assessment and maximizing comfort: What are factors affecting response to pain? o Perception of Pain: Pain tolerance, gate-control theory of pain o Expressions of Pain: physiologic effects, sensory/emotional responses o Cultural Norms Perceptions of pain impulses are individual Diverse cultures express pain in many ways o Anxiety Increased discomfort Magnifies pain perception o Previous experience Effects ability to manage pain o Fatigue/ sleep deprivation Less energy to cope with pain Review non-pharmacologic means of pain management and pharmacological. o Preparation for childbirth to reduce anxiety Reduced need for analgesia Breathing techniques Good continuous support from caregivers & partners o Non-pharmacological recommendations: Ambulating in early labor Sitting in a chair at the bedside Paced breathing techniques Encourage focus outside of self & the pain, effleurage Frequent emptying of the bladder, Frequent peri care, linen changes Repositioning using pillows Lip gloss, mouthwash for dry mouth Back rub, warm showers o Benefits: Prevention & Wellness Non-invasive Healing vs. Cure Cost & Access o Traditional Chinese Medicine Acupuncture/Acupressure o o o o o o o o o Herbal Therapy Mind-Body Therapies Hypnosis/Biofeedback/Meditation Chiropractic Reflexology/Massage/Yoga Hydrotherapy Risks: Lack of regulation Lack of research Inadequate training/certification Naturopathy Homeopathy Music therapy Aromatherapy What are factors to consider prior to administration of analgesic medications? o Sedation effect on Mother o Sedation effect on Fetus o Medical status of mother o Progress of labor o Effect on contractions o Half-life of medication o Types of meds: Sedatives Barbiturates Benzodiazepines H1-Receptors Narcotic Analgesics Nitrous Oxide (pg. 403) Review the various types of regional anesthesia, contraindications and the nursing intervention. o Regional anesthesia is the temporary and reversible loss of sensation produced by injecting an anesthetic agent into direct contact with nerve impulses. o Types: Epidural Intrathecal (Spinal) Combined Intrathecal & Epidural General Anesthesia Pudendal Nerve Block Local Perineal Infiltration o Contraindications: Absolute CONTRAINDICATIONS: Maternal refusal Local or systemic infections, Uncorrected hypovolemia. Allergy to specific local anesthetic agents. Coagulation disorders, (platelets below 100,000/mm.) o Relative Contraindications: Increased Intracranial Pressure Sever anatomic abnormalities, Sepsis Uncooperative patient o Interventions: Explain side effects of medications to patient Consent & Time out for all procedures Assist with positioning patient for regional anesthesia Pre-hydration of IV fluids Monitor vital signs frequently, during & after procedure Assess for urinary retention/ distention Re-position with left lateral displacement Ensure Patient safety after medication: Side rails up Call bell within reach Inform family not to get patient OOB. What is Narcan? o Used for the reversal of narcotics which can cause respiratory depression in mother or baby. Fentanyl short-acting opioid, rapid onset usually used by anesthesia o Naloxone Chapter 15: Intrapartum Nursing Assessments/ fetal monitoring. Review the nurse’s responsibility with a maternal assessment: o physical assessment o labor progress o social & cultural assessment for normal pregnant women o determining high-risk patients. What is Leopold’s Maneuvers? o Systematic palpation of the uterus to determine positioning, presentation, and engagement. Electronic fetal heart rate monitoring (EFM) & contraction monitoring: what are the 2 types available? when are they used or not used? o Contractions Noninvasive External monitoring: Tocodynameter (Toco) o placed on fundus Invasive internal monitoring: Intrauterine pressure catheter (IUPC) o more accurate o placed inside by MD or CNM after ROM o Fetal Heart Tone Fetoscope Doppler Electronic Monitoring How do you describe labor contractions? o Resting tone, frequency, duration, intensity, How do nurses document uterine activity? o Assess frequency, duration, intensity of contractions. Dilation, effacement, station, engagement, and presentation, pain level, What is frequency, duration, and intensity of contractions? o Frequency: Assess from the beginning of one contraction to the beginning of the next contraction o Duration: Place one hand on the fundus, note the time the uterus begins to tense and when relaxation occurs o Intensity: Estimate intensity of contractions by comparing indent ability of the fundus to: The tip of the nose for mild contractions The chin for moderate contractions The forehead for strong contractions o Resting tone: relaxation time between two contractions Know normal baseline parameters and variations of fetal periodic changes in fetal HR’s. o o o o o o o o o o o o o Baseline: 110-160 bpm over a 10 minute period, excluding periodic or episodic changes Variability: changes in baseline by 5-25 bpm over a 2-10minute period Tachycardia: sustained FHr above 160bpm Bradycardia: FHR belows 110bpm lasting 2-10min or longer Prolonged bradycardia: lasts over 10 min Category I: FHR baseline between 110-160bpm, moderate variability, no late or variable decels, accelerations & early decelerations present or absent Category II: All tracings not categorized as I or III Category III: Absent variability with any of the following: Recurrent Late decelerations Recurrent variable decelerations Bradycardia Sinusoidal pattern Periodic changes occur with contractions Episodic changes occur without contractions Accelerations: Transient increases in FHR usually caused by fetal movement. It is a sign of fetal well-being. (15bpm up by 15 bpm wide) Decelerations: Periodic decreases in FHR, categorized by the time of occurrence with ctx Early: uniform, mirror the contractions (transient head compression) Variable: v shaped, vary in depth and occurrence, cord compression. Late: uniform in shape, occurs after ctx begins Non-reassuring FHR Patterns Prolonged: duration <2 minutes and >10 minutes (non-reassuring, FHR>15bpm deep x 15 bpm amplitude from 2-10 min; >10min=bradycardia) Sinusoidal pattern: similar to waveform, absence of variability Causes: fetal anemia, severe fetal hypoxia, maternal meds What are the nursing interventions for those changes, when they are used? o Change patient’s position to improve FHR pattern: left lateral, right lateral, knee/chest position (review uterine resuscitation) What is variability, accelerations & decelerations? o Variability changes in baseline by 5-25 bpm over a 2-10 min period o Accelerations Transient increases in FHR usually caused by fetal movement A sign of fetal well-being (15bpm up by 15 bpm wide) o Decelerations Periodic decreases in FHR, categorized by the time of occurrence with ctx Early: uniform, mirror the contractions (transient head compression) Variable: v shaped, vary in depth and occurrence, cord compression. Late: uniform in shape, occurs after ctx begins Prolonged: duration <2 minutes and >10 minutes What nursing interventions are used for Uterine Resuscitation? o Change patient’s position to improve FHR pattern Use left lateral, right lateral, or knee/chest position Increase IV fluids Notify MD or CNM Administer flow O2 via face mask @7-10L/min D/C pitocin if no improvement Assess pt for hypotension Assist with VE, AROM Explanation & support given to patient & partner Interpreting FHR patterns: What is the relationship between the fetal circulation (FHR), accelerations and decelerations? o Accelerations: Increase FHR, good o Decelerations: Periodic decrease in FHR USE VEAL CHOP: Variable decelerations Cord compression Early decelerations Head compression Accelerations OK/O2 Late decelerations insufficiency Placenta (Utero-placental)