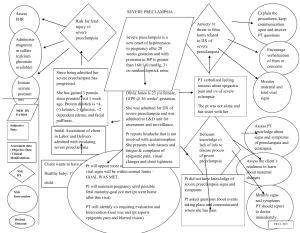
Definition o o o o o o o Gestational hypertension- new onset of SBP ≥140 mmHg /DBP ≥90 mmHg on at least 2 occasions 4 hours apart after 20 weeks of gestation in a previously normotensive woman & NO proteinuria/ NO features of preeclampsia followed by normalization of BP post-partum. Preeclampsia- New onset of SBP ≥140 mmHg or DBP ≥90 mmHg on at least 2 occasions at least 4 hours apart after 20 weeks of gestation in a previously normotensive woman or SBP ≥160 mmHg /DBP≥110 mmHg confirmed within a short interval (minutes) to facilitate timely antihypertensive therapy + proteinuria OR in the absence of proteinuria with new onset of HTN+ new onset of the following: (thrombocytopenia, renal insufficiency, elevated liver transaminases, pulmonary edema, persistent cerebral/ visual symptoms) Chronic HTN- HTN present before pregnancy/20 weeks of gestation OR HTN 1st diagnosed during pregnancy & persist atleast for12 wks postpartum, SBP ≥140 mmHg, DBP ≥90 mmHg, or both Superimposed PET on a chronic HTN- sudden increase in BP that was well controlled/ increase in therapy to control BP/ new onset of proteinuria or sudden increase in proteinuria in pt. with known proteinuria before/ early in pregnancy. Preeclampsia with severe features- preeclampsia + any of these findings: SBP ≥160 mmHg/ DBP ≥110 mmHg on 2 occasions at least 4 hrs apart while a patient is on bed rest (unless antihypertensive therapy is initiated before this time), thrombocytopenia, liver dysfunction, progressive renal insufficiency, pulmonary edema, persistent cerebral/ visual disturbances. Eclampsia- preeclampsia+ generalized seizure that cannot be attributed to other causes. HELLP- variant of preeclampsia suggested by microangiopathic findings (hemolysis, elevated liver enzymes, low platelets) Clinical Features History- GA->before 20 wks-chronic HTN, new onset/worsening HTN after 20 wkspreeclampsia that co-exist with proteinuria/ maternal dysfunction/ uteroplacental dysfunction, new onset HTN after 20 weeks without co-existing complication-gestational HTN, if dx of severe HTN/ preeclampsia in 1st/ early 2nd trimester- r/o gestational trophoblastic disease. Preeclampsia- visual disturbance (scintillations and scotomata), new-onset headache (frontal, throbbing/ similar to a migraine headache) & GI complaint (sudden, new-onset, constant epigastric pain), rapidly increasing /nondependent edema, reduced urine output, nausea & vomiting Measure BP in sitting position-≥140/≥90mmHg, ophthalmic finding- retinal edema, retinal vasospasm, impaired vision, RUQ abdominal tenderness, CNS finding- clonus. Chronic HTN- Signs- Centripetal obesity, buffalo hump/ wide purple abdominal striae =>glucocorticoid excess/ clinical signs /demonstrating hyperthyroidism, hypothyroidism, /growth hormone excess. systolic bruit over the abdomen /flanks =>renal artery stenosis, radio femoral delay /diminished pulses in the lower versus upper extremities =>coarctation of the aorta. Signs of end-organ damage -presence of S4 on cardiac auscultation =>LVH/ diastolic dysfunction due to preeclampsia-induced vasospasm. Carotid bruits => atherosclerotic disease due to longstanding hypertension, and Retinal changes of chronic hypertension. Investigation- urinalysis, CBC (Thrombocytopenia-<100,000/microL, and serum sodium, potassium, creatinine, and glucose, creatinine clearance, blood urea nitrogen (BUN), albumin, 24-hour urinary protein, serum calcium, uric acid, glycosylated hemoglobin, TSH, liver enzymes and bilirubin, and a urine dipstick for protein. Spot urine for protein- creatinine ratio=> >0.3mg/dl / >300mg/day-> preeclampsia. Ultrasound assessment of fetal growth, amniotic fluid volume and umbilical artery Doppler assessment. Management -don’t routinely admit to hospital -Antihypertensive therapy should be initiated for BP ≥ 160/105. -aim for BP 135/85mmHg or less -measure BP & dipstick proteinuria once/2x /wk until BP is 135/85 or less -FBC, LFT, RFT at presentation & then weekly (Assess development of preeclampsia) -patient education & counselling -ask mother to monitor fetal movement daily -timing of delivery at 37+0- 38+6 weeks Pathophysiology of preeclampsia Abnormal development of placenta, shallow cytotrophoblast migration toward the uterine spiral arterioles, defective trophoblast differentiation => placental hypoperfusion & ischemia=> fetal growth restriction, increased secretion of sFlt-1 & soluble endoglin, decreased availability of VEGF, PlGF, other mediators of endothelial dysfunction, oligohydramnios => systemic endothelial dysfunction(vasoconstriction & decreased blood-flow to organs)=> HTN, platelet activation, CNS changes, edema, glomerular endotheliosis, proteinuria & renal insufficiency, hemolysis, hepatic ischemia & necrosis. -Systemic endothelial dysfunction of maternal blood vessels=> abnormal systemic arterial vasoconstriction=> new onset HTN. -Abnormal systemic arterial vasoconstriction=> blood accumulates in venous system (hepatic veins) => liver enlargement=> stretches liver capsules & activates liver nociceptors/ hepatic hematoma or rupture=> abdominal RUQ pain -Abnormal systemic arterial vasoconstriction=> high pressure in intracranial arteries=> stimulate vomiting center=> nausea/ vomiting OR liver damage and dysfunction=> abdominal distress=> nausea/ vomiting. -Abnormal systemic arterial vasoconstriction=> raised ICP=> headache/ stroke or TIA/ visual changes -Vascular dysfunction in brain damages cerebral tissue=> hyperactive, hypersynchronous electrical activity in the cortex=> eclampsia -Vascular dysfunction in brain damages cerebral tissue=> damage to UMN=> decrease inhibition of LMN that mediate reflexes=> hyper-reflexia with clonus. -Systemic endothelial dysfunction=> abnormal increase in vascular permeability=> rate of fluid leaking out of vessels> rate of fluid reabsorbed=> pulmonary edema=> SOB. -Glomerular endothelial dysfunction=> vasoconstriction of afferent arterioles in kidney nephrons/ decreased glomerular filtration=> reduced urine output. -Placenta under-perfusion and ischemia=> more fragile vascular connection between placenta & uterus=> easier separation of decidual basalis uterine layer from fetal vessels=>placental abruption=> uterine tenderness & PV bleeding. Lab test • • • • • • • • • • • Uric acid- if the kidneys have been damaged by preeclampsia, uric acid levels in the blood may rise. Hematocrit- A high hematocrit value can be a sign of preeclampsia; preeclampsia often causes the body's tissues to absorb blood plasma=> becomes more concentrated=> abnormally high hematocrit value. Platelets- Preeclampsia may cause an abnormally low platelet count (<100,000/microL) Partial thromboplastin time (PTT)-Preeclampsia can cause problems with blood clotting that increase the partial thromboplastin time. Electrolytes-eg. sodium, potassium, magnesium, calcium, and chloride, amounts of electrolytes in the body may change if preeclampsia is causing kidney damage or is causing fluid to leak out of blood vessels into surrounding tissues (edema). Urine protein (24-hour urine protein or urine protein to creatinine ratio) – used to look for elevated protein in the urine BUN, serum creatinine – kidney function tests used to look for organ damage resulting from preeclampsia; serum creatinine will be measured frequently to monitor your condition. Alanine aminotransferase (ALT) and aspartate aminotransferase (AST) – elevated levels of these liver function tests may indicate organ damage from preeclampsia; ALT and AST will be measured frequently to monitor your condition. Peripheral blood smear – red blood cells are examined with a microscope for damage or abnormalities. Lactate dehydrogenase (LD) – elevated LD levels indicate tissue or cell damage, which occurs in the breakdown of red blood cells. Bilirubin – elevated levels of bilirubin are usually an indication of liver damage or red blood cell destruction (hemolysis). Principles of management of PET -Control the BP- Preeclampsia without severe features-> managed with twice-weekly BP monitoring, antenatal testing for fetal well-being and disease progression, and delivery by 37 weeks' gestation. Preeclampsia with any severe feature ->immediate stabilization and inpatient treatment with magnesium sulfate, antihypertensive drugs, corticosteroids for fetal lung maturity if less than 34 weeks' gestation, and delivery plans. monitor as inpatients or closely at home for 72 hours postpartum. -Control and prevention of eclampsia- Elevate bed side rails, place patient in the lateral decubitus position (physical restraints may be necessary), suction oropharyngeal secretions and vomitus, maintain airway, adequate oxygenation, and IV access, Fetal resuscitation involving maternal oxygenation, left lateral positioning, and continuous fetal heart rate monitoring is needed. Magnesium sulphate (IV or IM) ->Used as prevention if sustained SBP >160, DBP >110; proteinuria > 1g/24h or ≥ 3+ on dipstick; liver and/or renal impairment; coagulopathy. loading doses of 4 to 6 g intravenously over 20 to 30 minutes and maintenance doses of 1 to 2 g/hour (and up to 3 g/hour) -presence/surveillance of severe features of PET- Hospitalize until delivery, review findings from frequent maternal and fetal assessment throughout the day, monitor blood pressure every 4 hours, frequently assess maternal symptoms (eg, headache, vision changes, epigastric or abdominal pain, decreased fetal activity, vaginal bleeding). Symptoms of preeclampsia with severe features would warrant delivery, accurately record fluid intake and urine output to identify oliguria (defined as <500 mL over 24 hours), deteriorating kidney function (rising creatinine to above 1.1 mg/dL [0.1 mmol/L]) and persistent oliguria over 24 to 48 hours would warrant delivery, repeat lab test (CBC, serum creatinine, liver chemistry 2x weekly. -Fetal surveillance- Monitor with monthly ultrasounds to assess fetal growth after viability and fetal surveillance by biophysical profile weekly or non-stress test twice weekly. --Timing of delivery- Mild preeclampsia should be delivered at 37 weeks, Severe preeclampsia should be delivered after 34 weeks & Corticosteroids are given for fetal lung maturity where appropriate (IM Dexamethasone 6 mg 6 hourly 4 doses or 12 mg 12 hourly 2 doses. -Mode of delivery- cesarean delivery to a nulliparous woman with preeclampsia with severe features of <32 weeks of gestation having unfavorable cervix, given the relatively high frequency of abnormal intrapartum fetal heart rate tracings and low likelihood of a successful vaginal delivery. preeclampsia with features of severe disease, does not mandate immediate cesarean birth. -Counselling patient/ spouse- patient education on signs and symptoms & severity of disease & advice to monitor fetal movement daily, instruct correct procedure for woman who self-monitor, recommend lifestyle modification & follow prescribed medications regularly, advice spouse/ family members to provide intervention/ notify health-care provider immediately if severe symptoms occur, counsel for informed choice of post-partum family planning & next pregnancy should attend ANC services early to prevent and identify and appropriate management of preeclampsia. Induced labor maternal complications- uterine tachysystole, uterine hypertonus, caesarean section, uterine rupture, instrumental vaginal delivery, severe hypertension, worsening of pre-eclampsia, development of seizures and eclampsia and HELLP Syndrome, maternal vomiting, maternal diarrhea, fever, antibiotic use, and postpartum hemorrhage. fetal-neonatal complications -meconium-stained liquor, Apgar score <7 at 5 minutes, NICU admission, seizures, birth asphyxia, and stillbirth. C-section Risk baby to breathing problems and surgical injury, risk mother to infection, PPH, reaction to anesthesia, blood clots, wound infection, surgery injury, increase risk during future pregnancy & problems in future pregnancies, such as low-lying placenta, placenta accreta and damage to the wall of the womb. possible complications associated with this condition (and if left untreated) -liver, kidney and brain damage -bleeding problems -eclampsia -stroke -PPH -baby=> premature birth/ placental abruption Management of eclampsia Ensure airway, breathing and circulation (keep airway patent, establish IV line, monitor SaO2, insert catheter), protect airway & minimize risk of aspiration, place pt. on her left side & suction her mouth, immediately called skilled person for intubation, prevent maternal injury- close observation & use of soft padding & side rails on bed, administer magnesium sulphate-If the patient has already received a prophylactic loading dose and is receiving a continuous infusion when the seizure occurs, an additional 2 g should be given intravenously. Otherwise, a 4- to 6-g loading dose IV over 15 to 20 minutes, followed by a continuous infusion of 2 g per hour. Lorazepam and phenytoin may be used as second-line agents for refractory seizures Discharge advice -Post-partum mx of HTN- Monitor BP for 72hrs in hosp., equivalent outpt. surveillance, repeat BP assessment 7-10days postpartum & repeat BP earlier if symptoms, BP >160/100mmHg=> high dependency care & invasive monitoring, sustained BP≥150/100mmHg-start/ increase antiHTN drugs, sustained BP≥140/90mmHg-start anti-HTN drugs (labetalol/atenolol, nifedipine/amlodipine, ACEI) Methyldopa Should be discontinued postnatally due to its maternal side effect (sedation, postural hypotension, postnatal depression) -Family planning- POPs & levonorgestrel-releasing intrauterine system (Mirena) are appropriate options in women with hypertension. -Her future health & next pregnancy- counsel on the risk of recurrence, recurrence risk for gestational HTN-16-47%, recurrence risk for preeclampsia-2-7%