MedCram EKG Course
advertisement

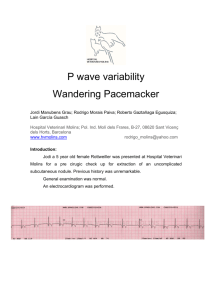
Atrial Fibrillation w/ rapid ventricular response (RVR, >100 bpm) or slow ventricular response (<100 bpm) => parasystolic event. Irregular No P waves Risk for strokes and PE => requires anticoagulation No “A” waves in JVP Wandering Atrial Pacemaker (W.A.T) Irregular HR <100 bpm P-waves look different Multifocal Atrial Tachycardia (M.A.T) Irregular HR >100 P-waves look different Does not require anticoagulation => in order to precisely differentiate may use methods to slow AV conduction. Escape Rhythms: occurs when there is a sufficient pause to allow a slower pacemaker to depolarize. Atrial Escape Rhythm Regular After pause, HR slightly slower than 60-80 and previous rhythm After pause, P-waves look different Narrow QRS <0.12 s Junctional Escape Rhythm Regular After pause, HR between 40-60 bpm No P-waves Narrow QRS *Retrograde P wave: may be present and can appear before, during or after the QRS complex. Retrograde P waves are usually inverted in the inferior leads. The electrical impulse travels forward, or in an antegrade direction, to produce a NORMAL QRS complex. Retrograde P waves that are very close to the QRS, or within it, are presumed to occur from a junctional rhythm, as the impulse leaves the ectopic pacemaker and travels forward and backward at the same time. *Accelerated Junctional Rhythm => regular, after pause = HR 60-80, no P-waves, narrowed QRS. Ventricular Escape Rhythm Regular After pause, HR between 20-40 bpm No P-waves Wide QRS *Ventricles are not affected by parasympathetic NS, unlike SA and AV node. Premature Atrial Contraction: focus in the atrium (not the sinoatrial node) generates an action potential before the next scheduled SA node action potential. After PAC, HR may be different after resetting of SA node. Abnormally shaped P wave (occurred outside of SA node) that appears before time according to previously regular P-P interval. Before PAC, P-P interval is regular; during PAC, P-P interval is irregular; after PAC, P-P interval is regular. Compensatory pause following contraction => the extra atrial action potential causes the SA node to become refractory to generate its next scheduled beat, and thus it must “skip a beat” and will resume exactly 2 P-P intervals after the last normal sinus beat. QRS complex changes depending on the prematurity of the atrial beat => o if AV node is not on refractory period => narrow QRS o if AV node is partially on refractory period => wide QRS o if AV node is on refractory period => no QRS *Atrial Bigeminy: pattern of heart beats that occurs in couplets. A regular (or sinus) beat is followed by a “premature” atrial beat. P wave typically has a different morphology and axis to the sinus P waves. Last P wave is the premature one. Last QRS is the widest one. Resetting of SA node occurs. Bigeminy — every other beat is a PAC. Trigeminy — every third beat is a PAC. Quadrigeminy — every fourth beat is a PAC. Couplet – two consecutive PACs. Triplet — three consecutive PACs. Premature Junctional Complex (PJC) Narrow QRS complex, either (1) without a preceding P wave or (2) preceded by an abnormal P wave with a PR interval of < 120 ms (these “retrograde” P wave are usually inverted in leads II, III and aVF). Occurs sooner than would be expected for the next sinus impulse. Followed by a compensatory pause. Bigeminy — every other beat is a PJC. Trigeminy — every third beat is a PJC. Premature Ventricular Complex (PVC) Broad QRS complex (≥ 120 ms) with abnormal morphology (mostly negative deflection as the direction of vector of foci in ventricle propagate in opposite direction). P waves are not affected. P-P interval are regular. Premature — i.e. occurs earlier than would be expected for the next sinus impulse. Discordant ST segment and T wave changes. Usually followed by a full compensatory pause. With a full compensatory pause, the next normal beat arrives after an interval that is equal to double the preceding R-R interval (see diagram below). Retrograde capture of the atria may or may not occur => concealed retrograde conduction, depolarization of AV node by ventricular extrasystole. Classification Unifocal — Arising from a single ectopic focus; each PVC is identical. Multifocal — Arising from two or more ectopic foci; multiple QRS morphologies. Patterns Bigeminy — every other beat is a PVC. Trigeminy — every third beat is a PVC. Quadrigeminy — every fourth beat is a PVC. Couplet — two consecutive PVCs. Triplet — three consecutive PVCs. >3 consecutive PVC = Ventricular Tachycardia. *Multifocal PVCs *Ventricular Bigeminy Tachyarrhythmias Paroxysmal Atrial Tachycardia (PAT, aka Paroxysmal supraventricular tachycardia, PSVT) Etiology: multiple causes including digoxin toxicity, atrial scarring, catecholamine excess, congenital abnormalities; may be idiopathic. Atrial rate 200 +/- 50 bpm. P wave morphology is abnormal when compared with sinus P wave due to ectopic origin. There is usually an abnormal P-wave axis (i.e. inverted in the inferior leads II, III and aVF). At least three consecutive identical ectopic p waves. QRS complexes usually normal morphology unless pre-existing bundle branch block, accessory pathway, or rate related aberrant conduction. Isoelectric baseline (unlike atrial flutter). AV block may be present — this is generally a physiological response to the rapid atrial rate, except in the case of digoxin toxicity where there is actually AV node suppression due to the vagotonic effects of digoxin, resulting in a slow ventricular rate => o “PAT with block”: Paroxysmal Junctional Tachycardia (Atrioventricular Nodal Reentrant Tachycardia, AVNRT – similar but not the same) Etiology: Digoxin toxicity (= the classic cause of AJR), Beta-agonists, i.e. isoprenaline, adrenaline, Myocardial ischemia, Myocarditis, Cardiac surgery. Atrial rate 200 +/- 50 bpm. Retrograde P waves inverted in II, III and aVF; upright in V1 and aVR. No visible P-waves (hidden within the QRS complex) or P-waves immediately before the QRS or P-waves immediately after the QRS complex. Short PR interval (< 120 ms) => junctional rather than atrial focus. Paroxysmal Ventricular Tachycardia (V-Tach) Etiology: CAD, aortic stenosis, cardiomyopathy, hypokalemia or hypomagnesemia, hypoxemia. Duration: Sustained = Duration > 30 seconds or requiring intervention due to hemodynamic compromise. Non-sustained = Three or more consecutive ventricular complexes terminating spontaneously in < 30 seconds. Features: Rapid heart rate (200 +/- 50 bpm). Broad QRS complexes (> 140 ms). Absence of typical RBBB or LBBB morphology. Extreme axis deviation (“northwest axis”, -90 to -180 degrees) — QRS is positive in aVR and negative in I + aVF. AV dissociation (P and QRS complexes at different rates). o Capture beats — occur when the sinoatrial node transiently ‘captures’ the ventricles, in the midst of AV dissociation, to produce a QRS complex of normal duration (<120 ms). o Fusion beats — occur when a sinus and ventricular beat coincide to produce a hybrid complex of intermediate morphology. Positive or negative concordance throughout the chest leads, i.e. leads V1-6 show entirely positive (R) or entirely negative (QS) complexes, with no RS complexes seen. Brugada’s sign – The distance from the onset of the QRS complex to the nadir of the S-wave is > 100ms. Josephson’s sign – Notching near the nadir of the S-wave. RSR’ complexes with a taller “left rabbit ear”. This is the most specific finding in favor of VT. This is in contrast to RBBB, where the right rabbit ear is taller. AV dissociation: P waves (arrowed) appear at a different rate to the QRS complexes. Capture beat: the sinus node “captures” the ventricles producing a narrow-complex beat. Fusion beats: the first of the narrower complexes is a fusion beat (the next two are capture beats). POSITIVE concordance in the precordial leads/ NEGATIVE concordance in the precordial leads Brugada’s sign (red callipers) and Josephson’s sign (blue arrow). Atrial or Junctional (Supraventricular) Tachycardia w/ Bundle Branch Block (BBB, aka Aberrancy) vs. Ventricular Tachycardia. *Typically, does pt. have CAD? Yes => V-Tach; QRS: <140 => PSVT vs. >140 => VT. *SVT w/ BBB can be treated w/ Beta-blockers vs. VT cannot be treated w/ Beta-blockers!!! Brugada Criteria Absence of an RS complex in all precordial leads (V1-6)? Yes => V-Tach. Precordial R waves only/Precordial S waves only Precordial RS waves => go to step 2 R to S interval >100 ms in one precordial lead? Yes => V-Tach. *<100 ms => go to step 3 AV dissociation? Yes => V-Tach. P waves can be spotted in between QRS complexes (circled) and superimposed upon the T wave causing a peaked appearance (arrow)/No AV dissociation => go to step 4 Morphology criteria for VT present both in V1-2 and V6? Yes => V-Tach or NO => SVT w/ Aberrancy (BBB). VT is frequently either in a right bundle branch block pattern (upright in V1) or a left bundle branch block pattern (downward in V1). If upward in lead V1 (RBBB pattern), then VT is present in the following situations: A monophasic R or biphasic qR complex in V1. If an RSR' pattern (“bunny-ear”) is present in V1, with the R peak being higher in amplitude than the R’ peak, then VT is present. An rS complex in lead V6 favors VT. If downward in lead V1 (LBBB pattern), then VT is present in the following situations: The presence of any Q or QS wave in lead V6 favors VT. A wide R wave in lead V1 or V2 of 40 ms or more favors VT. Slurred or notched downstroke of the S wave in V1 or V2 favors VT. Duration of onset of the QRS complex to peak of QS or S wave > 60 ms favors VT. Polymorphic VT and Torsades de Pointes (TdP) *Fatal rhythm Etiologies: prolonged QT interval (> 440 ms) => induced by medications such as Levaquin, Azithromycin, Amiodarone, Fluconazole, Zofran, Type 1A and Type III Antiarrhythmic drugs; congenital; hypokalemia, hypomagnesemia, hypocalcemia. Treatment: IV magnesium (initially), if not converted to NSR => asynchronized electrocardioversion. *The QTc rule of thumb is this: If the QT interval is less than half the RR interval, then the corrected QT (QTc) is not prolonged. *"R-on-T phenomenon" is the superimposition of an ectopic beat on the T wave of a preceding beat. Early observations suggested that R-on-T was likely to initiate sustained ventricular tachyarrhythmias. *TdP is initiated when a PVC occurs during the preceding T wave, known as ‘R on T’ phenomenon. *HR => 250-350 bpm Sinus rhythm with inverted T waves, prominent U waves and a long Q-U interval due to severe hypokalemia (K+ 1.7) A premature atrial complex (beat #9 of the rhythm strip) lands on the end of the T wave, causing ‘R on T’ phenomenon and initiating a paroxysm of polymorphic VT. Because of the preceding long QU interval, this can be diagnosed as TdP.