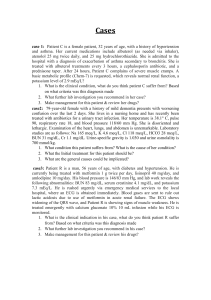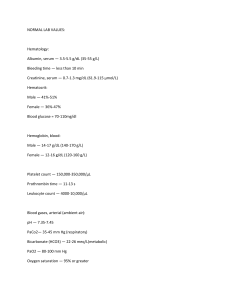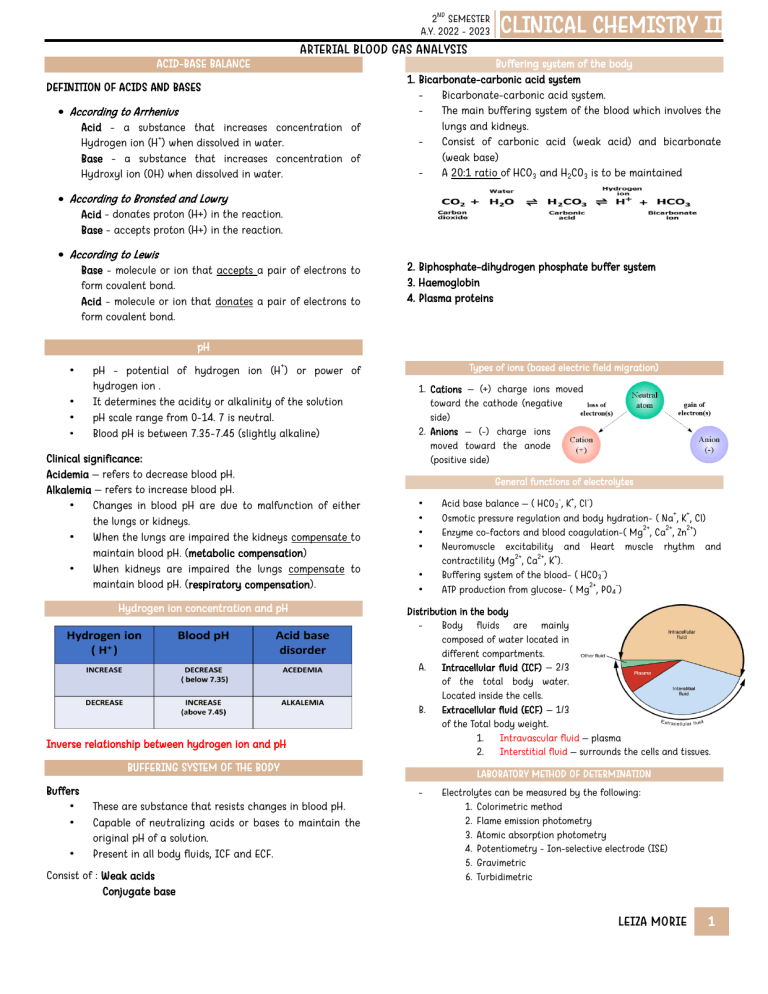
ND 2 SEMESTER A.Y. 2022 - 2023 CLINICAL CHEMISTRY II ARTERIAL BLOOD GAS ANALYSIS ACID-BASE BALANCE DEFINITION OF ACIDS AND BASES According to Arrhenius Acid - a substance that increases concentration of + Hydrogen ion (H ) when dissolved in water. Base - a substance that increases concentration of Hydroxyl ion (OH) when dissolved in water. Buffering system of the body 1. Bicarbonate-carbonic acid system - Bicarbonate-carbonic acid system. - The main buffering system of the blood which involves the lungs and kidneys. - Consist of carbonic acid (weak acid) and bicarbonate (weak base) - A 20:1 ratio of HCO3 and H2CO3 is to be maintained According to Bronsted and Lowry Acid - donates proton (H+) in the reaction. Base - accepts proton (H+) in the reaction. According to Lewis Base - molecule or ion that accepts a pair of electrons to form covalent bond. Acid - molecule or ion that donates a pair of electrons to form covalent bond. 2. Biphosphate-dihydrogen phosphate buffer system 3. Haemoglobin 4. Plasma proteins pH • • • • + pH - potential of hydrogen ion (H ) or power of hydrogen ion . It determines the acidity or alkalinity of the solution pH scale range from 0-14. 7 is neutral. Blood pH is between 7.35-7.45 (slightly alkaline) Clinical significance: Acidemia – refers to decrease blood pH. Alkalemia – refers to increase blood pH. • Changes in blood pH are due to malfunction of either the lungs or kidneys. • When the lungs are impaired the kidneys compensate to maintain blood pH. (metabolic compensation) • When kidneys are impaired the lungs compensate to maintain blood pH. (respiratory compensation). Hydrogen ion concentration and pH Inverse relationship between hydrogen ion and pH Types of ions (based electric field migration) 1. Cations – (+) charge ions moved toward the cathode (negative side) 2. Anions – (-) charge ions moved toward the anode (positive side) General functions of electrolytes • • • • • • • Consist of : Weak acids Conjugate base - LABORATORY METHOD OF DETERMINATION - These are substance that resists changes in blood pH. Capable of neutralizing acids or bases to maintain the original pH of a solution. Present in all body fluids, ICF and ECF. + Distribution in the body Body fluids are mainly composed of water located in different compartments. A. Intracellular fluid (ICF) – 2/3 of the total body water. Located inside the cells. B. Extracellular fluid (ECF) – 1/3 of the Total body weight. 1. Intravascular fluid – plasma 2. Interstitial fluid – surrounds the cells and tissues. BUFFERING SYSTEM OF THE BODY Buffers • • - Acid base balance – ( HCO3 , K , Cl ) + + Osmotic pressure regulation and body hydration- ( Na , K , Cl) 2+ 2+ 2+ Enzyme co-factors and blood coagulation-( Mg , Ca , Zn ) Neuromuscle excitability and Heart muscle rhythm and 2+ 2+ + contractility (Mg , Ca , K ). Buffering system of the blood- ( HCO3 ) 2+ ATP production from glucose- ( Mg , PO4 ) Electrolytes can be measured by the following: 1. Colorimetric method 2. Flame emission photometry 3. Atomic absorption photometry 4. Potentiometry - Ion-selective electrode (ISE) 5. Gravimetric 6. Turbidimetric LEIZA MORIE 1 ND 2 SEMESTER A.Y. 2022 - 2023 + CLINICAL CHEMISTRY II ARTERIAL BLOOD GAS ANALYSIS Sodium (Na ) Most abundant cation (90 %) in ECF less concentration in ICF. Regulated by hormone aldosterone through reabsorption from the kidneys. Functions: a. Maintain osmotic pressure, this prevents the cell from bursting. b. Water balance and maintain blood pressure. c. Neuromuscular excitability Levels are regulated by: ADH – water retention causes decrease of Na (dilutional hyponatremia). Aldosterone – increase secretion; increase Na reapsortion (hypernatremia) Thirst Normal value of sodium 1. Serum – 135- 148 mEq/L 2. CSF – 138-155 mEq/L Clinical significance Hyponatremia (< 135 mEq/L) - Due to increase sodium loss or increase water retention. - One of the most common electrolyte disorders. Symptoms: nausea, vomiting, muscle weakness, lethargy, headache, and ataxia. - <125 mEq/L – severe neuropsychiatric symptoms. Causes: Dehydration, vomiting, diarrhea, severe burns, metabolic acidosis, renal disease, Addison’s disease, syndrome of inappropriate ADH secretion (SIADH), nephrotic syndrome Pseudohyponatremia - Marked hemolysis decreased sodium level due to dilutional effect. - Hyperlipidemia and hyperprotenemia may also falsely decrease serum sodium (due dilutional effect). Hypernatremia (> 145 mEq/L) Increase sodium concentration due to loss of water, gain of sodium or both. Less common. Symptoms: altered mental status, lethargy, irritability, seizures, muscle twitching, hyper reflexes, difficulty in breathing and increase thirst. Causes: diabetes insipidus, renal disease, decrease water intake, fever, vomiting, alkalosis, severe burns, hyperadrenalism, diabetic coma. Specimen of choice: a. Serum b. Plasma c. 24 urine d. CSF e. Sweat Anticoagulant: Heparin Specimen consideration 1. Avoid hemolysis 2. Used for pure water to avoid trace contamination 3. Smoking increases sodium level 4. Prolong standing increases sodium level (shift to intracellular fluid) 5. oxalate decreases Na level 6. exercise decreases Na due to sweat 7. thumb or fingers must not use to cover tubes because it contains sodium Laboratory method Colorimetric method (Albanese and Lein) 1. sodium + zinc uranyl acetate = sodium uranyl acetate precipitate 2. sodium uranyl acetate precipitate + water + sodium salicylate = yellow precipitate Flame emission photometry – produce yellow color when exposed to flame. Ions selective electrode (ISE) – used glass aluminum silicate Reference value serum: 135-145 mmol/L 24 H urine: 40-220 mmol/L CSF: 138-150 mmol/L Conversion factor: mmol/L to mEq/L= 1.0 + Potassium (K ) Major cation in ICF and less in ECF. No renal threshold Functions 1. Muscle contraction both skeletal and cardiac. 2. Respiration. 3. Muscle irritability Reference value Serum: 3.5-5.5 mmol/L (adult) Infant: 4.0 – 5.9 mEq/L 24 H urine: 25-125 mmol/L mmol/L- mEq/L= 1.0 - Increase or decrease level of K may result to muscle weakness, paralysis and cessation of cardiac contraction. Clinical significance + Hypokalemia – decrease level of K Symptoms: weakness, fatigue, constipation, paralysis, difficulty in breathing. Causes: diarrhea, vomiting, renal disease, tumor, malabsorption, Cushing syndrome, hypomagnesemia, hyperaldosteronism, alkalosis. 3.0-3.4- mild hypokalemia The most common cause of hypokalemia due to increase activity of aldosterone (hyperaldosteronism) Diarrhea – causes direct K loss in the stool. Vomiting – mainly result of K loss in the urine. - Effects in cardiac muscle 1. Decreases cell excitability resulting to arrhythmia and paralysis 2. The heart may experience cessation in contraction in either hyperkalemia or hypokalemia. Alkalosis: decrease serum potassium Pseudohypokalemia Leukocytosis cause falsely decreases K. as seen in leukemia if sample left at room temperature. Causes: Hemolysis, thrombocytosis, prolong tourniquet application, fist clenching, blood stored in ice, IV fluid. + Hyperkalemia – Increased level of K Symptoms: muscle weakness, tingling, numbness, mental confusion, cardiac arrhythmias. Causes: renal disease, Addison’s disease, diuretics, muscle injury, acidosis, hypo aldosteronism, haemolytic disease. The most common cause of hyperkalemia is impaired renal excretion such as aldosterone deficiency and renal failure. Hyperkalemia LEIZA MORIE 2 ND 2 SEMESTER A.Y. 2022 - 2023 CLINICAL CHEMISTRY II ARTERIAL BLOOD GAS ANALYSIS 1. 2. 3. Acidosis : potassium increases Low insulin causes elevated serum potassium Hyperkalemic drugs: captopril, digoxin, heparin therapy. Effects on cardiac muscle 1. 8 mmol/L – lack of muscle excitability (ability to respond to stimulus) 2. 10 mmol/L – can lead to cardiac arrest. Specimen consideration 1. Hemolyzed sample must be avoided to prevent falsely elevated K. 2. ( K level inside the cell is very high) 3. Exercise increases K level to avoid this, let the patient rest for a few minutes before drawing blood sample. 4. Used pure water in analysis. 5. K level is slightly lower in plasma than in serum Laboratory method Colorimetric method (Lockhead and Purcell) – turbidity is proportional to the K concentration. Flame emission spectrophotometry – produces violet color when expose to flame. Ion-selective electrode (ISE) – used valinomycin gel Atomic absorption spectrophotometry Causes: hypothyroidism, hyperaldosteronism, bone cancer, antacids, dehydration, Addison’s disease, acute renal failure. Specimen: a. b. c. d. e. Specimen consideration 1. No venous stasis or tourniquet during collection 2. Avoid hemolysis because RBC contains 10x magnesium than serum/plasma 3. Physiologic increase in women with ecclampsia. Laboratory method Colorimetric method 1. Calmagite – produce violet color 2. Methyl – thymol blue 3. Titan yellow (Dye-lake method) 4. formazan dye (vitros machine) ISE AAS – reference method Fluorometric analysis – fluorescent compound + Magnesium (Mg ) 2 most abundant cation in the ICF. 53%- found in the bone, 46 %- found in muscle and other organs. Supplied by diet. 3 form in the blood a. 55 %- free magnesium b. 30 %- protein-bound c. 15 % - complexed Mg Functions 1. Muscle contraction and heart rhythm. 2. Enzyme co factors ( glycolysis, synthesis of carbohydrates, lipids, proteins etc) 3. Maintains the structure of DNA, RNA and ribosomes. nd Factors affecting magnesium in the blood PTH Increases renal reabsorption and intestinal absorption. Aldosterone and thyroxine Increases renal excretion. Reference value 0.63- 1.0 mmol/L 5.0 mmol/L- life threatening Clinical significance Hypomagnesemia most commonly observed in ICU patients and undergoing diuretic therapy. Symptoms: arrhythmia, psychosis, weakness, cramps, depression, seizure, tetany, paralysis. Causes: malabsorption syndrome (sprue), malnutrition, chronic alcoholism, hyperaldosteronism, hyperthyroidism, acute renal failure, severe diarrhea. Hypermagnesemia Symptoms: hypotension, bradycardia, increase temperature, nausea, vomiting, lethargy. Serum Plasma ( lithium heparinized) 24 urine Avoid using EDTA, oxalate, and citrate. Avoid hemolysis. 2+ - Calcium (Ca ) Only 1 % found in the blood the rest in the bones. Most abundant cation in the body Blood: 1. free calcium (ionized) the active form- 50 % 2. complex Ca-10 % 3. protein bound – 40 % - Calcium is absorbed in the small intestine. - Regulators of blood Cacium: Parathyroid hormone, calcitonin, and Vitamin D. - Renal threshold: >10 mg/dl Functions 1. 2. 3. 4. 5. Neurotransmitter regulator. Helps for proper contraction of the heart. For blood coagulation. Enzyme activator. Maintain bone and teeth structure. Factors influencing serum calcium level PTH (Parathyroid hormone) - mobilizing calcium from the bones - increase synthesis of 1,25-dihydroxycholecalciferol Calcitonin - produced by p-follicular cells of the thyroid gland - inhibits bone resorption by regulating the activity of osteoclasts - antagonist to PTH Active Vitamin D3 (active calciferol) - undergoes hydroxylation producing 1,25dihydroxycholecalciferol Plasma protein - direct relationship with calcium Serum/Plasma Phosphate - inverse relationship with calcium Other factors affecting calcium level LEIZA MORIE 3 ND 2 SEMESTER A.Y. 2022 - 2023 CLINICAL CHEMISTRY II ARTERIAL BLOOD GAS ANALYSIS Acidosis: decreases protein binding resulting to increase calcium Alkalosis: increases protein binding resulting to decrease calcium. Hypoclorenemia Clinical Significance Causes: DKA, aldosterone deficiency, vomiting, high serum bicarbonate. Metabolic alkalosis, diuretics. Hypocalcemia Symptoms: muscle cramps, tetany, seizures, and arrhythmia. Causes: primary hypothyroidism, vit D deficiency, renal failure, Fanconi’s syndrome, hypoalbuminemia, pacreatitis, alkalosis Hypercalcemia Symptoms: often asymptomatic, severe cases include mild weakness, lethargy, GI symptoms and renal discomfort. Causes: hyperthyroidism, acidosis, lung cancer, increase vit D, multiple myeloma, sarcoidosis. Specimen 1. Serum 2. Plasma- lithium anticoagulant 3. 24-hour urine Reference value Total calcium 2.20-2.70 mmol/L (children) 2.15-2.50 mmol/L (adult) Ionized calcium 1.20-1.38 mmol/L (children) 1.16-1.32 mmol/L (adult) Urine 2.50-7.50 mmol/day - Phosphate (PO4) Intracellular anion. most are in the form of inorganic phosphate (serum) In complex with magnesium and calcium 70% of plasma inorganic phosphorus is organic and 30% are inorganic. Majority of inorganic phosphate is excreted in urine and PTH favors urinary loss of phosphorus. Absorption in small intestines. Functions: 1. For intermediary metabolism of carbohydrates 2. Components of phospholipids, nucleic acid, nucleotide and inorganic phosphate esters 3. Bone mineralization - Functions: 1. Maintain water balance and osmotic pressure. 2. Acid-base balance 3. Maintenance of electrolyte balance/electroneutrality (Chloride shift)-exchange with HCO3 across the RBC membrane. 4. Hydration. Clinical Significance Serum Plasma- lithium heparinized Urine CSF Sweat Tears Colorimetric method 1. Schales and schales (mercuric nitrate titration method) produces paint violet color. 2. Mercuric thiocynate and ferric nitatre produce reddish color ISE method – used silver chloride- silver sulfide membrane. Coulometric (amphometric method) – measure by Chloridometer with silver ion - Chloride (Cl ) Major anion in the ECF. Counter ion of Na- always accompany Na to maintain electric neutrality. Lost or excreted in sweat. Only anion that enzyme activator – activates amylase Regulated by aldosterone. Reference range Plasma: 98- 107 mmol/L 24 H urine: 110- 250 mmol/dl Specimen: a. b. c. d. e. f. - ANIONS - Causes: metabolic acidosis, renal tubular acidosis, excess loss of bicarbonate, cystic fibrosis, CHF, hyperthyroidoism, severe diarrhea. Laboratory determination Laboratory determination 1. Orthocresolphthalein complexone dyes (colorimetric) 2. AAS- reference method 3. ISE- ion exchanger membrane or ionophore 4. Clark collip precipitation method- measure oxalic acid as the end point 5. Ferro Ham chloroanilic acid precipitation method 6. Compleximetric- removal of calcium by EDTA - Hyperchlorenemia Clinical Significance Hypophospathemia Causes: a. hyperparathyroidism b. rickets c. osteomalacia d. Fanconi’s syndrome Hyperphosphatemia Causes: a. hypoparathyroidism b. increase Vit D c. hypersecretion of growth hormone d. uremia e. glumerulonephritis Reference range At Birth Children Adult 1.34 – 3.35 mmol/L 1.28 – 2.24 mmol/L 0.96 – 1.44 mmol/L Specimen LEIZA MORIE 4 ND 2 SEMESTER A.Y. 2022 - 2023 CLINICAL CHEMISTRY II ARTERIAL BLOOD GAS ANALYSIS 1. 2. 3. 4. 5. Serum Plasma-lithium heparinized 24-hour urine Avoid hemolysis Circadian variation- highest in the morning Laboratory determination FISKE-SUBARROW METHOD (spectrophotometry) Reagent: Molybdate End color: Blue - Bicarbonate (HCO3 ) 2 most abundant anion in ECF nd - Functions: Major buffering system of the blood. Exchange with Cl across the RBC to maintain ionic charge neutrality within the cell (chloride shift). Clinical Significance Decrease in: Metabolic acidosis + HCO3 combines with hydrogen ion (H ) to produce CO2 which is exhaled by the lungs. SUMMARY ELECTROLYTES Anions (-) charge Cations (+) charge + + 2+ - 2+ - 2- Cl , HCO , PO Na , K , Mg , Ca 3 4 NORMAL VALUES Note: Normal values may vary slightly from other laboratories Electrolytes + Na N. V. 135-145 mEq/L Cl - 98-107 mEq/L + 3.4-5.0 mEq/L K 2+ Ca Total- 2.15-2.50 mmol/L Ionized- 1.16-1.32 mmol/L Mg 2+ 0.63- 1.0 mmol/L PO4 2- 0.87- 1.45 mmol/L HCO3 - 22-26 mEq/L LEIZA MORIE 5