Signs of Congestive Heart Failure on the Chest Radiograph Molly Lalor MS4
advertisement

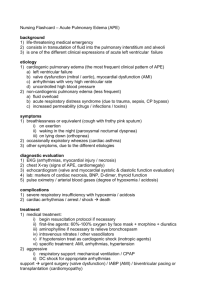
Signs of Congestive Heart Failure on the Chest Radiograph Molly Lalor MS4 OHSU Radiology Rotation November 2006 When should you use the Chest x-ray in CHF? ► The Chest Radiograph is a valuable tool for confirming signs of congestive heart failure and should be considered in patients with new or newly exacerbated clinical signs and symptoms of CHF1. ► Can you name signs and symptoms of CHF? CHF clinical symptoms and signs ►Symptoms: dyspnea on exertion, orthopnea, paroxysmal nocturnal dyspnea, peripheral edema, fatigue. (Palpitations, chest pain, diaphoresis etc. may occur depending on etiology). ►Signs: Left: bibasilar rales (crackles), S3 or S4, signs of peripheral hypoperfusion. Right: jugular venous distention, large pulsatile liver, abdominojugular reflex, peripheral edema. CXR in CHF: what can it show me? There are four main pieces of information to be gleaned from a chest radiograph regarding heart failure. ► Is ► Is there Pulmonary Edema? there evidence of long term pulmonary venous hypertension? ► What is my patient’s intravascular volume status? ► Is there heart chamber enlargement? depends on etiology of CHF. This presentation will not cover this topic. CXR: What can it show me? ► ► ► ► ► So first let’s consider pulmonary edema. Pulmonary edema is abnormal accumulation of extravascular lung water2,3. There are two major types/ mechanisms: hydrostatic edema and alveolar damage edema. There are other more rare mechanisms like endothelial damage edema, but we’ll consider the two most common. Mixed types can occur but we’ll keep them separate for simplicity. Pulmonary Edema = Abnormal Extravascular Lung Water* ► Again, because this is important: pulmonary edema can be caused by elevated hydrostatic pressure (CHF is in this category). ► Or, it can be caused by alveolar damage like in Adult Respiratory Distress Syndrome. ► On the following slide, look at the cartoon showing physiologic barriers against edema formation. Pulmonary Edema Barriers Alveolar air space alveolar epithelium with tight junctions Interstitium capillary endothemium with “loose” junctions lymphatics Capillary RBC lumen RBC Hydrostatic Pulmonary Edema high capillary pressure forces water molecules across endothelium (through loose junctions) into the interstitium and sometimes into the air space. Alveolar air space alveolar epithelium with intact tight junctions H2O Interstitium capillary endothemium with “loose” junctions lymphatics Increased RBC capillary Pressure RBC Hydrostatic Pulmonary edema: In this section of lung, septal capillaries are congested and the alveoli are filled with pink-staining proteinaceous edema fluid. Within the edema fluid there are macrophages, many of which contain hemosiderin pigment. These changes result from increased hydrostatic pressure in the pulmonary circulation, as is seen in left-sided heart failure or mitral stenosis. From www.pathology.vcu.edu/.../cardio/lab2.c.html Pulmonary Edema faculty.southwest.tn.edu/wray/images/ Hydrostatic Pulmonary Edema: Can you think of the causes of increased capillary hydrostatic pressure? Increased Arterial Pressure: more blood to push through the tube: Increased Venous Pressure: Capillary pressure •Left Heart (pump) failure with pressure backup *Left to right shunts •Hypertension (systemic) *Renal Failure •Veno-occlusive disease *etc •Etc. Alveolar Damage Pulmonary Edema: Not from CHF Water in the air space Alveolar air space Broken tight junctions alveolar epithelium with BROKEN tight junctions Interstitium lymphatics RBC RBC Pulmonary Edema continued ► So in considering your patient who may have CHF, evaluate his/her chest film for the mechanism of pulmonary edema: is it cardiogenic (hydrostatic) or is it from diffuse alveolar damage (ie there’s another process besides CHF going on.) ► Let’s look at some examples. Hydrostatic vs Alveolar Damage: you can usually tell them apart on chest radiograph! CHF: More whiteness (water) in lower lung areas due to higher capillary pressures lower down. Diffuse Alveolar Damage: all over whiteness from all over alveolar damage. ► Now that we’re clear that CHF manifests as hydrostatic pulmonary edema, what does that look like? *Vascular Indistinctness *Interlobular Fissure Thickening * Peri-bronchial Cuffing *Septal Lines (Kerleys) Pulmonary edema= abnormal extravascular lung water Note: peri-bronchovascular fluid cuff (imagine how this would blur the vessel margins on radiograph!) No edema Interstitial Edema Vascular Indistinctness Water is the same density as vessels, and so as it leaves vasculature for interstitium the margins become fuzzy. Crisp vessel margins, no edema Edema Vascular Indistinctness Crisp margins, no edema Edema Interlobular Fissure Thickening Edema in the lung along the fissure Peri-Bronchial Cuffing Peribronchial cuffing represents extravasated water surrounding the bronchus. Pre-diuresis: note the cuffing (large arrow) Post diuresis Septal Lines Thickened interlobular septae What about Cephalization? ► Cephalization means that the upper lung zone vessels look bigger than the lower lung zone vessels because more blood is flowing through the higher vessels. This is also called flow inversion. ► This phenomenon is the opposite of the normal gravity-dependent regional pulmonary blood flow. Cephalization The upper lobe vascular caliber is greater than lower vessels. Cephalization ► Many sources teach that cephalization (flow inversion) is an early and sensitive sign of acute pulmonary edema or acute CHF4-7. This teaching is likely based on studies of chronic mitral stenosis patients. ► However, studies have shown that cephalization is not well correlated with acute pulmonary hypertension in acute MI3,9,10, and that flow inversion remains after diuresis8. ► Ketai and Godwin in a review conclude that cephalization is almost never seen unless there is chronic pulmonary venous hypertension3 . Cephalization ► Pistolesi et al (1988) found that flow inversion correlated positively with pulmonary vascular resistance and not with wedge pressure, edema, or arterial oxygen tension8. ► Therefore, cephalization likely reflects chronic structural changes in the dependent lung vasculature (like reduction of cross sectional area)3,8. Cephalization ► So what does that all mean? ► If you see cephalization it means your patient likely has a chronic process causing pulmonary venous hypertension. ► Cephalization is not a sign of pulmonary edema. Intravascular Volume Status The vascular pedicle (mediastinal width above top of aortic arch) represents the superior vena cava on the patient’s right and the left subclavian artery on the left. If it is wide, that indicates greater intravascular volume. Look at the example on the following slide. Intravascular Volume Status Pre-dialysis Post-dialysis Quiz Time! ► For the following chest xrays, practice deciding if you think there is pulmonary edema-hydrostatic or alveolar damage. ► Answers at the end. #1 #2 #3 #4 #5 #6 #7 Quiz Answers ► #3 and #5 show hydrostatic pulmonary edema. ► #6 shows alveolar damage pulmonary edema. ► Bonus: #7 demonstrates cephalization. References ► ► ► ► ► ► ► ► ► ► 1. American College of Radiology Committee on Appropriateness Criteria for Congestive Heart Failure, 2006. 2. Reading the Chest Radiograph; A Physiologic Approach. Milne and Pistolesi, 1993. 3. Ketai and Godwin, A New View of Pulmonary Edema and Acute Respiratory Distress Syndrome. Journal of Thoracic Imaging 13: 147-171. 1998. 4. UpToDate. Acute Decompensated Heart Failure (Cardiogenic Pulmonary Edema). Accessed 11/02/06. 5. EMedicine “Congestive Heart Failure and Pulmonary Edema” 6. Loyola University teaching website: www.meddean.luc.edu/lumen/MedEd/MEDICINE/PULMONAR/CXR/atlas/pulmonaryedema.htm 7. Sumer’s Radiology website:http://www.sumerdoc.blogspot.com/ 8. Pistolesi M et al. Factors Affecting Regional Pulmonary Blood Flow in Chronic Ischemic Heart Disease. Journal of Thoracic Imaging 3(3): 6572. 1988. 9. Kostuk WJ. Circulation 1973 48: 624. 10. Goodman and Morgan. Pulmonary Edema and adult respiratory distress syndrome. Radiologic Clinics of North America 1991; 29: 943-963.