Cardiovascular System The Heart Chapter 20
advertisement

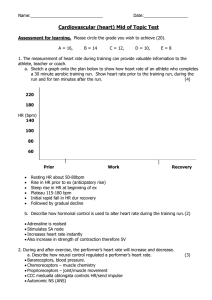
Chapter 20 Cardiovascular System The Heart Heart • Located in the pericardial cavity, which… • is in the mediastinum – a space defined by being between sternum, lungs and spine. • Also found in mediastinum are the thymus and vena cava Pericardial Sac • Protective membrane surrounding heart – 3 divisions… – Fibrous Layer – made up of tough, fibrous connective tissue and irregular dense connective tissue – Parietal Layer – inner border of fibrous pericardium, made up of serous membrane – pericardial space – contains serous fluid (lubrication) – Visceral Layer – internal to parietal surrounds heart itself (Layers of the Serous Pericardium) Heart Wall • Epidardium (visceral pericardium)– includes simple squamous epithelium, loose connective tissue and fat • Myocardium – muscle (much of wall thickness) • Endocardium – a layer of simple squamous epithelium. (This is continuous with the endothelium of blood vessels) • Trabeculae Carnae – raised projections on the inner surface of the heart wall Heart “Skeleton” • Fibrous connective tissue forms supporting structures • rings surrounding heart valves • notice arrangement of muscle attachment to the rings – contraction causes heart to ‘shorten’ apex to base Cardiac Muscle • Branching/Interconnected/multinucleate muscle bundles • ‘cells’ join at specialized sites called intercalated disks – desmosome – mechanical connection (fibrous anchoring takes up strain) – gap junctions – allow ions to flow freely between cells – because of this interconnection heart functions as a syncytium (a fused mass of cells) Conduction System • “Pacemakers” of the heart • SinoAtrial (SA) node – located just toward the midline from the superior vena cava • Internodal pathway • AtrioVentricular (AV) node – medial to the right AV valve • AV Bundle • L/R bundle branches • Purkinje fibers Conducting System Function • SA node pulses causing atria to contract • Internodal pathway slows this signal ‘just a bit’ to allow atria time to complete contraction • Signal reaches AV node causing it to fire an impulse down the… • AV bundle (left & right branches) • Signal reaches heart apex and travels back up walls of ventricles causing them to contract Heartbeat • Coordinating beating of Atria & Ventricles • Heart muscle exhibits autorythmicity – beats on its own • Electrical Conduction System regulates beating for efficiencey • Since cardiac muscle fibers are interconnected (remember intercalated disks?) would eventually all contract. • Two muscle masses – atria & ventricles (syncitia) Cardiac Cycle • Two distinct phases… • Systole – contraction phase • Diastole – relaxation phase Description begins at end of ventricular diastole with relaxed ventricles Cardiac cycle … stepwise • Ventricles are full – AV valves are open, semilunar valves are closed • Ventricles begin to contract – pressure rises • Cuspid (AV) valves will be pushed closed by the pressure wave • brief ‘isometric’ contraction period with no blood leaving • sufficient pressure builds to open semilunar valves • blood leaves left ventricle through aortic arch and right ventricle through pulmonary aorta Cardiac cycle continues • Isometric relaxation of ventricles – no blood leaves • Cuspid valves open and blood flows passibely from atria into ventricles • About 1/3 way through ventricular diastole atria begin to contract (atrial systole) and remaining blood is forced into ventricles. • After Atrial systole, atria relax (diastole) and atria fill passively. Heart Sounds • Lubb – low pitched sound of valves closing • Dupp – higher pitch sound of aortic and pulmonary valves closing • Slush – (especially audible in thinner people) – blood flowing turbulently into ventricles Contraction • AP arrives – T-Tubules (transverse tubules) carry signal from surface of cell to sarcoplasmic reticulum • Loose association between SR and T-tubules results in slow onset of contraction with prolonged contraction phase… • Na+ rushes in via t-tubules to SR causing Ca++ to be expelled from SR stores Contraction continued • Ca++ proceeds to sarcoplasm (cytoplasm) where it binds to troponin • troponin changes shape and moves tropmyosin off receptor sites… excitation occurs • This portion is referred to as Rising Phase • A second type of Ca++ channel opens in SR and Ca++ pump turns off The End.