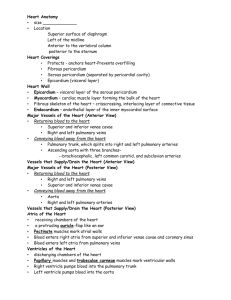
Physiology Lecture Outline: Cardiovascular Physiology The Cardiovascular System In simplest terms, the cardiovascular system consists of a central pump (the heart) and a series of tubes (blood vessels) connected to this pump which pushes fluid (blood) through these tubes. It's primary function is the transportation of these materials between all parts of the body and the heart. These materials include nutrients, water, waste, signal molecules, immune cells and gases (O2 and CO2). The Heart The heart is a muscular organ that lies in the center (left) of the thoracic cavity. It is composed mostly of myocardium (cardiac muscle) and is enclosed in the pericardial sac. The heart has four chambers, divided into left and right halves. Each half contains an upper chamber, the atrium (for receiving blood) and a lower chamber, the ventricle (for pumping blood). One-way flow in the heart is ensured by 4 heart valves: 1) the right (tricuspid) atrioventricular (AV) valve. 2) the left (bicuspid/mitral) atrioventricular (AV) valve. 3) the pulmonary semilunar valve in between the right ventricle and the pulmonary trunk. 4) the aortic semilunar valve in between the left ventricle and the aorta. The pulmonary trunk leaves the right ventricle and aorta leaves the left ventricle. Blood between the two sides do not mix. Each of the sides contract together in a coordinated fashion, first both of the atria contract, this is then followed by both of the ventricles contracting. Arteries - are vessels that carry blood away from the heart. Veins - are vessels that carry blood toward the heart. A ring of fibrous connective tissue (called the fibroskeleton) surround the openings between the top and bottom chambers. The fibroskeleton has several functions: 1. Provides a site of attachment for AV valves and helps keep theses openings patent during contraction. 2. Maintains integrity of the shape of the heart when ventricles contract, while allowing the apex and the base to be pulled together 3. It electrically separates (insulates) the atria from the ventricles, thus guarding against the spread of electrical signals that are not through the intrinsic electrical conduction system (discussed later). The Heart Functions as a Dual Pump: The Circuits of the Heart Within the cardiovascular system there are two circuits or circulations - the pulmonary and systemic. Pulmonary Circulation - Pumps blood to and from the Lungs. Often termed the "right side" of the heart. This circuit can also be thought of as starting at the R ventricle and ending at the L atrium. Systemic Circulation - Pumps blood to and from the body. Often termed the "left side" of the heart. This circuit can also be thought of as starting at the L ventricle and ending at the R atrium. Volumes and Pressures of the Dual Pump The cardiovascular system is a closed circulatory system, and for that to exist, the volume of blood in both sides of the pump must be equal. The pressures of the fluid in either side of the heart, however, are very different. The proximity of the lungs to the heart (about 4 inches) means that the right pump (R ventricle) does not have to work very hard to move the blood to the lung tissue. The minimum pressure required from the pulmonary circuit is normally about 25 mmHg. 2 The systemic circuit, however, is much more involved and the left pump (L ventricle) needs to work very hard to move the blood to every part of the body. The minimum pressure required from the systemic circuit is normally about 80 mmHg. Therefore, the pressure generated by the left side of the heart is over three times greater than that generated by the right side. As a consequence, the muscular wall of the left ventricle is about three times thicker than the right ventricle. CARDIAC MUSCLE AND THE HEART There are two types of cardiac muscle cells (myocardiocytes) in the heart: 1) autorhythmic myocardiocytes and 2) contractile myocardiocytes. About 1% of myocardial cells are autorhythmic and they spontaneously generate action potentials (APs) without nervous stimulation. In this way, control of heart rate is considered intrinsic myogenic control - that is, derived from within the heart muscle itself. In contrast, skeletal muscle is neurogenic - that is, it requires stimulation by the nervous system to initiate contraction. In cardiac muscle, input from autonomic neurons and hormones can modify the contraction rate set by the pacemaker cells and modifies the force of contraction. However, the heart will contract in the absence of all neural input. Autorhythmic cells are anatomically distinct from contractile myocardiocytes. They are smaller, have few contractile fibers, organelles and contain no organized sarcomeres - so they don't contribute to force generation. About 99% of cardiac muscle cells are contractile myocardiocytes. These cells are striated, have organized sarcomeres and have high energy demands, 1/3 of cell volume is mitochondria. A characteristic of cardiac muscle are that they contain intercalated disks, which are interdigitated membranes joined by desmosomes and gap junctions. The desmosomes are a type of cell attachment, so that adjacent cells are physically attached to each other to cope with the stressful mechanical activity of the heart. Gap junctions are simply protein channels connecting adjacent myocardiocytes, they allow ions to pass though and thus waves of depolarization to spread throughout the muscle tissue - creating nearly simultaneous contraction. Excitation-Contraction Coupling in Cardiac Muscle is Similar to Skeletal Muscle Contraction occurs by the same sliding filament activity as in skeletal muscle. However, an important difference is that the AP opens membrane voltage-gated Ca2+ channels for extracellular Ca2+ entry. This entry of Ca2+ from the ECF is required for cardiac muscle contraction. Ca2+- Induced Ca2+ Release In cardiac muscle, about 90% of the Ca2+ used in contraction is stored in the SR, and about 10% comes from the ECF. The influx of Ca2+ from the ECF triggers release of SR Ca2+ stores, without the ECF Ca2+, no Ca2+ would be released from the SR. The Ca2+ diffuses through cytosol to contractile elements and bind troponin allowing crossbridge cycling and contraction. Ca2+ removal requires Ca2+-ATPase (SR). Ca2+ removal also achieved by Na+- Ca2+ indirect active transporter (ECF). In Cardiac Muscle, Contraction can be Graded A single muscle fiber can execute graded contractions, so that the fiber varies the amount of force it generates. Graded contractions in skeletal muscle occur through motor unit recruitment (spatial summation) or with increased firing frequency of the somatic motor neuron (temporal summation). However, the force generated in cardiac muscle depends on the number of cross bridges formed. When cytosolic [Ca 2+] is low, fewer crossbridges activated, giving a weaker force of contraction. If cytosolic [Ca2+] is increased, more crossbridges formed giving additional force generated. Thus, the strength of myocardial contraction is 3 2+ 2+ directly related to the amount of Ca present in the cytosol. The more Ca free inside the cell the, the stronger the contraction. The cytosolic concentration of Ca2+ can be increased two ways: 1) by increasing the amount of Ca2+ that enters the cell through voltage-gated calcium channels. 2) by storing more Ca2+ in the sarcoplasmic reticulum. Catecholamines and Electrical Activity Norepinephrine (NE) and epinephrine (E) are Catecholamines. These catecholamines regulate the amount of Ca2+ available for cardiac muscle contraction. E and NE bind 1 (beta-l) receptors on cardiac muscle membrane to increase force of contraction. NE and E increase the open probability of Ca2+ channels in the myocardial contractile cell, but at the same time they also increase the K+ permeability, enhancing outward K+ flow and terminating the plateau. Thus, E and NE increase Ca2+ entry and enhance intracellular sarcoplasmic reticulum stores of Ca2+ without increasing the duration of the contraction. Functionally, this makes sense. Since E and NE also increase heart rate, it would be counterproductive to lengthen the time of cardiac contraction. NE and E also activate second messenger systems in myocardiocytes and trigger signal transduction which causes phosphorylation of proteins inside the cell, including Ca2+ channels. Phosphorylated voltage-gated Ca2+ channels increase the probability of them opening, this allows more Ca2+ to enter cell. Phospholamban is a regulatory protein on the SR and helps to concentrate Ca2+ in the SR. Stimulation of NE receptors (1) triggers phosphorylation of phospholamban, which then enhances the Ca2+-ATPase activity on the SR. This means that more Ca2+ can be stored in the SR and more quickly. The net result is a stronger contraction and a shorter duration of cardiac contraction (heart beats faster). Another property of cardiac muscle is that when it is stretched, it contracts more forcefully. This is due to the length-tension relationship that we have already seen in skeletal muscle. The degree of overlap between thick and thin filaments will effect the tension generated by that muscle cell. Stretching myocardial cells also allows more Ca2+ entry, this also leads to a stronger contraction. The degree of stretch of myocardiocytes at any one time depends on blood volume in the chambers when filling is occurring. Action Potentials in Myocardial Cells Contractile cells and autorhythmic cells show distinctive AP generation. Ca2+ is important in the AP, in contrast to skeletal muscle and neurons. Myocardial Contractile Cells Stable resting membrane potential (-90 mV). Action potentials similar to those of skeletal muscles and neurons. Rapid depolarization is due to Na+ entry and repolarization due to K+ efflux. A unique feature of APs in myocardial contractile cells is the absence of a hyperpolarization phase at the end. The myocardial cell returns directly to its stable resting membrane potential of -90 mV (the equilibrium potential for potassium). Because efflux and influx are exactly balanced at -90 mV, there is no driving force to cause K+ to leave the cell and hyperpolarize it. The myocardiocyte AP is lengthened compared to skeletal muscle AP, due to Ca2+ entry creating the elongated plateau phase before repolarzation. Typical skeletal muscle AP duration is 1-5 msec but for contractile myocardial cells AP duration is about 250 msec. Most of this AP is in the absolute refractory period and this helps to prevent tetanus and allows chambers to fill. 4 K+ Channels in Contractile Myocardioicytes There are multiple forms of K+ channel in myocardial cells, each with different properties. There are 3 channels involved in the contractile cell action potential. 1) iKl channel (inward rectifier): This channel is open during the resting phase. They are voltage-sensitive and begin to close when the cell depolarizes, but they are slow and do not actually close until the beginning of the plateau phase. 2) ito channel (transient outward rectifier): This channel opens at the end of depolarization and closes very rapidly. K+ efflux through this channel is the reason for the quick drop in membrane potential just before the plateau. 3) iK channel (delayed outward rectifier): This channel open at the end of the plateau and is responsible for the repolarization phase. They are activated by the depolarization but are slow to react. Autorhythmic Myocardiocytes Pacemaker ability results from unstable membrane potential. It starts at -60 mV and drifts upward, this can be called a pacemaker potential. When it reaches threshold (-40mV), the cell fires an AP. The membrane potential instability is caused by "funny" (If ) cation channels that allow Na+ and K+ permeability at -60 mV, this channel allows more Na+ in than K+ out and induces current flow and the drifting membrane. Open If channels creates net influx of positive charge, depolarizing autorhythmic cells. Depolarization then closes If channels and opens Ca2+ channels. At threshold, many Ca2+ channels open, thus creating Ca2+ influx and rapid depolarization. Repolarization is due to K+ efflux through open K+ channels. The timing of APs in these cells can be influenced by norepinephrine and epinephrine. These stimulate 1 receptors and increase ion flow in If and Ca2+ channels. This then increases the rate of depolarization, which increases heart rate. ACh acts on muscarinic receptors (as part of the parasympathetic division of ANS) to slow heart rate by altering K+ and Ca2+ permeability. Electrical Conduction System The electrical conduction system in the heart coordinates contraction. The APs originates in one part of the strategically located autorhythmic cells and then spreads this signal between cells via gap junctions in intercalated disks. The depolarization of muscle cells is followed by a wave of muscle contraction that passes across the atria then moves into the ventricles. The electrical conduction system consists of five major sites: 1) sinoatrial (SA) node node; 2) atrioventricular (AV) node; 3) AV Bundle (of His); 4) right and left bundle branches; and 5) Purkinje fibers. The sinoatrial (SA) node, in the superior, posterior portion of the right atrium, initiates contraction of the heart because it fires APs at the highest rate (see table below). For this reason, it is called the pacemaker of heart. The internodal pathway connects SA node to atrioventricular (AV) node, located in the floor of right atrium. This connects to the AV Bundle (of His) located in the IV septum. This then splits into right and left bundle branches running down the IV septum and finally into Purkinje fibers at the apex of the heart. Due to the electrical insulation of the fibroskeleton, the direction of the AP is controlled and results in apex-to-base contraction of ventricles. Thus, blood is squeezed out of the ventricles from the bottom to the top of the chambers. Blood ejection is also aided by the spiral arrangement of muscles in the walls. The slow conduction of the electrical signal through AV node cells lengthens their refractory period, this helps to create the AV nodal delay and allows the atria to complete their contraction before ventricular contraction begins. If the SA pacemakers malfunction and fire at a very rapid rate, AV nodal delay prevents every action potential from passing into the ventricles, in this way permitting the ventricles to function at a slower pace so that they have time to fill with blood. The SA node sets the heart rate because it fires APs at 5 the fastest rate and the other regions follow the lead of the SA node. If the SA node is damaged, then another pacemaker sets the heart rate. Table 1. The rate of action potentials/min for the autorhythmic myocardiocytes. These are average values for a intact heart inside a healthy individual at rest. Electrical Conduction Spontaneous Rate of Region Action Potentials/minutes SA Node 70-80 AV Node ----AV Bundle 40-60 R and L Bundle Branches ----Purkinje Fibers 20-40 The Electrocardiogram Reflects the Electrical Activity of the Heart The Electrocardiogram (ECG or EKG) is a recording of the electrical activity of the heart, detected by recording electrodes placed on the skin. Because the ventricles have more muscle than the atria, they create a larger electrical signal so the waves associated with the ventricles are usually larger than the waves associated with the atria. An ECG is not a single action potential, but shows the sum of all the electrical potentials generated by all heart cells at any moment. Some basic definitions for an EKG trace: Segment – a straight line. Wave – a deflection from the straight line (0 milivolts). Interval – a segment and a wave. Complex – a series of waves. The Main Components of an ECG P wave: Depolarization in the atria. QRS complex: Depolarization of ventricles (and atrial repolarization, typically masked on the ECG). T wave: Repolarization of the ventricles. PQ or PR interval: Represents AV nodal delay. T-P segment: Ventricular diastole (filling). In Lab we perform EKGs on fellow students using the Vernier Lab pro computer program. No two EKGs will be identical or exactly like a “normal” example but there are fundamental properties that are shared amongst all “normal” EKG traces. In the lab manual, there is a normal trace, indicating the typical orientation (up or down), amplitude (height) and duration (time interval) of the segments, interval, wave and complexes. Mechanical events lag slightly behind their electrical signals. Atrial contraction begins really as the P wave ends and continues during P-R segment. Ventricular contraction begins just after Q wave and continues through S-T segment. Common terms include: tachycardia - fast heart rate (above 100); bradycardia - slow heart rate (below 60). At very rapid heart rates, there may be less blood pumped per beat because the muscle has not had time to relax completely, but remember, the longer refractory period of myocardial cells prevents tetanus! Tetanus would not allow the heart to relax at all. In that state, no blood would be pumped to the brain and the rest of the body. Arrhythmias can result from benign extra beats or more serious conditions discussed in lab. THE CARDIAC CYCLE 6 The cardiac cycle is the period of time from the beginning of one heartbeat to the beginning of the next. There are two main stages: Diastole - the time during which cardiac muscle relaxes and Systole - the time during which cardiac muscle is contracting. Atria and ventricles do not contract at same time, but each side of the heart contracts at the same time. For convenience, the cardiac cycle can be divided into 5 stages. Atrial and Ventricular Diastole: The Heart at Rest The heart is at rest and the atria and ventricles are relaxing. The atria are filling with venous blood. The AV valves open as ventricles relax and blood flows by gravity from atria to ventricles. During this phase, the ventricles are about 80% of filled with blood, this is termed passive filling. Atrial Systole: Completion of Ventricular Filling When the atria contract (systole), the remaining 20% of blood fills the ventricles, this is like a "topping off" of the ventricles. Atrial systole begins following depolarization of the SA node, as a wave of depolarization (electrical signal) across the atria is followed by a wave of contraction that pushes blood into the ventricles to complete ventricular filling. Some blood is forced back into veins, creating a small retrograde blood movement, measured as a pulse in the jugular vein. At this time, just prior to ventricular systole (the next stage), the ventricles are full of blood, this is termed End Diastolic Volume (EDV) and represents the maximum ventricular volume. At rest in a 70 Kg male, this value is typically 135ml in each ventricle. Clinical Note: Because most of ventricular filling occurs passively, pathologies in which atrial contraction is disturbed may have very little effect on overall cardiovascular function. It is not uncommon for people with atrial fibrillation to have few symptoms. Early Ventricular Systole (part one) and the First Heart Sound Ventricular systole begins at the apex of the heart as spiral bands of muscle squeeze blood upward toward the base. The increasing pressure of the blood in the ventricles forces the AV valves closed - creating the first heart sound, the "lub" of "lub dub". Both ventricles are now 'sealed' compartments in that the AV and semilunar valves are closed. The ventricles are continuing to contract, but if all valves are closed, the blood goes nowhere. The heart is in Isovolumic Ventricular Contraction. This occurs when the blood volume inside the ventricles remains the same (prefix iso- means 'same'), but pressure is increasing. During this phase, the atria repolarize and relax as the ventricles continue to contract. Ventricular Systole (part two): Ventricular Ejection When ventricular contraction generates enough pressure it opens the semilunar valves, and blood enters arteries (RV => pulmonary trunk/artery, LV => aorta). The high-pressure blood is forced into the arteries (ejection of blood from ventricles), which displaces lower-pressure blood, creating blood movement. Remember that each ventricle has equivalent blood volumes but different pressures. The RV requires a min of 25 mmHg and the LV requires a min of 80 mmHg to open the semilunar valves. At these respective pressures, the pressure gradient which drives blood flow is established. At this time, just after ventricular systole, the ventricles have just ejected blood but the ventricles do not empty. In fact, at rest they only eject about half of the blood volume in the ventricle. The blood volume remaining in the ventricles after ejection is termed End Systolic Volume (ESV). A typical value for a 70 Kg male at rest is about 65ml per ventricle that remains in the heart after ejection. We can calculate how much blood left the heart (called Stroke Volume) if we know the maximum volume, EDV, and subtract the volume remaining after contraction, ESV. This means that about 70ml of blood is ejected per beat. See calculation below from this formula: Stroke Volume (SV) = EDV - ESV Ventricular Diastole and the Second Heart Sound 7 As the ventricles relax, the pressure of the blood inside decreases. The blood in the large arteries leaving the ventricles falls back toward the heart as the driving force subsides. This reversal of blood toward the heart fills the cusps of the semilunar valves, slamming them closing them - creating the second heart sound, "dub" of "lub dub". The AV valves remain closed because ventricular pressure is still greater than the atrial pressure. As the ventricles relax, the pressure of the blood inside decreases and once the semilunar valves close, the compartment is again 'sealed'. Now the ventricles are undergoing Isovolumetric Ventricular Relaxation. This is a state where pressure is decreasing but volume remains constant. When ventricular pressure becomes less than atrial pressure, the weight of the blood in the atria opens the AV valves (like a trap door) and blood moves into ventricles. The cardiac cycle is now complete because it is at the filling stage again, where we started. Disorders of Heart Valves Valvular Stenosis refers to a narrowing of the opening of the valves, often associated with stiffness of the valve. In cases such as AV valve stenosis, atrial systole becomes significant. The atria must contract more forcefully to get the blood through a narrower opening into the ventricle. This causes turbulent blood flow which can be detected as sound, commonly referred to as a heart murmur. This reduces the heart's efficiency and thus increases its work load. Valvular Prolapse - occurs when there is incomplete closure of the AV valves, allowing retrograde flow of blood. These are often called incompetent or insufficient valves. It is an inherited weakness of the chordae tendineae (the 'cords' that attach to the 'flaps' of the AV valve) so that during ventricular sytole, there is sum back flow into the atria. Typically is makes a click followed by a swish sound when blood leaks back into atria. These murmurs can range from harmless to severe. Most valvular disorders commonly occur on the left side of the heart because these valves are subjected to greater forces during contraction of the powerful left ventricle. For instance, mitral valve prolapse is the most common valvular disorder. Heart Rate is Modified by Autonomic Neurons and Catecholamines The rhythm and rate of the heart is initiated by SA node, but modulated by neural and hormonal input. In a normal adult heart, the resting rate of the SA node is about 70 action potentials (APs) per minute, this translates to a heart rate of about 70 bpm. The parasympathetic and sympathetic branches of the ANS exert antagonistic control over heart rate. Parasympathetic activity slows heart rate and Sympathetic activity increases heart rate and force of contraction. If the heart were separated from ANS innervation, the intrinsic rate of the SA node would actually be about 90-100 APs per minute, but inside the body it is brought down to about 70 by parasympathetic modulation via the vagus nerve. The parasympathetic division releases ACh from the vagus nerve on to muscarinic receptors at autorhythmic cells of the SA and AV nodes to decrease heart rate, by increasing K+ efflux. The sympathetic division releases NE and E on 1 receptors to increases heart rate (via AV node conduction). This can elevate heart rate up to 120 bpm and greater. Stroke Volume is the Volume of Blood Pumped by One Ventricle in One Contraction Stroke volume (ml/beat) = Amount of blood pumped by one ventricle during a single contraction. It is calculated as: Stroke Volume (SV) = EDV - ESV For example, if we use the values given in the cardiac cycle describe above, we can calculate SV. If EDV = 135ml and ESV = 65ml, then SV = EDV - ESV; => 135ml - 65ml = 70ml/beat (per beat). Stroke volume isn't constant, it is homeostatically regulated. It can decrease when you are at rest and increase greatly during exercise. Multiple Factors Influence Stroke Volume 8 Stroke volume is directly related to the force generated by cardiac muscle during contraction. Greater force means greater stroke volume. The force is affected by 2 parameters, 1) the length of muscle fiber at beginning of contraction and 2) the contractility of the heart. Contractility is the intrinsic ability of cardiac muscle fiber to contract at any given fiber length. Length-Tension Relationships and Starling's Law of the Heart As the sarcomere length in cardiac muscle increases, the tension generated by the contracting muscle increases. This leads to increases in stroke volume, as the more forceful the contraction, the greater amount of blood can be ejected. As additional blood flows into ventricles, this causes muscle fibers to stretch, lengthening the fibers and hence increasing the force of contraction. Stretch and force are related by the Frank-Starling law of the heart: Stretch (sarcomere length) is proportional to EDV. Force is proportional to stroke volume. Stroke Volume and Venous Return The heart contracts more forcefully as additional blood enters the heart. The blood that returns to the heart from the venous circulation is termed 'venous return' and the greater the venous return, the more forceful the heart will pump. Venous return determines EDV and this determines stroke. The Pre-load stretch is the degree of myocardial stretch created by venous return. Several factors affecting venous return, such as the skeletal muscle contractions (skeletal muscle pump), this squeezes low pressure veins and push blood toward heart. The Respiratory pump is also a factor in venous return. It is created by the movement of thorax during respiration. Increases in pressure in abdominal veins, flow 'down' into the decreased pressure in thoracic veins. The result is that the lower thoracic pressure draws more blood in from the abdominal veins. Also, the constriction of veins via sympathetic activity has an important impact on moving more blood into heart. Sympathetic innervation of veins allows also allows for redistribution of venous blood to the arterial side of the cardiovascular circulation. Cardiac Output is a Measure of Cardiac Performance Cardiac output (CO) is an indicator of total blood flow through the circulation. It doesn't describe blood distribution among tissues. CO (L/min) = Amount of blood pumped per ventricle per unit time. It is calculated as: CO = Heart Rate (HR) x Stroke Volume (SV) At rest in a 70 Kg man, CO is about 5 L/min (average). Normally, both sides have equal CO. If for some reason CO's become unequal, blood will pool behind the weaker side of the heart. Blood Flow through the Cardiovascular System Pressure, Volume, Flow and Resistance Liquids and gases flow from areas of higher pressure to areas of lower pressure - that is to say, they flow down their pressure gradients. The high pressure generated when the ventricles contract forces blood to flow into vessels that exist at lower pressure. The pressure of the fluid (blood pressure) continues to fall as blood moves away from the heart. The vessels with the highest pressure are the aorta and other large systemic arteries. The vessels with lowest pressures are the veins the superior and inferior venae cavae. Compressing a Fluid Raises its Pressure The Hydrostatic Pressure (HP) of blood falls over distance as energy is lost to friction. Ventricular contraction attempts to decrease volume of the ventricle as the pressure is increased. Driving Pressure - is created within the ventricles to drive blood through the vessels. As the heart chambers relax, pressure falls and allows blood to flow in (thus volume increases). Blood vessel volume can also change. In the body, when vasodilation (increase in blood vessel diameter) occurs this results in increased 9 blood volume and decreased pressure. When vasoconstriction (decrease in blood vessel diameter) occurs, this results in decreased blood volume and increased pressure. For the heart, the term systole means contraction and also implies ejection of blood. The term diastole means relaxation and indicates that filling of blood is occurring. Blood Flows Down its Pressure Gradient Blood flows from an area of higher pressure to one of lower pressure. Differences in pressure between 2 ends of a tube creates a pressure gradient (P). P2 P1 Flow P Fluid flow depends on the change in pressure; P1 - P2 = P. The greater the pressure gradient, the greater the driving force for fluid flow. The Pressure Gradient is the driving force for blood flow. Resistance Opposes Flow Blood flowing through blood vessels encounters friction from the vessel walls and the components of blood colliding with each other. The term Resistance (R) refers to the tendency of the cardiovascular system to oppose blood flow. Increased resistance leads to decreased flow. Thus, Flow 1/R ( = proportional to). There are three parameters that contribute to resistance to flow of fluid through tube: 1. Tube Length (L) - as the tube lengthens, resistance increases. In the body, length is determined by the anatomy of the vascular system and this remains fairly constant. 2. Fluid Viscosity () - describes the 'thickness' of a fluid. The viscosity of blood is about 5-6 times greater than water (due to blood cells and plasma proteins). The more viscous the fluid the greater the resistance to flow. The viscosity of blood in the body is normally maintained to remain constant. 3. Tube Radius (r) - the radius can be simplified to mean the diameter of the tube. As the radius of the tube decreases, the resistance to flow increases; conversely, as the radius of the tube increases, the resistance to flow decreases. This parameter does not remain constant in the body - the diameter of blood vessels change continuously - thus, the radius of blood vessels is the main determinant of resistance to blood flow in the body. The relationship between these parameters and flow of a fluid through a tube can be expresses by: Poiseuille's law: R = 8 L/r4 However, in humans this can be simplified to: R 1/r4 as blood vessel radius becomes the main determinant. Vasoconstriction leads to increased resistance and decreased flow. Vasodilation leads to decreased resistance and increased flow. Therefore, blood flow is described by this formula: Flow P R OR P 1/r4 If the driving force remains constant, flow varies inversely with resistance (determined by radius).