Cardiovascular assessment
advertisement

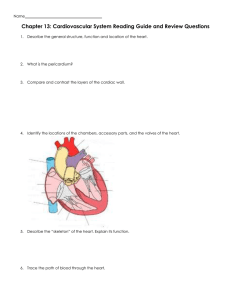
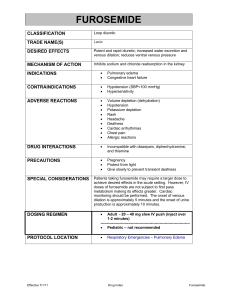
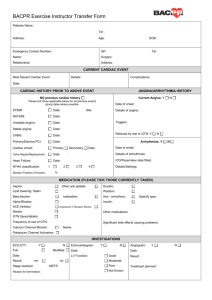
CARDIAC ASSESSMENT Cardiovascular Assessment 1. 2. 3. 4. The medical chart review; Patient/family interview; Physical assessment, Precautions and contraindications 1. MEDICAL CHART REVIEW 1. Diagnosis and date of event 2. Symptoms on admission and after the patient’s admission 3. Other significant medical problems in the past medical history 6. Relevant social history, including smoking, alcohol and drug 7. Oxygen therapy and other respiratory treatment 8. Clinical laboratory data 4. Current medications 9. Radiological studies 5. Risk factor for cardio\vascular and pulmonary 10. Surgical procedures MEDICAL CHART REVIEW Other therapeutic regimens Other diagnostic tests Electrocardiogram and Vital signs telemetry monitoring Pulmonary function test Arterial blood gases cardiac catheterization data Hospital course since admission. Occupational history Home environmental assessment 2. Patient/family interview • establishing relation with the patient and family, • discerning their level of understanding of the medical problem(s), and • their goals and expectations for rehabilitation. Typically, interview questions should be open ended and straightforward. For example • What prompted you to come to the hospital/seek physical therapy? • Do you ever have problems with shortness of breath, chest pain or discomfort, lightheadedness or dizziness, getting tired easily, palpitations, etc.? • Do you experience any type of discomfort or pain with exertion? If it occurs during ambulation, at what distance, speed, or incline? What about stairs? • Can you describe your symptoms for me? • What brings on your symptoms? What kinds of things are you doing immediately before or at the time of the onset of your symptoms? • Are your symptoms aggravated by certain positions, such as lying flat or on one side or the other? • How long have you had these symptoms? • Do the symptoms interfere with things you would like to do? Such as? • Have you discovered any ways to relieve the symptoms? • What has your doctor told you about your problem? • Have you ever received physical therapy for this problem or any other problem? • Have you ever smoked? How much and for how long? • What would you say your major difficulty is right now? • What would you like us to work on before you go home? • What are your goals for your recovery? 3. Physical examination 1) Examine pulse 2) Examine heart sound 3) Examine heart rhythm 4) Blood pressure 5) Rate and depth of respiration 6) Oxygen saturation 7) Examine pain 3. Physical examination • General appearance Obesity, cachexia, barrel-shaped chest, signs of breathing difficulty (e.g., tachypnea, use of accessory muscles of respiration, intercostal retractions) • Vital signs increase or decrease heart rate, blood pressure, or respiratory rate; presence of fever • Skin Cold and clammy in low-cardiac output states; pale, blue, and cold if peripheral vasoconstriction; • Cyanosis (peripheral or central) if marked arterial hypoxemia; or xanthomas in familial hypercholesterolemia • Head, eyes, ears, nose, and throat (HEENT) • Abnormal funduscopic eye examination (e.g., retinal arteriolar changes in hypertension HTN and DM) • Abnormal neck examination (e.g., jugular venous distension in right or biventricular heart failure, exaggerated venous pulse waves in pulmonary HTN or right-sided valvular disease, or prominent carotid pulsations in aortic incompetence) • Signs of upper respiratory infection (which might be seeding lower respiratory tract) • Chest, lungs Abnormal chest examination (e.g., decrease chest or diaphragmatic excursions in chronic obstructive pulmonary disease, prominent pulsations in cardiac hypertrophy, thrills in valve disease) • Abnormal breath sounds (e.g., decreased, bronchial, or adventitious breath sounds • Cardiovascular Abnormal heart sounds (e.g., murmurs in valvular disease, third and/or fourth heart sounds • if diastolic dysfunction or reduced ventricular compliance, friction rubs in pericarditis • Abnormal peripheral pulses (e.g., decreased if atherosclerotic disease or aortic stenosis, bounding in aortic incompetence) • Abdomen Enlarged liver and spleen, ascites in right heart failure • Extremities Abnormal digital clubbing) extremity examination (e.g., peripheral edema, Sign or Symptom of Cardiovascular diseases • Chest pain or discomfort due to mismatch between myocardial oxygen supply and demand (due to coronary disease, LV hypertrophy, LV outflow obstruction, coronary spasm, microvascular angina), autonomic dysfunction, MV prolapse • Claudication due to peripheral arterial disease with mismatch between peripheral O2 supply and demand • Clubbing of digits due to right-to-left shunting in congenital heart disease • Cough due to acute pulmonary edema, MS • Cyanosis due to right-to-left shunting in congenital heart disease, significant decrease cardiac output • Dizziness due to inadequate cardiac output resulting in # perfusion of the brain (due to LV dysfunction, LV outlet obstruction, arrhythmias, blood pooling in lower extremities) • Dyspnea due to pulmonary venous pressure caused by LV diastolic or systolic dysfunction (due to coronary ischemia, hypertension, valvular disease, cardiomyopathy), peripheral arterial disease with lactic acidosis • Edema due to " Systemic venous pressure due to " RA pressure (e.g., LV failure, MS, cor pulmonale, TS, TR, constrictive pericarditis) • Fatigue due to low cardiac output (due to LV dysfunction, LV outlet obstruction, arrhythmias), drugs • Hemoptysis due to acute pulmonary edema, MS • Hypotension due to decrease cardiac output, vasodilation • Jugular venous distension due to increase systemic venous pressure caused by increase RA pressure (see preceding entry for Edema) • Nocturia due to CHF with peripheral edema • Orthopnea In CHF, SOB when lying flat due to increase pulmonary venous pressure caused by increase venous return to heart, which is not able to handle increase workload • Palpitations due to arrhythmias • Paroxysmal nocturnal dyspnea In CHF, sudden onset of SOB that awakens patient at night because of " pulmonary pressures caused by the gradual reabsorption of edema fluid from the LEs (which are no longer dependent), resulting in " venous return to heart, which is not able to handle " workload Functional Classification of Heart Disease Functional Classification, Exercise Tolerance, Description Approximate I (6 –10 METs) Patient with cardiac disease but without any resulting limitations of physical activity; ordinary physical activity does not cause undue fatigue, palpitations, dyspnea, or anginal pain II (4–6 METs) Slight limitations of physical activity; comfortable at rest, but ordinary physical activity results in fatigue, palpitations, dyspnea, or anginal pain III (2–3 METs) Marked limitation of physical activity; comfortable at rest, but less than ordinary physical activity causes symptoms, as above IV (<2 METs) Unable to carry out any physical activity without discomfort; symptoms of cardiac insufficiency or of angina may be present even at rest; if exertion is undertaken, discomfort increase Absolute Contraindications 1. Unstable or rest angina 2. A recent significant change in the resting ECG suggesting significant ischemia or recent MI 3. Dangerous arrhythmias causing symptoms of hemodynamic changes 4. Symptomatic CHF/pulmonary edema 5. Suspected or known dissecting aneurysm 6. Severe aortic stenosis Absolute Contraindications • Acute pulmonary embolus or pulmonary infarction • Uncontrolled diabetes mellitus • Uncontrolled HTN: Resting SBP >200 mm Hg and/or resting DBP >110 mm Hg • Persistent hypotension after MI (SBP <90 mm Hg) • Acute systemic infection, accompanied by fever, body aches, or swollen lymph glands • Acute pericarditis or myocarditis High-risk level • Severely depressed LV function • Presence of angina or other significant symptoms at low levels of exertion (<5 METs) or during recovery • Presence of abnormal physiological responses with exercise testing • High level of silent myocardial ischemia • History of complex ventricular arrhythmias at rest or appearing or increasing with exercise • History of cardiac arrest or sudden cardiac death • Complicated or high-risk MI or revascularization procedure • (e.g., anterior infarction, large infarct size, infarct extension, congestive heart failure [CHF], cardiogenic shock, and/or complex ventricular arrhythmias) • Presence of congestive heart failure Low-risk level • Individuals with a history of a cardiac abnormality • Presence of normal physiological responses and functional status of at least 7 METs (metabolic equivalents for energy expenditure) on exercise testing • No history of myocardial ischemia or other significant symptoms of exercise intolerance (unusual shortness of breath, lightheadedness, or dizziness) during exercise testing and recovery • No history of resting or exercise-induced complex arrhythmias • No history of congestive heart failure • Status/post uncomplicated MI or revascularization procedure • Absence of clinical depression Intermediate-risk level • Mildly to moderately depressed LV function • Presence of angina or other significant symptoms of exercise intolerance only at high levels of exertion (less than 7 METs) • Mild to moderate level of silent ischemia during exercise testing or recovery (<2-mm ST-segment depression from baseline) • Functional capacity less than 5 or 6 METs on graded exercise test 3 or more weeks after MI. • Failure to comply with exercise intensity prescription. Cardiovascular Diagnostic Tests and Procedures 1) Arterial blood gases (ABGs) • Is oxygenation normal (Pao2 >80 with O2 saturation [SaO2] >97%) or adequate (PaO2 >60 with SaO2 >90%)? If SaO2 <85%, exercise is usually contraindicated. • Are PaCO2 and pH within normal limits (35–45 mm Hg and 7.35– 7.45, respectively)? • Are alterations acute or chronic ? • Was the patient receiving supplemental oxygen when the ABGs were drawn? • Does the patient need oxygen during treatment? 2)Cardiac catheterization Are the chamber and vessel pressures normal? Are there any gradients across the valves? 3) Ventriculography Is ventricular performance normal (EF >40%–50%, normal wall motion)? Is there evidence of valvular regurgitation? 4) Angiography Are there any obstructions in the coronary arteries? If so, how many, in which vessels, and to what degree? Are coronary artery bypass grafts patent?