TENS
advertisement

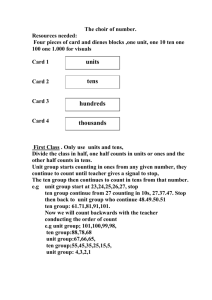
TRANCUTANEOUS ELECTRICAL NERVE STIMULATION -TENS RHPT 353 – 1435-1436-1ST SEMESTER Lecture outlines 2 This lecture deals about transcutaneous electrical nerve stimulation (TENS) in following categories; Physiology of pain Basic terminologies & Definition of TENS Physiological & therapeutic effects of TENS Indications & Contra indication of TENS Technique of application of TENS 353 RHPT TENS 26/09/1437 Lecture objectives 3 At the end of lecture the student is able to Define and outline the principle of TENS. List the physiological effects, therapeutic effects, indication, & contraindication of TENS Select the appropriate TENS dose Demonstrate & apply TENS on her/ his colleague 353 RHPT TENS 26/09/1437 PHYSIOLOGY OF PAIN 4 Definition of pain: Pain is an unpleasant sensory and emotional experience associated with tissue damage. It is a protective mechanism that warns us that there is something wrong and can provoke body response to avoid further injury. 353 RHPT TENS 26/09/1437 PHYSIOLOGY OF PAIN 5 Pain Process The pain process started whenever there is tissue damage which stimulate the nociceptors Nociceptors They are receptors responsible for the reduction and transmission of pain impulses. They are free nerve endings that are widely distributed throughout the body and stimulated with noxious intense stimulus damaging the tissue as intense heat, cold, strong mechanical deformation and chemical substances. 353 RHPT TENS 26/09/1437 Types of Pain 6 Acute pain - It is pain of sudden welldefined onset and associated with tissue damage. - It is usually accompanied by signs of hyperactivity in the autonomic nervous system. - Signs & symptoms of inflammation are very strongly perceived – leads to very intense pain Referred Pain Chronic Pain - It is pain extending beyond the - Pain originating in deep normal course of injury or illness. structures and viscera - It is usually lasting 6 months or which is perceived in some more. superficial sites as skin. - Chronic pain produces significant - The actual damage changes in personality, life style, occur in area and pain is and functional ability. felt in other remote area. - The signs & symptoms of inflammation is very less – leads to mild pain in certain activities. 353 RHPT TENS 26/09/1437 TYPES OF NERVE FIBERS 7 The nervous system responds promptly to all kinds of stimuli. The nerve fibers have different of transmitting the impulse depending on the diameter of the nerve and other factors. A fiber B fiber C fiber 353 RHPT TENS 26/09/1437 A fiber 8 Large myelinated, fast conducting, motor and sensory nerve fibers. A delta fibers Mediate afferent information pertaining to touch proprioception A alpha and kinesthesia. and beta The smallest of myelinated A fibers mediates nociceptive information primarily to superficial sharp, easy to localize pain. A fibers A gamma fibers fibers 353 RHPT TENS 26/09/1437 Convey information relative to changes in muscle length. 9 B fiber Smaller and slower conducting myelinated, efferent, preganglionic fibers of the autonomic nervous system 353 RHPT C fiber Unmyelinated post ganglionic fibers of the synaptic nervous system. Unmyelinated or poorly myelinated afferent fibers of the peripheral nerves. Group C fibers are small and slow conducting. It mediates nociceptive information, more indication of deep, hard to locating pain of chronic variety TENS 26/09/1437 Note 10 Myelinated nerve fibers conduct an electrical current at faster velocity then non-myelinated fibers C. Larger diameter fibers also has a rapid conduction velocity. So The largest myelinated afferent nerve fibers ( A alpha and beta) are the most rapid conducting and also the easiest to excite or depolarize. 353 RHPT TENS 26/09/1437 Pain pathway 11 Once nociceptors are stimulated the pain impulses passed to the spinal cord along two types of afferent nerve fibers: A delta fibers: Conduct impulses of acute sharp fast pain at speed of 6-30 m/sec. C fibers: Conduct impulses of chronic, dull slow pain at speed of 0.5-2 m/sec. 353 RHPT TENS 26/09/1437 Pain pathway 12 The nerve impulses giving rise to conscious pain travel in 4 regions of nervous system 1. The peripheral nervous system (nociceptors & afferent pathways) 2. Spinal cord (Dorsal horn, Spinothalamic tract & multisynaptic ascending system) 3. Brain stem & thalamus 4. Cerebral cortex 353 RHPT TENS 26/09/1437 First order neuron 13 • Start at peripheral receptor • Ends in the dorsal horn of the spinal cord Second order neuron • Start at dorsal horn of the spinal cord • Ends in the thalamus Third order neuron • Start at thalamus • Ends in the sensory cortex 353 RHPT TENS 26/09/1437 Afferent nerve fiber distribution 14 353 RHPT TENS 26/09/1437 Neurotransmitter – Substance “P” is believed to be the neurotransmitter involved at the synapse between 1st & 2nd order neurons. After synapse – the 2nd order neuron cross to the opposite side of the sp. cord & ascend to central pathways. Synapse 15 353 RHPT TENS 26/09/1437 The ascending tracts carry the 2nd order neuron (Sp.Cord) through central pathways concerned with nociception are Lateral Spinothalamic tract(LST) & Multi Synaptic Ascending system (MAS). The 2nd order neuron end in thalamus & synapse. Pathways – Ascending tracts 16 353 RHPT TENS 26/09/1437 Pathways – Ascending tracts 17 353 RHPT TENS 26/09/1437 Neuromodulation of Pain 18 The passage of nociceptive information is interrupted along several stages of ascending nociceptive pathways to produce Neuromodulation of pain. 1. Peripheral 2. Spinal segmental 3. Supraspinal 4. Cortical 353 RHPT TENS 26/09/1437 Neuromodulation of Pain Peripheral level 19 Intervention involves a ↓ in the amount of those chemicals released in response to tissue damage which are responsible for nociceptor activation. S.W.D, Hot Packs – Heat – Produce local vasodilatation - ↑ blood flow – removal of these chemicals. Ultrasound – Cell permeability - ↓ amount of exudates. Ice - ↓ amount of exudates 353 RHPT TENS 26/09/1437 Neuromodulation of Pain Spinal segmental level 20 It involves inhibition of activity of Aδ & C fibers before ascends further in neural axis. The inhibition – Pain modulation theories – Melzack & Wall 353 RHPT TENS 26/09/1437 Neuromodulation of Pain Supraspinal level 21 The placebo effect & counter irritation are also believed to operate at this level - Pain modulation theories – Melzack & Wall 353 RHPT TENS 26/09/1437 Neuromodulation of Pain Cortical level 22 It involves modification of individual perception & interpretation of pain. Behavior modification & cognitive strategies – psychological approach. 353 RHPT TENS 26/09/1437 Pain modulation Theories 23 Gate control theory Descending inhibition of pain 353 RHPT TENS 26/09/1437 Gate Control Theory– by Melzack & Wall 24 It serves as a major impetus to the commercial production of TENS. The modulation of pain transmission by altering afferent input to the spinal cord is called gate control theory. 353 RHPT TENS 26/09/1437 Gate Control Theory– by Melzack & Wall 25 According to this theory: Pain impulses are relayed from the periphery to the spinal cord through thin myelinated A delta and unmyelinated C fibers which synapse with neurons and interneurons in the dorsal horn. These dorsal horn neurons also received non-nociceptive input from other fibers as large myelinated low threshold A beta fibers that carry353 touch sensation.TENS RHPT 26/09/1437 26 Stimulation of A beta fibers inhibits pain transmission at the level of spinal cord as the following: - A beta fibers give off collateral which impinge on the terminations of A delta and C fibers in laminae of the dorsal horn where they produce presynaptic inhibition of pain impulses by secretion of substance called gama aminobuteric acid (GABA) which inhibit substance p secretion, thus preventing pain impulses from reaching higher centers. 353 RHPT TENS 26/09/1437 Stimuli – Aδ + c fiber – Dorsal horn – open gate for pain. Stimuli – Aβ – Presynaptic inhibition – closing of gate for pain. 27 353 RHPT TENS 26/09/1437 Descending inhibition of pain 28 When stimulation of A delta fibers, the pain impulse ascend up to the higher brain centers. Once the pain impulses have reached the higher centers, they activate certain areas in the midbrain which send descending inhibition impulses that travel back down to the spinal cord where they inhibit transmission of pain impulses. Descending inhibition of pain. 353 RHPT TENS 26/09/1437 Definition 29 Transcutaneous electrical nerve stimulation (TENS) is a non invasive method of electrical stimulation through intact skin and aimed to relief pain by specifically exciting peripheral nerves. Or it is the application of electrical stimulation to skin via surface electrode to stimulate nerve fibers to relief pain. 353 RHPT TENS 26/09/1437 Types of TENS mode 30 Conventional TENS (High TENS) Brief intense TENS Burst mode TENS Acupuncture (Low) TENS 353 RHPT TENS 26/09/1437 1. Conventional TENS (High TENS) 31 Conventional TENS (high frequency, short pulse , low intensity). 353 RHPT TENS 26/09/1437 Conventional TENS (High TENS) 32 Usually use stimulation at a relatively high frequency. Hi TENS is effective in treatment of acute pain of superficial nature as well as chronic pain. Relief pain through gait control theory. Patient sensation is tingling ,and paresthesia sensation. 353 RHPT TENS 26/09/1437 Conventional TENS (High TENS) 33 Parameters: - Low intensity: 12-30mA - High frequency: 100-150 Hz - Pulse duration: 50-80us - Duration: 20-60min 353 RHPT TENS 26/09/1437 2. Acupuncture (Low) TENS 34 Acupuncture TENS (low frequency, long pulse, high intensity) Stimulation parameters: -Low frequency: 1-5 Hz -High intensity: 30mA or more -Long pulse duration: 150-300us -Duration: 30-40min 353 RHPT TENS 26/09/1437 2. Acupuncture (Low) TENS 35 Low TENS is effective in treatment of chronic pain of damaged deep tissues Patient sensation is paresthesia , pulse muscle twitch seen. Pain relief through descending pain suppression system 353 RHPT TENS 26/09/1437 3-Brief intense TENS 36 It produce rapid onset but short term pain relief Use during painful procedures as wound debridement, joint mobilization. Parameters: • • • • • Amplitude : to patient’s tolerance. Pulse rate: 80-150Hz Duration: 15 min Pulse duration 50-250us Duration of pain relief: temporary. 353 RHPT TENS 26/09/1437 4- Burst mode TENS 37 It provide a packaging of stimuli groups ranging from 1-10 It combine characters of both low and high TENS Relief pain through endogenous opiate 353 RHPT TENS 26/09/1437 4- Burst mode TENS 38 Produce more comfortable contraction. Parameters: - amplitude: comfortable paresthesia - Frequency: 50-100Hz - Pulse duration: 50-200 us - Duration: 20-30min - Duration for pain relief: long lasting 353 RHPT TENS 26/09/1437 Indications of TENS 39 Acute and chronic post operative pain Musculoskeletal pain” sprain, strain, myofascial” Neurological pain as in, trigeminal neuralgia, and peripheral nerve injuries. Obstetric pain “ during delivery” Arthritic pain “ osteoarthritis, rheumatoid” Acute and chronic low back pain 353 RHPT 26/09/1437 TENS Other recent indication of TENS: 40 Improve cutaneous blood flow Anti emetic effect Wound healing Fracture healing (non-united fracture) 353 RHPT Reduction of neglect in post stroke patients TENS 26/09/1437 Contraindication 41 Anesthetic skin Patient at risk Over the carotid sinus Pregnancy Allergy Epilepsy Treatment while driving 353 RHPT TENS 26/09/1437 Parameters used in TENS unit 42 - - Waveforms : biphasic waveform is used. It may be square ,rectangular, triangular, or sine wave. Each type used according the patient’s case as the triangular used for acute pain. Frequency : High TENS 80- 120 Hz as in acute pain Low TENS 1-20 Hz as in chronic pain 353 RHPT TENS 26/09/1437 Parameters used in TENS unit 43 - - - - Pulse width: Vary from 50-400 us For normal neuromuscular system100-150us For neurological damage 200-300us Amplitude based on the patient’s sensation Modulation: There is a variation in either pulse duration, frequency, or amplitude parameter in a cycle fashion This help to overcome nerve accommodation. 353 RHPT TENS 26/09/1437 Types of Electrodes 44 Carbon rubber Self adhesive Aluminum foil • coated with a conductive gel prior to attachment to the skin. • become more popular • Lint pad covering 353 RHPT TENS 26/09/1437 Advantage of TENS 45 Non invasive Portable Safe Cheaper Few contraindications and precaution Non addictive 353 RHPT TENS 26/09/1437 Disadvantage 46 Fail of patients to tolerate the sensations Skin irritation due to allergic reaction to gel Chemical burn Some patients fail to respond to the treatment 353 RHPT TENS 26/09/1437 Electrode placement: 47 Over the painful site, or trigger point. Acupuncture point proximal and distal to the painful area. Over the same dermatome. In case the pain is distributed across a large area with no definite trigger point. Peripheral nerves. Electrodes are placed in the line of the nerve where it is particularly superficial. This method is effective in treatment of neurological pain. 353 RHPT TENS 26/09/1437 Electrode placement: 48 Spinal nerve root associated with pain. The electrodes should be placed parallel to the spinal column. Contiguous placement. In conditions such as postoperative incisions, lacerations in which direct electrode placement is contraindicated as in incisional pain. The electrodes are placed parallel and approximately 1cm from the incision using 2 electrodes or in crossed pattern if 4 electrodes are used. 353 RHPT TENS 26/09/1437 Treatment setup and application 49 Prepare the patient. Adjust output parameters. Place the electrodes in position. Increase the output intensity slowly to the desired sensation level according to the patient. Usually with conventional TENS the subjects feel tingling sensation with no muscle twitch, while with acupuncture TENS subjects feel more strong sensation but not unpleasant with visible muscle contraction. 353 RHPT 26/09/1437 TENS 50 Electrode positions for common pain conditions (A) anterior view, 353 RHPT TENS 26/09/1437 51 Electrode positions for common pain conditions (B) posterior view 353 RHPT TENS 26/09/1437 Duration and Frequency of Treatment 52 Conventional TENS may be used as needed, but caution should be used when applied while the patient is sleeping. Patient response usually immediate ( high TENS), but adapt quickly to this type of stimulation (the reason many unit have included modulation modes). Acupuncture TENS and burst TENS may be given as needed in treatment bouts not exceeding 30 minutes and may be repeated 3 or 4 times daily. 353 RHPT TENS 26/09/1437 TENS Application in Non-united Fracture 53 Treatment Parameters Frequency: 120 Hz Pulse duration: 300 μsec Intensity: barely sensed by the patients (lowest possible) Duration: 1 hour /session, 4 times daily Electrodes placement If the fracture is enclosed in a blaster cast electrodes should be placed proximal and distal to the cast. 353 RHPT 26/09/1437 TENS If the fracture site is free of casting, use two electrodes one placed on either side of the of the fracture site. 54 Electrodes placement for non-union fracture with the cast present. 353 RHPT 26/09/1437 TENS 55 Electrodes placement for non-union fracture with no cast present. 353 RHPT TENS 26/09/1437 Precautions 56 Intense or prolonged stimulation may result in muscle spasm or muscle soreness. Improper use can result in electrode burn or skin irritation Contact dermatitis may occur after prolonged use. Careful cleansing of the skin and the use of different sites for the electrodes help to avoid that. 353 RHPT TENS 26/09/1437