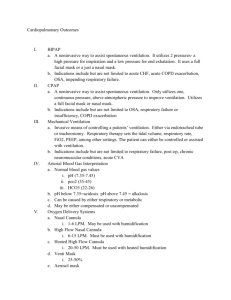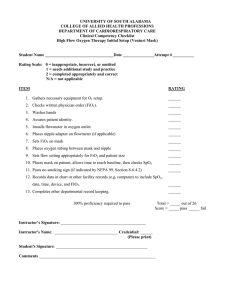
Respiratory diagnostic procedures are used to evaluate a client’s respiratory status by checking indicators such as the oxygenation of the blood, lung functioning, and the integrity of the airway. Respiratory diagnostic procedures nurses should be knowledgeable about include pulmonary function tests, arterial blood gases, bronchoscopy, and thoracentesis Pulmonary function tests (PFTs) determine lung function and breathing difficulties. ● PFTs measure lung volumes and capacities, diffusion capacity, gas exchange, flow rates, and airway resistance, along with distribution of ventilation. ● Helpful in identifying clients who have lung disease. ● Commonly performed for clients who have dyspnea. ● Can be performed before surgical procedures to identify clients who have respiratory risks. ● If client is a smoker, instruct client not to smoke 6 to 8 hr prior to testing. ● If a client uses inhalers, withhold 4 to 6 hr prior to testing. (This can vary according to facility policy.) Pulmonary function tests – They include tests that measure lung size and air flow, such as spirometry and lung volume tests. Other tests measure how well gases such as oxygen get in and out of your blood. These tests include pulse oximetry and arterial blood gas tests. Another pulmonary function test, called fractional exhaled nitric oxide (FeNO), measures nitric oxide, which is a marker for inflammation in the lungs. You may have one or more of these tests to diagnose lung and airway diseases, compare your lung function to expected levels of function, monitor if your disease is stable or worsening, and see if your treatment is working. The purpose, procedure, discomfort, and risks of each test will vary. Spirometry measures the rate of air flow and estimates lung size. For this test, you will breathe multiple times, with regular and maximal effort, through a tube that is connected to a computer. Some people feel lightheaded or tired from the required breathing effort. Lung volume tests are the most accurate way to measure how much air your lungs can hold. The procedure is similar to spirometry, except that you will be in a small room with clear walls. Some people feel lightheaded or tired from the required breathing effort. Lung diffusion capacity assesses how well oxygen gets into the blood from the air you breathe. For this test, you will breathe in and out through a tube for several minutes without having to breathe intensely. You also may need to have blood drawn to measure the level of hemoglobin in your blood. Pulse oximetry estimates oxygen levels in your blood. For this test, a probe will be placed on your finger or another skin surface such as your ear. It causes no pain and has few or no risks. Arterial blood gas tests directly measure the levels of gases, such as oxygen and carbon dioxide, in your blood. Arterial blood gas tests are usually performed in a hospital, but may be done in a doctor’s office. For this test, blood will be taken from an artery, usually in the wrist where your pulse is measured. You may feel brief pain when the needle is inserted or when a tube attached to the needle fills with blood. It is possible to have bleeding or infection where the needle was inserted. Fractional exhaled nitric oxide tests measure how much nitric oxide is in the air that you exhale. For this test, you will breathe out into a tube that is connected to the portable device. It requires steady but not intense breathing. It has few or no risks. https://medlineplus.gov/lab-tests/lung-function-tests/ https://www.youtube.com/watch?v=46caPxJVPQI Incentive Spirometry (Spirometer) NCLEX Review for Nursing with Demonstration Arterial Blood Gas 1. An arterial blood gas (ABG) sample reports the status of oxygenation and acid-base balance of the blood. ● An ABG measures the following. ◯ pH: amount of free hydrogen ions in the arterial blood (H+) ◯ PaO2: partial pressure of oxygen ◯ PaCO2: partial pressure of carbon dioxide ◯ HCO3 ̄: concentration of bicarbonate in arterial blood ◯ SaO2: percentage of oxygen bound to Hgb as compared with the total amount that can be possibly carried ● ABGs can be obtained by an arterial puncture or through an arterial line. Respiratory Management Oxygen is a tasteless and colorless gas that accounts for 21% of atmospheric air. Oxygen is used to maintain adequate cellular oxygenation. it is used in the treatment of many acute and chronic respiratory problems. Oxygen is administered in an attempt to maintain an saO2 of 95% to 100% by using the lowest amount of oxygen without putting the client at risk for complications. Clients who cannot spontaneously breathe on their own require mechanical ventilation. This can include clients who need respiratory assistance due to severe respiratory disease, general anesthesia, trauma, or other illnesses. Oxygen delivery devices Supplemental oxygen can be delivered by a variety of methods based on the client’s particular circumstances. The percentage of oxygen delivered is expressed as the fraction of inspired oxygen (FiO2). While the client is receiving oxygen, the nurse should continue to monitor vital signs, including SaO2 for changes, and intervene as needed. LOW‐FLOW Oxygen delivery systems These deliver varying amounts of oxygen based on the method and the client’s breathing pattern. Nasal cannula ● A length of tubing with two small prongs for insertion into the nares ● FiO2 24% to 44% at flow rates of 1 to 6 L/min ADVANTAGES ● Safe, easy to apply, comfortable, and well tolerated. ● The client is able to eat, talk, and ambulate. DISADVANTAGES ● FiO2 varies with the flow rate, and the client’s rate and depth of breathing. ● Extended use can lead to skin breakdown and drying of the mucous membranes. ● Tubing is easily dislodged. NURSING ACTIONS ● Assess patency of the nares. ● Ensure that the prongs fit in the nares properly. ● Use water-soluble gel to prevent dry nares. ● Provide humidification for flow rates of 4 L/min and greater. Simple face mask ● Covers the client’s nose and mouth. ● FiO2 40% to 60% at flow rates of 5 to 8 L/min. (The minimum flow rate is 5 L/min to ensure flushing of CO2 from the mask.) ADVANTAGES: A face mask is easy to apply and can be more comfortable than a nasal cannula. DISADVANTAGES ● Flow rates of less than 5 L/min can result in rebreathing of CO2. ● Device is poorly tolerated by clients who have anxiety or claustrophobia. ● Eating, drinking, and talking are impaired. ● Use caution with clients who have a high risk of aspiration or airway obstruction. Moisture and pressure can collect under the mask and cause skin breakdown. NURSING ACTIONS ● Assess proper fit to ensure a secure seal over the nose and mouth. ● Ensure that the client wears a nasal cannula during meals. Partial rebreather mask ● Covers the client’s nose and mouth ● FiO2 40% to 75% at flow rates of 6 to 11 L/min ADVANTAGES: The mask has a reservoir bag attached with no valve, which allows the client to rebreathe up to one third of exhaled air together with room air. DISADVANTAGES ● Complete deflation of the reservoir bag during inspiration causes CO2 buildup. ● FiO2 varies with the client’s breathing pattern. ● Mask is poorly tolerated by clients who have anxiety or claustrophobia. ● Eating, drinking, and talking are impaired. ● Use with caution for clients who have a high risk of aspiration or airway obstruction. NURSING ACTIONS ● Keep the reservoir bag from deflating by adjusting the oxygen flow rate to keep it inflated. ● Assess proper fit to ensure a secure seal over the nose and mouth. ● Assess for skin breakdown beneath the edges of the mask and bridge of nose. ● Ensure that the client uses a nasal cannula during meals. Nonrebreather mask ● Covers the client’s nose and mouth ● FiO2 80% to 95% at flow rates of 10 to 15 L/min to keep the reservoir bag two-thirds full during inspiration and expiration ADVANTAGES ● Delivers the highest O2 concentration possible (except for intubation). ● A one-way valve situated between the mask and reservoir allows the client to inhale maximum O2 from the reservoir bag. The two exhalation ports have flaps covering them that prevent room air from entering the mask. DISADVANTAGES ● The valve and flap on the mask must be intact and functional during each breath. ● Poorly tolerated by clients who have anxiety or claustrophobia. ● Eating, drinking, and talking are impaired. ● Use with caution for clients who have a high risk of aspiration or airway obstruction. NURSING ACTIONS ● Perform an hourly assessment of the valve and flap. ● Assess proper fit to ensure a secure seal over the nose and mouth. ● Assess for skin breakdown beneath the edges of the mask and bridge of nose. ● Ensure that the client uses a nasal cannula during meals. High‐FLOW Oxygen delivery systems These deliver precise amounts of oxygen when properly fitted. Venturi mask ● Covers the client’s nose and mouth ● FiO2 24% to 60% at flow rates of 4 to 12 L/min via different sizes of adapters, which allow specific amounts of air to mix with oxygen ADVANTAGES ● Delivers the most precise oxygen concentration. ● Humidification is not required. ● Best suited for clients who have chronic lung disease. DISADVANTAGES: Use of a Venturi mask is expensive. NURSING ACTIONS ● Assess frequently to ensure an accurate flow rate. ● Make sure the tubing is free of kinks. ● Assess for skin breakdown beneath the edges of the mask, particularly on the nares. ● Ensure that the client wears a nasal cannula during meals. Aerosol mask, face tent, and tracheostomy collar ● Face tent fits loosely around the face and neck. ● Tracheostomy collar is a small mask that covers a surgically created opening in the trachea. ● FiO2 24% to 100% at flow rates of at least 10 L/min. (Provide high humidification with oxygen delivery.) ADVANTAGES ● Good for clients who do not tolerate masks well. ● Useful for clients who have facial trauma, burns, or thick secretions. DISADVANTAGES: High humidification requires frequent monitoring. NURSING ACTIONS ● Empty condensation from the tubing often. ● Ensure that there is adequate water in the humidification canister. ● Ensure that the aerosol mist leaves from the vents during inspiration and expiration. ● Make sure the tubing does not pull on the tracheostomy. T‐piece FiO2 24% to 100% at flow rates of at least 10 L/min ADVANTAGES: Can be used for clients who have tracheostomies, laryngectomies, or endotracheal tubes (ET). DISADVANTAGES: High humidification requires frequent monitoring. NURSING ACTIONS ● Ensure that the exhalation port is open and uncovered. ● Ensure that the T-piece does not pull on the tracheostomy or ET tube. ● Ensure that the mist is evident during inspiration and expiration. Oxygen therapy INDICATIONS Potential diagnoses Hypoxemia and hypoxia: ● Hypoxemia is an inadequate level of oxygen in the blood. Hypovolemia, hypoventilation, and interruption of arterial flow can lead to hypoxemia. ● Hypoxia is a decrease in tissue oxygenation. Client Presentation Early findings ● Tachypnea ● Tachycardia ● Restlessness ● Pale skin and mucous membranes ● Elevated blood pressure ● Findings of respiratory distress (use of accessory muscles, nasal flaring, tracheal tugging, and adventitious lung sounds) Late findings ● Confusion and stupor ● Cyanotic skin and mucous membranes ● Bradypnea ● Bradycardia ● Hypotension ● Cardiac dysrhythmias Considerations Preparation OF The Client ● Explain all procedures to the client. ● Place the client in semi-Fowler’s or Fowler’s position to facilitate breathing and promote chest expansion. ● Ensure that all equipment is working properly. Ongoing Care ● Provide oxygen therapy at the lowest flow that will correct hypoxemia. ● Assess/monitor respiratory rate, rhythm and effort, lung sounds, and SaO2 to determine the client’s need for supplemental oxygen. ◯Manifestations of hypoxemia are shortness of breath, anxiety, tachypnea, tachycardia, restlessness, pallor or cyanosis of the skin or mucous membranes, adventitious breath sounds, and confusion. ◯ Manifestations of hypercarbia (elevated levels of CO2) are restlessness, hypertension, and headache. ● Monitor diagnostic reports that show information related to oxygenation, including ABGs. ● Promote good oral hygiene, and provide as needed. ● Promote turning, coughing, deep breathing, use of incentive spirometer, and suctioning. ● Promote rest, and decrease environmental stimuli. ● Provide emotional support for clients who appear anxious. ● Assess nutritional status. Provide supplements as prescribed. ● Assess/monitor skin integrity. Provide moisture and pressure-relief devices as indicated. ● Assess/monitor and document the client’s response to oxygen therapy. ● Titrate oxygen to maintain prescribed oxygen saturation. ● Discontinue supplemental oxygen gradually. COMPLICATIONS Oxygen toxicity ● Oxygen toxicity can result from high concentrations of oxygen (typically above 50%), long durations of oxygen therapy (typically more than 24 to 48 hr), and the client’s degree of lung disease. ● Manifestations include a nonproductive cough, substernal pain, nasal stuffiness, nausea, vomiting, fatigue, headache, sore throat, and hypoventilation. NURSING ACTIONS ● Use the lowest level of oxygen necessary to maintain the prescribed SaO2. ● Monitor ABGs. Notify the provider if results are outside the expected or prescribed ranges. ● Use an oxygen mask with continuous positive airway pressure (CPAP) or bi-level positive airway pressure (BiPAP) if prescribed to help decrease the amount of oxygen needed. ● Use positive end expiratory pressure (PEEP) as prescribed while the client is receiving mechanical ventilation to help decrease the amount of needed oxygen. Oxygen‐induced hypoventilation Oxygen-induced hypoventilation can develop in clients who have COPD and chronic hypoxemia with hypercarbia. NURSING ACTIONS ● Monitor respiratory rate and pattern, level of consciousness, and SaO2. ● Provide oxygen therapy at the lowest flow rate that manages hypoxemia. ● If the client tolerates it, use a Venturi mask to deliver precise oxygen levels. ● Notify the provider of findings of respiratory depression, such as a decreased respiratory rate or a decreased level of consciousness. Combustion Oxygen is combustible. NURSING ACTIONS ● Post “No Smoking” or “Oxygen in Use” signs to alert others of a fire hazard. ● Know where the closest fire extinguisher is located. ● Educate the client and others about the fire hazard of smoking during oxygen use. ● Have the client wear a cotton gown because synthetic or wool fabrics can generate static electricity. ● Ensure that all electric devices (razors, hearing aids, radios) are working well. ● Ensure electric machinery (monitors, suction machines) are well-grounded. ● Do not use volatile, flammable materials (alcohol or acetone) near clients who are receiving oxygen. Noninvasive positive pressure ventilation Continuous positive airway pressure CPAP Provides positive pressure using a leak-proof mask via noninvasive positive-pressure ventilation device. ● The device is to keep the airways throughout the respiratory cycle open and improve gas exchange in the alveoli. ● Most effective treatment for sleep apnea because the positive pressure acts as a splint to keep the upper airway and trachea open during sleep Bi‐level positive airway pressure BiPAP Machine cycles to provide a set positive inspiratory pressure when inspiration takes place and then during expiration to deliver a lower set end expiratory pressure. ● Requires wearing a leak-proof mask. ● Most often used for clients who have COPD and who require ventilatory assistance. NURSING ACTIONS ● Assess skin around the masks for breakdown as a tight seal is required. ● Check the percentage of oxygen on the machine (both) for both the inspiratory pressure and expiratory pressure when the client is receiving BiPAP. Transtracheal oxygen therapy Delivers oxygen directly in to the lungs per a small, flexible catheter that is passed through the trachea via a small incision. ● The oxygen delivery is reduced by 55% for a client at rest and 30% for a client who is active. ● The catheter is less visible and avoids irritation that occurs from the use of nasal prongs. Endotracheal tube and endotracheal intubation ETT INDICATIONS ● A tube is inserted through the client’s nose or mouth into the trachea. This allows for emergency airway management of the client. ● Oral intubation is the easiest and quickest form of intubation and is often performed in the emergency department. ● Nasal intubation is performed when the client has facial or oral trauma. This route is not used if the client has a clotting problem. Placement ● Intubation is typically performed by a nurse anesthetist, anesthesiologist, critical care or emergency physician, or pulmonologist. ● A chest x-ray verifies correct placement of the endotracheal (ET) tube. ● ET tubes can be cuffed or uncuffed. The cuff on the tracheal end of an ET tube is inflated to ensure proper placement and the formation of a seal between the cuff and the tracheal wall. This prevents air from leaking around the ET tube. ● The seal ensures that an adequate amount of tidal volume is delivered by the mechanical ventilator when attached to the external end of the ET tube. ● The client is unable to talk when the cuff is inflated. NURSING ACTIONS ● Have resuscitation equipment to include a manual resuscitation bag with a face mask at the bedside at all times. ● Ensure the intubation attempts last no longer than 30 seconds and then reoxygenate before another attempt to intubate. ● Monitor vital signs and verify ET tube placement by checking end-tidal carbon dioxide levels and chest x-ray. ● Auscultate for breath sounds bilaterally after intubation. ● Observe for symmetric chest movement. ● Stabilize the endotracheal tube with a tube-holding device or secure with tape. ● Monitor for hypoxemia, dysrhythmias, and aspiration. Mechanical ventilation Mechanical ventilation provides breathing support until lung function is restored, delivering 100% oxygen that is warmed (body temperature 37° C [98.6° F]) and% humidified at FiO2 levels between 21% to 100%. Positive-pressure ventilators deliver air to the lungs under pressure throughout inspiration to keep the alveoli open and to prevent alveolar collapse during expiration. Benefits include the following. ◯ Forced/enhanced lung expansion ◯ Improved gas exchange (oxygenation) ◯ Decreased work of breathing Mechanical ventilation can be delivered via: ◯ ET tube. ◯ Tracheostomy tube. Mechanical ventilators can be cycled based on pressure, volume, time, and/or flow. INDICATIONS To maintain a patent airway and adequate oxygen saturation of 95% or greater. Potential diagnoses ● Hypoxemia, hypoventilation with respiratory acidosis ◯ Airway trauma ◯ Exacerbation of COPD ◯ Acute pulmonary edema due to myocardial infarction or heart failure ◯ Asthma attack ◯ Head injuries, cerebrovascular accident, or coma ◯ Neurological disorders (multiple sclerosis, myasthenia gravis, Guillain‐Barré) ◯ Obstructive sleep apnea ● Respiratory support following surgery (decrease workload) ● Respiratory support while under general anesthesia or heavy sedation CONSIDERATIONS Preparation OF The Client ● Explain the procedure to the client. ● Establish a method for the client to communicate, such as asking yes/no questions, providing writing materials, using a dry-erase and/or picture communication board, or lip reading. Ongoing Care Maintain a patent airway. Assess the position and placement of tube. Document tube placement in centimeters at the client’s teeth or lips. Use two staff members for repositioning and resecuring the tube. Apply protective barriers (soft wrist restraints) according to hospital protocol to prevent self-extubation. Use caution when moving the client Suction oral and tracheal secretions to maintain tube patency. Support ventilator tubing to prevent mucosal erosion and displacement. Have a resuscitation bag with a face mask available at the bedside at all times in case of ventilator malfunction or accidental extubation. ● Assess respiratory status every 1 to 2 hr: breath sounds equal bilaterally, presence of reduced or absent breath sounds, respiratory effort, or spontaneous breaths. ● Suction the tracheal tube to clear secretions from the airway. ● Monitor and document ventilator settings hourly. ◯ Rate, FiO2, and tidal volume ◯ Mode of ventilation ◯ Use of adjuncts (PEEP, CPAP) ◯ Plateau or peak inspiratory pressure (PIP) ◯ Alarm settings ● Monitor ventilator alarms, which signal if the client is not receiving the correct ventilation. ◯ Never turn off ventilator alarms. ◯ There are three types of ventilator alarms. Volume (low pressure) alarms indicate a low exhaled volume due to a disconnection, cuff leak, and/or tube displacement. Pressure (high pressure) alarms indicate excess secretions, client biting the tubing, kinks in the tubing, client coughing, pulmonary edema, bronchospasm, or pneumothorax. Apnea alarms indicate that the ventilator does not detect spontaneous respiration in a preset time period. ● Maintain adequate (but not excessive) volume in the cuff of the endotracheal tube. ◯ Assess the cuff pressure at least every 8 hr. Maintain the cuff pressure below 20 mm Hg (or 20 to 30 cm H2O) to reduce the risk of tracheal necrosis. ◯ Assess for an air leak around the cuff (client speaking, air hissing, or decreasing SaO2). Inadequate cuff pressure can result in inadequate oxygenation and/or accidental extubation. ● Administer medications as prescribed. ◯ Analgesics: morphine and fentanyl ◯ Sedatives: propofol, diazepam, lorazepam, midazolam, and haloperidol ■ Clients receiving mechanical ventilation can require sedation or paralytic agents to prevent competition between extrinsic and intrinsic breathing and the resulting effects of hyperventilation. ◯ Neuromuscular blocking agents: pancuronium, atracurium, and vecuronium are infrequently used in the clinical setting due to the their long half-life. ■ Neuromuscular-blocking agents paralyze muscles, but do not sedate or relieve pain. The use of a sedative or analgesic agent in conjunction with a neuromuscular blocking agent is typically prescribed. ◯ Ulcer-preventing agents: famotidine or lansoprazole ◯ Antibiotics for established infections ● Reposition the oral endotracheal tube every 24 hr or according to protocol. Assess for skin breakdown. ◯ Older adult clients have fragile skin and are more prone to skin and mucous membrane breakdown. Older adult clients have decreased oral secretions. They require frequent, gentle skin and oral care. ● Provide adequate nutrition. ◯ Assess gastrointestinal functioning every 8 hr. ◯ Monitor bowel habits. ◯ Administer enteral or parenteral feedings as prescribed. ● Continually monitor the client during the weaning process and watch for signs of weaning intolerance. ◯ Respirations greater than 30/min or less than 8/min ◯ Blood pressure or heart rate changes more than 20% of baseline ◯ SaO2 less than 90% ◯ Dysrhythmias, elevated ST segment ◯ Significant decrease in tidal volume ◯ Labored respirations, increased use of accessory muscles, and diaphoresis ◯ Restlessness, anxiety, and decreased level of consciousness ● Have a manual resuscitation bag with a face mask and oxygen readily available at the client’s bedside. ● Have reintubation equipment at bedside. ● Suction the oropharynx and trachea. ● Deflate the cuff on the endotracheal tube, and remove the tube during peak inspiration. ● Following extubation, monitor for signs of respiratory distress or airway obstruction (ineffective cough, dyspnea, stridor). ● Assess SpO2 and vital signs every 5 min. ● Encourage coughing, deep breathing, and use of the incentive spirometer. ● Reposition the client to promote mobility of secretions. ● Older adult clients have decreased respiratory muscle strength and chest wall compliance, which makes them more susceptible to aspiration, atelectasis, and pulmonary infections. Older adult clients require more frequent position changes to promote mobility of secretions COMPLICATIONS Trauma Barotrauma (damage to the lungs by positive pressure) can occur due to a pneumothorax, subcutaneous emphysema or pneumomediastinum. Volutrauma (damage to the lungs by volume delivered from one lung to the other). Fluid retention Fluid retention in clients who are receiving mechanical ventilation is due to decreased cardiac output, activation of renin-angiotensin-aldosterone system, and/or ventilator humidification. NURSING ACTIONS: Monitor intake and output, weight, breath sounds, and endotracheal secretions. Oxygen toxicity Oxygen toxicity can result from high concentrations of oxygen (typically greater than 50%), long durations of oxygen therapy (typically more than 24 to 48 hr), and/or the client’s degree of lung disease. NURSING ACTIONS: Monitor for fatigue, restlessness, severe dyspnea, tachycardia, tachypnea, crackles, and cyanosis. Hemodynamic compromise Mechanical ventilation has a risk of increased thoracic pressure (positive pressure), which can result in decreased venous return. NURSING ACTIONS: Monitor for tachycardia, hypotension, urine output less than or equal to 30 mL/hr, cool, clammy extremities, decreased peripheral pulses, and a decreased level of consciousness. Aspiration Keep the head of the bed elevated 30° at all times to decrease the risk of aspiration. NURSING ACTIONS: Check residuals every 4 hr if the client is receiving enteral feedings to decrease the risk of aspiration. Gastrointestinal ulceration (stress ulcer) Gastric ulcers can be evident in clients receiving mechanical ventilation. NURSING ACTIONS ● Monitor gastrointestinal drainage and stools for occult blood. ● Administer ulcer prevention medications (sucralfate and histamine2 blockers).