Respiratory System 1
advertisement
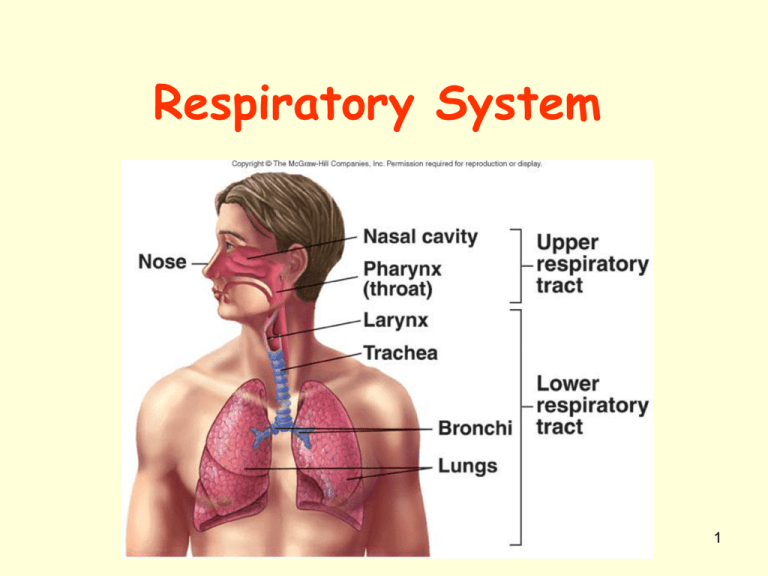
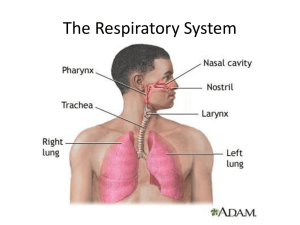
Respiratory System 1 Respiration • Ventilation: Movement of air into & out of lungs • External respiration: Gas exchange b/n air in lungs & blood – Transport of O2 and CO2 in the blood • Internal respiration: Gas exchange b/n the blood & tissues 2 Respiratory System Functions • Gas exchange: O2 enters blood & CO2 leaves • Regulation of blood pH: Altered by changing blood CO2 levels • Voice production: Movement of air past vocal folds makes sound & speech • Olfaction: Smell occurs when airborne molecules drawn into nasal cavity • Protection: Against microorganisms by preventing entry & removing them 3 Respiratory System Divisions • Upper tract – Nose, pharynx & associated structures • Lower tract – Larynx, trachea, bronchi, lungs 4 Nose and Pharynx • Nose – External nose – Nasal cavity • Functions – Passageway for air – Cilia cleans the air – Mucous humidifies (moistens air inhaled) – Capillaries warm air – Smell – Along with paranasal sinuses are resonating chambers for speech • Pharynx – Common opening for digestive & respiratory systems – Three regions • Nasopharynx • Oropharynx • Laryngopharynx 5 Larynx • Functions – Maintain an open passageway for air movement – Epiglottis & vestibular folds prevent swallowed material from moving into larynx (can move to cover trachea) – Vocal folds are primary source of sound production 6 Structure of Larynx – AKA voice box – Thyroid cartilage: AKA Adam’s apple • Protects vocal cords • Moves when you swallow – Epiglottis: closes off larynx so food & liquid travel down the esophagus 7 Voice Production • False vocal cords: assist w/ hold breath • True vocal cords: – Space between them called glottis – Vibration produces sound – In combination with tongue, mouth, & nose to produce words 8 Trachea • Windpipe • Divides to form Insert Fig 23.5 all but b – C-shaped cartilage with smooth muscle which keeps diameter to allow fluent air flow – Lined with cilia and mucus to moisten and clean air – Primary bronchi – Carina: Cough reflex 9 Organs of Respiration • Trachea: – AKA windpipe – Smooth muscle supported by C-shaped rings of cartilage • food can travel down esophagus easier – Passageway for air from larynx to bronchi – Lined w/ cilia & mucous 10 Tracheobronchial Tree • Conducting zone – Trachea to terminal bronchioles which is ciliated for removal of debris – Passageway for air movement – Cartilage holds tube system open & smooth muscle controls tube diameter • Respiratory zone – Respiratory bronchioles to alveoli – Site for gas exchange 11 Organs of Respiration • Bronchi: – Left & right primary bronchi branch off trachea – Lined w/ cilia – Supported by cartilage 12 Bronchial Tree Primary bronchi Secondary bronchi Tertiary bronchi bronchioles Terminal bronchioles Respiratory bronchioles Alveolar ducts Alveolar sacs alveoli 13 Terminal bronchiole: the last portion of the nonrespiratory conducting airway, which subdivide into respiratory bronchioles. Respiratory bronchiole: the final branch of a bronchiole, communicating directly with the alveolar ducts; a subdivision of a terminal bronchiole, it has alveolar outcroppings and itself divides into several alveolar ducts. 14 Bronchioles and Alveoli 15 Alveolus and Respiratory Membrane 16 Lungs • Two lungs: Principal organs of respiration – Right lung: Three lobes – Left lung: Two lobes 17 Organs of Respiration • Alveoli: – Extremely thin-walled sacs covered w/ capillaries – CO2 & O2 move by diffusion across the respiratory membrane – About 300 million alveoli in two lungs – Size of a tennis court 18 Organs of Respiration • Alveoli: – Surfactant lines the alveoli to aid diffusion & decrease surface tension – To prevent the alveoli from collapsing & sticking shut 19 Pleura • Pleural fluid produced by pleural membranes – Acts as lubricant – Helps hold parietal & visceral pleural membranes together 20 Ventilation • Movement of air into and out of lungs • Air moves from area of higher pressure to area of lower pressure (AKA Diffusion) • Pressure is inversely related to volume 21 Inspiration • Breathing in • When pressure in the lungs is less than the air pressure in the atmosphere • Diaphragm— will contract and lower, increasing the size of the thoracic cage 22 Inspiration • Increased volume will decrease the pressure & the lungs will expand 23 Expiration • Breathing out • When the pressure inside the lungs is greater than the pressure in the atmosphere • Diaphragm— relaxes and rises; decreases the size of the thoracic cage 24 Expiration • Decreased volume will increase pressure & lungs will decrease and push air out 25 Internal Respiration • Exchange of O2 and CO2 between tissue capillaries and tissue cells • CO2 moves from high concentration in cells to low concentration in blood 26 External Respiration • Conversion of deoxygenated blood to oxygenated blood – Aided by thin membranes – Large surface area – Narrow capillaries 27 Changing Alveolar Volume • Lung recoil – Causes alveoli to collapse resulting from • Elastic recoil and surface tension – Surfactant: Reduces tendency of lungs to collapse • Pleural pressure – Negative pressure can cause alveoli to expand – Pneumothorax is an opening between pleural cavity & air that causes a loss of pleural pressure 28 Compliance • Measure of the ease with which lungs & thorax expand – The greater the compliance, the easier it is for a change in pressure to cause expansion – A lower-than-normal compliance means the lungs and thorax are harder to expand • Conditions that decrease compliance – Pulmonary fibrosis – Pulmonary edema – Respiratory distress syndrome 29 Pulmonary Volumes • Tidal volume – Volume of air inspired or expired during a normal inspiration or expiration • Inspiratory reserve volume – Amount of air inspired forcefully after inspiration of normal tidal volume • Expiratory reserve volume – Amount of air forcefully expired after expiration of normal tidal volume • Residual volume – Volume of air remaining in respiratory passages and lungs after the most forceful expiration 30 Pulmonary Capacities • Inspiratory capacity – Tidal volume plus inspiratory reserve volume • Functional residual capacity – Expiratory reserve volume plus the residual volume • Vital capacity – Sum of inspiratory reserve volume, tidal volume, and expiratory reserve volume • Total lung capacity – Sum of inspiratory and expiratory reserve volumes plus the tidal volume and residual volume 31 Spirometer and Lung Volumes/Capacities 32 Minute and Alveolar Ventilation • Minute ventilation: Total amount of air moved into & out of respiratory system per minute • Respiratory rate or frequency: Number of breaths taken per minute • Anatomic dead space: Part of respiratory system where gas exchange does not take place • Alveolar ventilation: How much air per minute enters the parts of the respiratory system in which gas exchange takes place33 Physical Principles of Gas Exchange • Partial pressure – The pressure exerted by each type of gas in a mixture • Diffusion of gases through liquids – Concentration of a gas in a liquid is determined by its partial pressure and its solubility coefficient 34 Physical Principles of Gas Exchange • Diffusion of gases through the respiratory membrane – Depends on membrane’s thickness, the diffusion coefficient of gas, surface areas of membrane, partial pressure of gases in alveoli and blood • Relationship between ventilation and pulmonary capillary flow – Increased ventilation or increased pulmonary capillary blood flow increases gas exchange – Physiologic shunt is deoxygenated blood returning from lungs 35 Oxygen & Carbon Dioxide Diffusion Gradients • Oxygen – Moves from alveoli into blood. Blood is almost completely saturated with oxygen when it leaves the capillary – C02 in blood decreases because of mixing with deoxygenated blood – Oxygen moves from tissue capillaries into the tissues • Carbon dioxide – Moves from tissues into tissue capillaries – Moves from pulmonary capillaries into the alveoli 36 Hemoglobin and Oxygen Transport • Oxygen is transported by hemoglobin (98.5%) and is dissolved in plasma (1.5%) 37 Transport of Carbon Dioxide • Carbon dioxide is transported as bicarbonate ions (70%) in combination with blood proteins (23%) and in solution with plasma (7%) 38 Herring-Breuer Reflex • Limits the degree of inspiration and prevents overinflation of the lungs – Infants • Reflex plays a role in regulating basic rhythm of breathing and preventing overinflation of lungs – Adults • Reflex important only when tidal volume large as in exercise 39 Ventilation in Exercise • Ventilation increases abruptly – – – – At onset of exercise Movement of limbs has strong influence Learned component Decreases slightly • Ventilation increases gradually – After immediate increase, gradual increase occurs (4-6 minutes) – Anaerobic threshold is highest level of exercise without causing significant change in blood pH • If exceeded, lactic acid produced by skeletal muscles 40 Disorders • Asthma— spasms of smooth muscle in the bronchioles • Lung cancer – Constant irritation produces excess mucous and puts unnecessary stress on the bronchi – Alveoli destroyed by WBC’s acting on the irritation – Structural cells disappear and cancer cells take over 41 Disorders • Emphysema— alveolar walls lose their elasticity – Some alveoli merge and reduce volume – Have to work voluntarily to exhale • Bronchitis— inflammation of the bronchi – Creates site for infection and increases mucous 42 Disorders • Pneumonia— infection or inflammation of the alveoli • Tuberculosis (TB)— bacterial infection that destroys lung tissue and is replaced by non-elastic connective tissue 43 Disorders • Respiratory Distress Syndrome (RDS) – Lack of surfactant makes breathing difficult – Alveoli are sticking together – Occurs in infants • Pulmonary Embolism – blood clot obstructs circulation to lung tissue & tissue dies 44 Disorders • Respiratory Failure – Not enough O2 to maintain metabolism – Cannot eliminate enough CO2 – Caused by: • • • • Drugs Stroke CO poisoning Shock 45 Disorders • Colds and Flu— viral infections • Sudden Infant Death Syndrome (SIDS) – – – – Crib death Occurs between 1 week and 12 months Cause is unknown Baby stops breathing • Lung Caner: http://today.msnbc.msn.com/id/26184891/v p/36258056#36258056 46 Disorders • Laryngitis— vocal cords • Pharyngitis— sore throat • Rhinitis— lining of the nose 47 Effects of Aging • Vital capacity and maximum minute ventilation decrease • Residual volume and dead space increase • Ability to remove mucus from respiratory passageways decreases • Gas exchange across respiratory membrane is reduced 48