Acute Respiratory Distress Syndrome Heba Ismail, M.B.Ch.B Assistant Clinical Professor
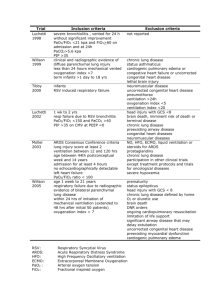
advertisement

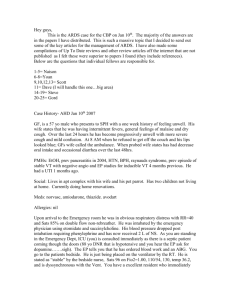
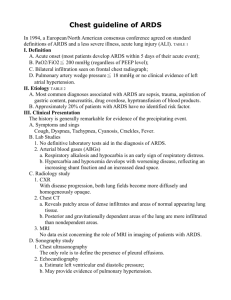
Acute Respiratory Distress Syndrome Heba Ismail, M.B.Ch.B Assistant Clinical Professor Division Of Pulmonary and Critical Care Medicine ARDS Objectives Updated definition of ARDS Briefly review Pathophysiology and Pathogenesis Etiology/Risk factors Clinical Presentation Diagnosis, Differential Diagnosis Management ARDS Case #1 A 70-year-old man was admitted to the ICU acute hypoxemic respiratory failure 48 hours earlier He underwent a surgical resection of the left lower lobe for stage IIIB adenocarcinoma of the lung. Intra-operative course He received a total fluid infusion of 5.5 L (including 3 units of packed red blood cells) The cumulative fluid infusion given during the peri-operative period was 8.0 L with a net negative 0.7L ARDS Case#1 Post Operative course Extubated and transferred to the ward 36 hours later dyspnea and hypoxemia were noted re-intubated ARDS Case#1 Past Medical History Adenocarcinoma of the lung, stage IIIb, diagnosed 3 months before surgery, treated with preoperative neo-adjuvant chemotherapy and radiotherapy History of moderate COPD Social History 80-pack-years of cigarette smoking chronic alcohol consumption of approximately 30g of ethanol per day. ARDS Case #1 Pre-operative evaluation Complete blood count and blood chemistry were normal Pre-operative evaluation for chronic heart disease was negative Forced Expiratory Volume in 1s (FEV1) was 1.79 L; 58% of the predicted value; calculated postoperative FEV1 was 49% of the predicted value ICU Admission Physical examination Vital signs, BP 100/70 mmHg, Pulse 120/min, Respirations 33/min, SpO2 of 85% on 100% Non rebreather, Temperature 37.0 C Cardiovascular S1, S2 normal Respiratory Decreased breath sounds over the left lower lung field, diffuse endinspiratory crackles over the remaining lobes . Laboratory Data Normal complete blood count and chemistry Blood and bronchoalveolar lavage (BAL) specimens were collected and sent for microbiologic analysis. Blood cultures, done Arterial blood gases: (on FiO2 0.6), PaO2 70mmHg,, PaCO2 45mmHg, HCO3 24, PaO2/ FiO2 117 CXR ARDS Case #1 What is your next diagnostic study? CT chest/PE Protocol Transthoracic Echocardiogram Right Cardiac Catheterization Repeat Bronchoscopy CT chest ARDS Case #1 Transthoracic echocardiography: Ejection fraction 60 %, normal left ventricular systolic function. Mild right ventricular dilation Right heart catheterization: Cardiac Output (CO): 7.74 L/min (normal 5-7 L/min) Cardiac Index (CI): 4.8 L/min/m2(normal 3-5 L/min/m2) CVP 8 mmHg SVRI: 960 dynes/sec/cm5/m2 (normal 1200-1800) Pulmonary artery systolic pressure (PASP): 59 mmHg Pulmonary Wedge Pressure: 11 mmHg ARDS Case #1 Which of the following statements is true: The Development of acute respiratory failure in this patient is due to: A. Pulmonary edema due to fluid overload B. Cardiogenic pulmonary edema due to left-sided heart failure C. Acute respiratory distress syndrome (ARDS) D. Pneumonia E. Massive pulmonary embolism The American-European Consensus Conference Definition of Acute Lung Injury and ARDS, AECC AECC Criticism From: Acute Respiratory Distress Syndrome: The Berlin Definition JAMA. 2012;307(23):2526-2533. doi:10.1001/jama.2012.5669 AECC Criticism, Hypoxemia Factors that affect PaO2/FiO2 vs FiO2 Cardiac output A-V O2 Difference Distribution of blood flow to different V/Q regions Low V/Q Shunt Oxygen consumption Hemoglobin concentration Effect of Intrapulmonary Shunt (S) and arterio-venous O2 Difference (AVD) on PaO2/FiO2 AECC Criticism, Hypoxemia AECC Criticism, Hypoxemia AECC Criticism, hypoxemia AECC Criticism, CXR AECC Criticism, CXR AECC Criticism, PCWP ARDS New Definition ARDS, New Definition ESICM convened an international panel of experts, with representation of ATS and SCCM The objectives were to update the ARDS definition using a systematic analysis of: current epidemiologic evidence physiological concepts results of clinical trials ARDS, New Definition All modifications were based on the principle that syndrome definitions must fulfill three criteria: Feasibility Reliability Validity Acute Respiratory Distress Syndrome The Berlin definition JAMA. 2012;307(23):2526-2533. doi:10.1001/jama.2012.5669 ARDS The Berlin Definition JAMA. 2012;307(23):2526-2533. doi:10.1001/jama.2012.5669 ARDS The Berlin Definition No change in the underlying conceptual understanding of ARDS “acute diffuse, inflammatory lung injury, leading to increased pulmonary vascular permeability, increased lung weight, and loss of aerated lung tissue…[with] hypoxemia and bilateral radiographic opacities, associated with increased venous admixture, increased physiological dead space, and decreased lung compliance.” Although the authors emphasize the increased power of the new Berlin definition to predict mortality compared to the AECC definition, in truth it’s still poor, with an area under the curve of only 0.577, (95% CI, 0.561-0.593) compared to 0.536, (95% CI, 0.520-0.553;P < 001 ) for the old definition. ARDS Pathophysiology ARDS Pathological Stages Initial "exudative" stage-diffuse alveolar damage within the first week “Proliferative" stage-resolution of pulmonary edema, proliferation of type II alveolar cells, squamous metaplasia, interstitial infiltration by myofibroblasts, and early deposition of collagen. Some patients progress to a third "fibrotic" stage, characterized by obliteration of normal lung architecture, diffuse fibrosis, and cyst formation ARDS Pathophysiology Risk Factors Sepsis Severe trauma Surface burns Multiple blood transfusions Drug overdose Following bone marrow transplantation Multiple fractures Aspiration Pneumonia Pulmonary contusion Pulmonary embolism Inhalational injury Near drowning Negative Pressure Pulmonary Edema Type of Non-Cardiogenic Pulmonary Edema Mechanism Rapid resolution of large levels of negative intra-thoracic pressures by removal of airways obstruction ------leads to alveolar and capillary damage -----leads to increased vascular permeability ARDS Clinical Presentation Dyspnea, Tachypnea Persistent hypoxemia, despite the administration of high concentrations of inspired oxygen Increase in the shunt fraction Decrease in pulmonary compliance Increase in the dead space ventilation Management of ARDS Basic Management Strategies for Patients with ALI/ARDS Identify and treat underlying causes Ventilatory support Lung protective ventilatory support strategy Application of PEEP Restore and maintain hemodynamic function Conservative fluid replacement strategy Vasopressors and inotropics support Prevent complications of critical illness Ensure adequate nutrition Avoid oversedation Using weaning protocol with spontaneous breathing trials Continous use of steroids for fibroproliferative phase ?questionable Fluid management and vasoactive support SAFE trial Resuscitation with saline is as beneficial as resuscitation with albumin in critically ill patients with shock FACTT trial Prospective, Randomized, Multi-Center Trial Utility and safety of using a pulmonary artery catheter versus central venous catheter to guide the volume replacement Liberal versus conservative fluid replacement ARDS FACTT Patients were treated with the specific fluid management strategy (to which they were randomized) for 7 days or until unassisted ventilation, whichever occurs first. The study enrolled 1000 patients and showed no benefit with PAC guided fluid therapy over the less invasive CVC guided therapy. ARDS FACTT The Use of Conservative fluid management strategy was associated with Significant improvement in oxygenation index Significant improvement in Lung Injury score increase in the number of ventilator- free days ARDS Mechanical Ventilation Ventilator associated lung injury Volutrauma Atelectotrauma Biotrauma Barotrauma Air embolism/translocation NHLBI ARDS Network Compared low tidal volumes (6ml/kg of ideal body weight ) against conventional tidal volumes (12ml/kg ideal body weight ) Significant decrease in mortality associated with the use of low tidal volumes (39.8% versus 31%, P= 0.007) NHLBI ARDS Network Improved Survival with Low VT NHLBI ARDS Network Main Outcome Variables NHLBI ARDS Network Main Organ Failure Free Days ARDS Mechanical Ventilation Initial tidal volumes of 8 mL/kg predicted body weight in kg, calculated by: [2.3 *(height in inches - 60) + 45.5 for women or + 50 for men]. Respiratory rate up to 35 breaths/min expected minute ventilation requirement (generally, 7-9 L /min) Set positive end-expiratory pressure (PEEP) to at least 5 cm H2O (but much higher is probably better) FiO2 to maintain an arterial oxygen saturation (SaO2) of 8895% (paO2 55-80 mm Hg). Titrate FiO2 to below 70% when feasible. Over a period of less than 4 hours, reduce tidal volumes to 7 mL/kg, and then to 6 mL/kg. ARDS Mechanical Ventilation ARDS Mechanical Ventilation Plateau pressure (measured during an inspiratory hold of 0.5 sec) less than 30 cm H2O, High plateau pressures vastly elevate the risk for harmful alveolar distension ( volutrauma). If plateau pressures remain elevated after following the above protocol, further strategies should be tried: Reduce tidal volume, to as low as 4 mL/kg by 1 mL/kg stepwise increments. Sedate the patient to minimize ventilator-patient dyssynchrony. Consider other mechanisms for the increased plateau pressure Potential benefits of hypercapnia in patients with ARDS Decrease in TNF-alpha release by alveolar macrophages Decrease in PMNL-endothelial cell adhesion Decrease in Xanthine oxiedase activity Decrease in NOS activity Reduction of IL-8 ARDS High versus Low PEEP Higher PEEP along with low tidal volume ventilation should be considered for patients receiving mechanical ventilation for ARDS. This suggestion is based on a 2010 meta-analysis of 3 randomized trials (n=2,229) testing higher vs. lower PEEP in patients with acute lung injury or ARDS, in which ARDS patients receiving higher PEEP had a strong trend toward improved survival. ARDS High versus Low PEEP However, patients with milder acute lung injury (paO2/FiO2 ratio > 200) receiving higher PEEP had a strong trend toward harm in that same metaanalysis. Higher PEEP can conceivably cause ventilatorinduced lung injury by increasing plateau pressures, or cause pneumothorax or decreased cardiac output. These adverse effects were not noted in the largest ARDSNet trial (2004) testing high vs. low PEEP. ARDS Mechanical Ventilation ARDS Mechanical Ventilation ARDS Mechanical Ventilation Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med, 2010;363:1107-16. This multicenter RCT of 340 patients with severe ARDS found early use of 48 hours of neuromuscular blockade reduced mortality compared to placebo (NNT of 11 to prevent one death at 90 days in all patients, and a NNT of 7 in a prespecified analysis of patients with a PaO2:FiO2 less than 120). Basic management Strategies for patients with ALI/ARDS Identify and treat underlying causes Ventilatory support Lung protective ventilatory support strategy Application of PEEP Restore and maintain hemodynamic function Conservative fluid replacement strategy Vasopressors and inotropics support Prevent complications of critical illness Ensure adequate nutrition Avoid oversedation Using weaning protocol with spontaneous breathing trials Continous use of steroids for fibroproliferative phase,?questionable CASE #1 On admission to the ICU, the patient was sedated and placed on volume control mechanical ventilation with the follow settings: FiO2: 0.6, VT: 450 ml, RR:18, PEEP:10 cm H2O, VΕ:8 L/min. Additional supportive therapy included initial, empiric, broadspectrum antibiotics and restrictive fluid management. On Day 3, due to further impairment of oxygenation (SaO2 <80%) that did not improve with increases in both PEEP and FiO2, the patient was placed on high frequency oscillatory ventilation. Although he had an initial improvement in oxygenation, his overall condition continued to decline and he died on Day 5 due to multiple organ failure. ARDS Inhaled NO Steroids Prone Position High Frequency Oscillatory Ventilation ECMO Inhaled Nitric Oxide It is a bronchial and vascular smooth muscle dilator Decreases the Platelets Adherence and Aggregation Improves Ventilation –Perfusion ratio Reduction in Pulmonary Artery Pressure and pulmonary Vascular Resistance Inhaled Nitric Oxide Two Prospective, Randomized, Placebo Controlled Clinical Trials failed to demonstrate an improvement in the survival. However, there was improvement in the oxygenation… ARDS Steroid A protocol for steroids in late ARDS, based on the Meduri paper* The patient must have no demonstrable infection broncho-alveolar lavage may be necessary to confirm this. This includes undrained abscesses, disseminated fungal infection and septic shock Steroids should not be started less than 7 days, or more than 28 days, from admission The patient should not have a history of gastric ulceration of active gastrointestinal bleeding Patients with burns requiring skin grafting, pregnant patients, AIDS, and those in whom life support is expected to be withdrawn, are unsuitable *Meduri GU, Kohler G, Headley S, Tolley E, Stentz F, Postlethwaite A. Inflammatory cytokines in the BAL of patients with ARDS. Persistent elevation over time predicts poor outcome. Chest 1995; 108(5):1303-1314. (2) Meduri GU, Headley AS, Golden E, Carson SJ, Umberger RA, Kelso T et al. Effect of prolonged methylprednisolone therapy in unresolving acute respiratory distress syndrome: a randomized controlled trial. JAMA 1998; 280(2):159-165. ARDS Steroids The patient should have evidence of ARDS and require an FiO2 >/= 50% The steroid regimen: Loading dose 2mg/kg Then 2mg/kg/day from day 1 to 14 Then 1mg/kg/day from day 15 to 21 Then 0.5mg/kg/day from day 22 to 28 Then 0.25mg/kg/day on days 29 and 30 Finally 0.125mg/kg on days 31 and 32. Prone Positioning Relieves the cardiac and abdominal compression exerted on the lower lobes Makes regional Ventilation/Perfusion ratios and chest elastance more uniform Facilitates drainage of secretions Potentiates the beneficial effect of recruitment maneuvers Study Overview • Placing patients who require mechanical ventilation in the prone rather than the supine position improves oxygenation. • In this trial, the investigators found a benefit with respect to all-cause mortality with this change in body position in patients with severe ARDS. Enrollment, Randomization, and Follow-up of the Study Participants. Guérin C et al. N Engl J Med 2013;368:2159-2168 Characteristics of the Participants at Inclusion in the Study. Guérin C et al. N Engl J Med 2013;368:2159-2168 Ventilator Settings, Respiratory-System Mechanics, and Results of Arterial Blood Gas Measurements at the Time of Inclusion in the Study. Guérin C et al. N Engl J Med 2013;368:2159-2168 Kaplan–Meier Plot of the Probability of Survival from Randomization to Day 90. Guérin C et al. N Engl J Med 2013;368:2159-2168 Primary and Secondary Outcomes According to Study Group. Guérin C et al. N Engl J Med 2013;368:2159-2168 Conclusions • In patients with severe ARDS, early application of prolonged pronepositioning sessions significantly decreased 28-day and 90-day mortality. Vent settings to improve oxygenation PEEP and FiO2 are adjusted in tandem • FIO2 • Simplest maneuver to quickly increase PaO2 • Long-term toxicity at >60% • Free radical damage • Inadequate oxygenation despite 100% FiO2 usually due to pulmonary shunting • Collapse – Atelectasis • Pus-filled alveoli – Pneumonia • Water/Protein – ARDS • Water – CHF • Blood - Hemorrhage Vent settings to improve oxygenation PEEP and FiO2 are adjusted in tandem • PEEP • Increases FRC • Prevents progressive atelectasis and intrapulmonary shunting • Prevents repetitive opening/closing (injury) • Recruits collapsed alveoli and improves V/Q matching • Resolves intrapulmonary shunting • Improves compliance • Enables maintenance of adequate PaO2 at a safe FiO2 level • Disadvantages • Increases intrathoracic pressure (may require pulmonary a. catheter) • May lead to ARDS • Rupture: PTX, pulmonary edema Oxygen delivery (DO2), not PaO2, should be used to assess optimal PEEP. Vent settings to improve ventilation Respiratory rate Max RR at 35 breaths/min Efficiency of ventilation decreases with increasing RR Decreased time for alveolar emptying TV Goal of 10 ml/kg Risk of volutrauma Other means to decrease PaCO2 Reduce muscular activity/seizures Minimizing exogenous carb load Controlling hypermetabolic states Permissive hypercapnea Preferable to dangerously high RR and TV, as long as pH > 7.15 Vent settings to improve ventilation RR and TV are adjusted to maintain VE and PaCO2 • Respiratory rate • Max RR at 35 breaths/min • Efficiency of ventilation decreases with increasing RR • Decreased time for alveolar emptying • TV • Goal of 10 ml/kg • Risk of volutrauma • Other means to decrease PaCO2 • Reduce muscular activity/seizures • Minimizing exogenous carb load • Controlling hypermetabolic states • Permissive hypercapnea • Preferable to dangerously high RR and TV, as long as pH > 7.15 • PIP • Elevated PIP suggests need for switch from volume-cycled to pressure-cycled mode • I:E ratio (IRV) • Increasing inspiration time will increase TV, but may lead to auto-PEEP • Maintained at <45cm H2O to minimize barotrauma • Plateau pressures • Pressure measured at the end of inspiratory phase • Maintained at <30-35cm H2O to minimize barotrauma Origins of mechanical ventilation The era of intensive care medicine began with positive-pressure ventilation • Negative-pressure ventilators (“iron lungs”) • Non-invasive ventilation first used in Boston Children’s Hospital in 1928 • Used extensively during polio outbreaks in 1940s – 1950s • Positive-pressure ventilators The iron lung created negative pressure in abdomen as well as the chest, decreasing cardiac output. • Invasive ventilation first used at Massachusetts General Hospital in 1955 • Now the modern standard of mechanical ventilation Iron lung polio ward at Rancho Los Amigos Hospital in 1953.