Oxygenation
advertisement
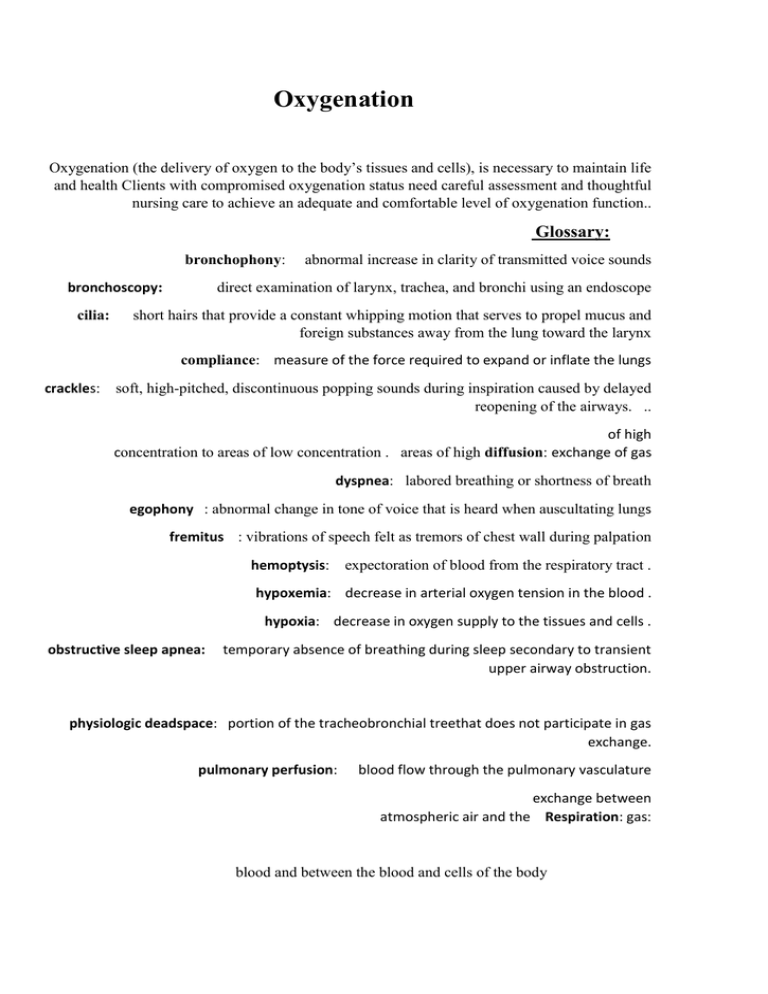
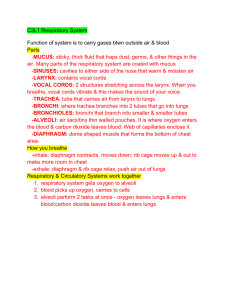
Oxygenation Oxygenation (the delivery of oxygen to the body’s tissues and cells), is necessary to maintain life and health Clients with compromised oxygenation status need careful assessment and thoughtful nursing care to achieve an adequate and comfortable level of oxygenation function.. Glossary: bronchophony: bronchoscopy: cilia: abnormal increase in clarity of transmitted voice sounds direct examination of larynx, trachea, and bronchi using an endoscope short hairs that provide a constant whipping motion that serves to propel mucus and foreign substances away from the lung toward the larynx compliance: measure of the force required to expand or inflate the lungs crackles: soft, high-pitched, discontinuous popping sounds during inspiration caused by delayed reopening of the airways. .. of high concentration to areas of low concentration . areas of high diffusion: exchange of gas dyspnea: labored breathing or shortness of breath egophony : abnormal change in tone of voice that is heard when auscultating lungs fremitus : vibrations of speech felt as tremors of chest wall during palpation hemoptysis: expectoration of blood from the respiratory tract . hypoxemia: decrease in arterial oxygen tension in the blood . hypoxia: decrease in oxygen supply to the tissues and cells . obstructive sleep apnea: temporary absence of breathing during sleep secondary to transient upper airway obstruction. physiologic deadspace: portion of the tracheobronchial treethat does not participate in gas exchange. pulmonary perfusion: blood flow through the pulmonary vasculature exchange between atmospheric air and the Respiration: gas: blood and between the blood and cells of the body Rhonchi: low-pitched wheezing or snoring sound associatedwith partial airway obstruction, heard on chest auscultation Tridor: harsh high-pitched sound heard on inspiration, usually without need of stethoscope, secondary to upper airway obstruction .. Tachypnea: abnormally rapid respirations Tidal volume: volume of air inspired and expired with eachbreath during normal breathing Ventilation: Wheezes: movement of air in and out of airways continuous musical sounds associated with airway narrowing or partial obstruction. Apnea: temporary cessation of breathing. Anatomy and physiology of Respiration: Normal functioning depends on essentially three factors: m to transport air to and from the lungs.Integrity of the airway . 1- -A properly functioning alveolar system remove Co2 from the bloodoxygenatevenous bloodlungs . 2 3-A properly functioning cardiovascular and hematologic system to carry nutrients and wastes to and from body cells. Structures of the Respiratory System: The airway, which begins at the: - -nose, pharynx, larynx, epiglottis ,tracheobronchial tree, includes the trachea, right and left main stem bronchi, segmental bronchi, and terminal bronchioles, at the end of the terminal bronchioles there are clusters of alveoli( singular, alveolus), small air sacs. The lungs and thoracic cavity are lined with a serious membrane called the pleural. The pleural space lies between the two layers, pleural fluid between the membranes acts a lubricant and as an adhesive agent to hold the lungs in an expanded position. A milliliter of fluid between the pleural surfaces allows the lungs to more easily along the chest wall as they expand and contract. Without this fluid, filling and emptying of the lungs are difficult. Pressure within the pleural space (intrapleural pressure) is always sub atmospheric (a negative pressure). This constant negative intrapleural pressure , along with the pleural fluid holds the lungs in an expanded position . Physiology of the Respiratory system : Living cells require oxygen and the removal of carbon dioxide a byproduct of oxidation. Gas exchange, the intake of oxygen and the release of carbon dioxide, is made possible by pulmonary ventilation, respiration, and perfusion. Pulmonary Ventilation and Regulation of Respiration: The first step in the process of oxygenation is ventilation, which is the movement of air into and out of the lungs for the purpose of delivering fresh air into the lung's alveoli. Ventilation is regulated by respiratory control centers in the Pons and medulla oblongata, which are located in the brain stem. The rate and depth of ventilation are constantly adjusted in response to changes in the concentrations of hydrogen ion (pH) and carbon dioxide (CO2) in the body’s fluids. For instance, an increase in carbon dioxide in the blood or a decrease in pH in the body’s fluids will stimulate faster and deeper ventilation. A decrease in blood oxygen concentration (hypoxemia) will also stimulate ventilation, but to a lesser degree. Inhalation of air is initiated when the diaphragm contracts, pulling it downward and thus increasing the size of the intrathoracic space this space is also increased by contraction of the external intercostals muscles, which elevate and separate the ribs and move the sternum forward. The effect of increasing the space inside the thorax is to decrease the intrathoracic pressure, so that air will be drawn in from the atmosphere. Stretch receptors in the lung tissue send signals back to the brain to cause cessation of inhalation, preventing over distension of the lungs. Exhalation occurs when the respiratory muscles relax, thus reducing the size of the intrathoracic space, increasing the intrathoracic pressure, and forcing air to exit the lungs. Under normal conditions, exhalation is a passive process. When the movement of air is impeded, additional muscles may be used to increase the ventilatory ability. These accessory muscles of ventilation include the sternocleidomastoid muscle, the abdominal muscles, and the internal intercostals muscles. In some disease states exhalation is impaired, requiring that the individual actively force air out of the lungs rather than passively exhaling. Forced expiration is aided by the intercostals muscles and the abdominal recti. When additional muscular force is required for breathing, the work of breathing is said to be increased. Microorganisms and debris. As air is inhaled through the nose, the larger particles are filtered out through hairs lining the nasal passages. Several mechanisms exist to keep the airways clear of microorganisms and debris. As air is inhaled through the nose, the larger particles are filtered out through hairs lining the nasal passages. The mucous membranes of the nasopharynx and sinuses warm and humidify the inspired air, and the film of mucus lining these membranes traps smaller particles. Closure of the glottis protects the airway from aspiration of food and fluids during swallowing. In the trachea and larger bronchi, tiny hair like cilia continually produce wavelike movements to propel mucus and particles upward, where they can be coughed out. If any invaders manage to reach the alveoli, specialized alveolar macrophages will engulf and destroy the offending organism. Respiration: Once fresh air reaches the lung’s alveoli, the next step in the process of oxygenation begins. The exchange of oxygen from the alveolar space into the pulmonary capillary blood is referred to as oxygen uptake; it may also be called external respiration. Oxygen diffuses across the alveolar membrane in response to a concentration gradient; that is, it moves from an area of higher concentration (the alveoli) to an area of lower concentration (the pulmonary capillary blood), seeking equilibrium. At the same time, carbon dioxide diffuses from the blood to the alveolar space, also in response to a concentration gradient . Gas exchange occurs via diffusion. Diffusion is the movement of gas or particles from areas of higher pressure or concentration to areas of lower pressure or concentration. Diffusion refers to the movement of oxygen and carbon dioxide between the air (in the alveoli) and blood ( in the capillaries). The greater pressure of oxygen in the alveoli causes the oxygen to move from the alveoli into the capillaries containing the un oxygenated venous blood. The carbon dioxide in the returning venous blood exerts a greater pressure then the carbon dioxide in the alveoli. Diffusion of gases in the lung is influenced by four factors: 1. Change in surface area available 2. Thickening of alveolar- capillary membrane 3. Partial pressure 4. Solubility and molecular weight of the gas Perfusion: Oxygenated capillary blood passes through the tissues of the body in the process called perfusion . The amount of blood flowing through the lungs is a factor in the amount of oxygen and other gases that are exchanged. The perfusion of the lung tissue also dependent s on the person's activity level. Greater activity results in an increased need for cellular oxygen by the body's tissues and a subsequent increase in cardiac output and consequently in increased blood return to the lungs. If a problem exists in ventilation, respiration, or perfusion, hypoxia may occur. The most common symptoms of hypoxia are dyspnea (difficulty breathing). Hypoxia is often caused by hypoventilation (decreased rate or depth of air movement into the lungs). Hypoxia can also be a chronic condition. The effects of chronic hypoxia can be detected in all body systems and are manifested as altered thought processes, headaches, chest pain, enlarged heart, clubbing of the fingers and toes, muscle pain. The Cardiovascular System and Transport of Respiration Gases. Once oxygen is bound to hemoglobin, the oxygen is delivered to the cells of the body by the process of circulation. Circulation of the blood is the function of the heart and blood vessels. The heart is a muscular pump that is divided into four chambers: the right and left atria and the right and left ventricles. A series of valves allows for unidirectional blood flow through the chambers, which is driven by the sequential contraction and relaxation of the heart muscle A single cycle of atrial and ventricular contraction and relaxation is referred to as a cardiac cycle, which is the product of the interplay of electrical and mechanical events. The electrical activity of the heart involves the generation and transmission of electrical current by specialized cardiac cells known as the cardiac conduction A small mass of cells in the right atrium, the sinoatrial node, or SA node, normally controls the heart rate by rhythmically generating electrical impulses. For this reason, the SA node is often referred to as the heart’s “pacemaker.” The impulses created by the SA node travel along specialized internodal pathways to spread throughout the atria, resulting in mechanical muscular contraction. The electrical activity is then transmitted down to the entricles via the atrioventricular (AV) node and spreads through the ventricular tissue along the bundle of His, right and left bundle branches, and Purkinje fibers. Again, the result is muscular contraction. The sequential contraction and relaxation of the atria and ventricles is an essential factor in the cyclical filling and emptying of the chambers, which produce circulation. The process of chamber filling is referred to as diastole, and the process of a chamber emptying is systole. Atrial diastole occurs as the right and left atria relax and blood flows into the right and left atrial chambers from the venae cavae and pulmonary veins, respectively. Filling of the ventricles causes the intraventricular pressure to rise. When the intraventricular pressure exceeds the pressure in the atria, the atrioventricular valves close. The ventricular muscle then begins to contract, further increasing intraventricular pressure until it is sufficient to force open the two semilunar valves (the pulmonic and aortic valves). As contraction of the ventricular walls proceeds, blood is forced out of the ventricles and into the circulation (ventricular systole). Blood leaving the right ventricle is pumped into the pulmonary artery, which quickly branches into right and left pulmonary arteries. Further division of the pulmonary arterial tree culminates in the pulmonary capillary bed. Blood in the pulmonary capillaries is in very close contact with the alveolar air; it is here that alveolar-capillary gas exchanges take place. From the pulmonary capillaries, the freshly oxygenated blood flows into the pulmonary veins and to the left atrium, which delivers it to the left ventricle. Blood leaving the left ventricle enters the aorta. The aorta serves as the “trunk” of the arterial tree, with branches leading to every organ and tissue group in the body. Blood flow through the arterial system is driven by the pressure generated during ventricular systole and is influenced by the volume and viscosity of the blood and the amount of resistance within the arterial system. Blood flow to specific organs and tissues may be increased or reduced by the relaxation or contraction of precapillary sphincters, which are rings of smooth muscle surrounding the arterioles. This mechanism allows for redistribution of blood flow to the areas of greatest need, a process known as autoregulation. Blood return through the venous system is also driven by pressure gradients, although the venous system. Temoperates under lower pressure than the arterial system does. In order to boost venous return, many veins (particularly in the lower extremities) are equipped with valves that prevent backward flow of blood (regurgitation); as the veins are compressed by their surrounding skeletal muscles, blood is forced along toward the vena cava and ultimately to the right atrium. -Factors affecting Respiratory Functioning: Adequate oxygenation is influenced by many factors, including: 1. Level of Health: acut and chronic illnesses can a persons respiratory function dramatically. For example people with renal or cardiac disorders often have compromised respiratory functioning because of fluid overload and impaired tissue perfusion. There are many disease states that may affect oxygenation, including obstructive pulmonary disease, restrictive pulmonary disease, diffusion defects, ventilation-perfusion mismatching, atherosclerosis, heart failure, anemia, and alterations in oxygen uptake. 2- Developmental considerations: There are many age-related developmental considerations affecting respiratory function. 1. Neonates and infants: 2. Toddlers, Preschoolers ,School-aged chlidren, and Adolescents. 3. Older Adults 3-Medications: Many medications affect the function of the respiratory system . Patients receiving drugs that affect the central nervous system need to be monitored carefully for respiratory complications. e.g. opioids are chemical agents that depress medullary respiratory center . As a result, the rate and depth of respirations decrease . Be alert for the possibility of respiratory depression or arrest when adeministering any narcotic or sedative . 4-Life style and Environmental Factors: Environmental and lifestyle factors can significantly affect a client’s oxygenation status. Clients who are exposed to dust, animal dander, asbestos, or toxic chemicals in the home or workplace are at increased risk for alterations in oxygenation. Individuals who experience significant physical or emotional stress or who are obese or underweight are also subject to changes in oxygenation status. Smokers and those exposed to second-hand smoke should be questioned as to the type and amount of tobacco and number of years of exposure. 5-Psychological Health; Many psychological factors and conditions can affect the respiratory system . Individuals responding to stress may sigh excessively or exhibit hyperventilation ( increased rate and depth of ventilation, above the bodys normal metabolic requirements). Hyperventilation can lead to lowered level of arterial carbon dioxide. Generalized anxiety has been shown to cause enough bronchospasm to produce an episode of bronchial asthma. In additional , patients with respiratory problems often develop some anxitey as a result of the hypoxia caused by the respiratory problem. The Nursing Process For Oxygenation: *-Assessing *- Nursing History *-Physical Assessment *-Common diagnostic Tests: 1-Pulmonary function studies 2-Spirometry 3-Pulse oximetry 4-Thoracentesis 5-Blood Gases: - pH: - PCO2: - HCO3:: − -PaO2 SaO2: 7.35–7.45 35–45 mm Hg 22–26 mEq/L 80–100 mm Hg 96%–98% *-Diagnosing : Nursing diagnoses indicating alterations in respiratory function are : 1. 2. 3. Ineffective Air way Clearance: when the client has difficulty maintaining a patent (open) airway at any point along the airway. This occlusion of the airway may be partial or complete. Ineffective Breathing Pattern: is commonly a problem for clients with restrictive pulmonary disease or central nervous system disorders that affect breathing. This respiratory pattern does not deliver adequate fresh air to the alveoli, resulting in chronic air hunger while contributing to muscle fatigue. Central nervous system disorders, including the effects of anesthetics and narcotics, may reduce both the rate and the depth of ventilation Impaired Gas Exchange: occurs when, despite the delivery of fresh air to the alveoli, adequate oxygen does not enter the arterial blood and/or carbon dioxide is not removed from the venous blood. e.g. emphysema , atelectasis (alveolar collapse) and pneumonia -Outcome Identification and Planning* The patient will: 1. -Demonstrate improved gas exchange in the lungs by an absence of cyanosis or chest pain and a pulse oximetry reading more than 95%. Relative the causative factors.Preserve pulmonary function by maintaining an optimal level of activity.- -Demonstrate self-care behaviors that provide relief from symptoms and prevent further pulmonary problems. Implementing:* Oxygen deficits, particularly in older people, impair all aspects of daily living. Nursing interventions related to oxygenation aim to: Promote optimal functioning of the respiratory system maintaining good nutrition, reducing anxiety, teaching about pollution-free environments.-To promote comfort, and to promote and control coughing : positioning, maintaining adequate fluid intake, providing humidified air, promoting proper breathing, deep breathing. -Nurses may also need to intervene by performing chest physiotherapy: percussion and vibrating, providing postural drainage) -suctioning the airway ,(suctioning irritates the mucosa and removes oxygen from respiratory tract, possibly causing hypoxemia, thus important to pre-oxygenate the patient before suctioning .This is accomplished by applying or increasing supplemental oxygen and having the patient take several deep breaths before inserting the catheter.) -Meeting respiratory needs with medications,: Many of the drugs used to dilate bronchial airways interact with caffeine. Encourage patients to avoid caffeine, which may potentiate the side affect of bronchodilators. - providing supplemental oxygen, sources of oxygen, oxygen flow rate measured Liters per minute, Humidification: because O2 dries and dehydrates the respiratory mucous membranes, supplying about 20%- 40% humidity are commonly used when oxygen is delivered at higher flow rates. Distilled or sterile water is commonly used to humidify oxygen. -Oxygen delivery systems: Nasal cannula, nasopharyngeal catheter, Face masks, Oxygen Tent Managing chest tubes,Using artificial airways, clearing an obstructed airway.The oral airway is used to maintain the tongue away from the posterior oropharynx in the unconscious client. It is essential to choose the correct size, since an airway that is too large may actually cause occlusion, while one that is too small may compress the tongue, stimulating the vomiting center. Endotracheal tubes bypass the upper airway structures altogether; they may be inserted via the nose or mouth and are passed beyond the vocal cords into the trachea. An inflatable cuff near the distal end of the tube serves to seal off the airway, allowing for mechanical ventilatory assistance and protecting the airway from aspiration . . Types of Artificial Airways clearing an obstructed airway: -Disease Processes Oxygenation alterations can often be traced to disease states related to alterations in ventilation, alveolar gas exchange, oxygen uptake, or circulation. There are many disease states that may affect oxygenation, including obstructive pulmonary disease, restrictive pulmonary disease, diffusion defects, ventilation-perfusion mismatching, atherosclerosis, heart failure, anemia, and alterations in oxygen uptake -Atherosclerosis Alterations in systemic circulation may also be generalized or localized. A common cause of altered arterial circulation is atherosclerosis. This disease is characterized by narrowing and eventual occlusion of the lumen (opening of the arteries) by deposits of lipids, fibrin, and calcium on the interior walls of the arteries. The reduction in blood flow with accompanying oxygen deprivation leads to ischemia (deprivation of blood flow) and eventual infarction (necrosis or death) of the affected tissue. -Anaerobic Metabolism The utilization of food (glucose) for cellular energy occurs via metabolic pathways that use oxygen; this is known as aerobic metabolism. Many cells are also capable of utilizing alternate metabolic pathways in the absence of oxygen for short periods of time. -Heart Failure Generalized decreases in tissue perfusion may be caused by left-sided heart failure or by loss of circulating blood volume- as may occur with shock or hemorrhage. Heart failure is a condition in which the heart is unable to pump enough blood to meet the metabolic needs of the body; typically, this is accompanied by a backup of blood in the venous circuits (pulmonary and systemic veins), leading to the condition known as congestive heart failure. -Anemia Another factor that influences oxygenation is the amount of hemoglobin in the blood available to bind with oxygen. A deficiency of hemoglobin (anemia) may decrease the oxygen-carrying capacity of the blood. Person who is anemic may have normal SaO2 levels but still continue to experience inadequate tissue oxygenation at the cellular level.