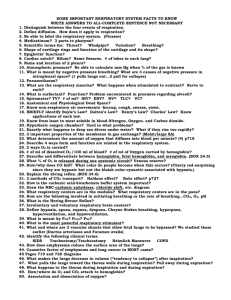
Week 5 Oxygenation and Tissue Perfusion
advertisement

Week 5 Oxygenation and Tissue Perfusion Learning Objectives 1. Describe and list factors that affect oxygenation and tissue perfusion. 2. Explain common physical assessment procedures used to evaluate respiratory health of patients across the lifespan. 3. Identify priority respiratory assessment findings. 4. Differentiate normal respiratory assessment from abnormal findings. Learning Objectives (cont’d.) 5. Describe the integral relationship between perfusion and oxygenation. 6. Explain the role and limitations associated with pulse oximetry assessment. 7. Explain and utilize vital signs and peripheral vascular assessment techniques and findings to assess perfusion. Oxygenation • Definitions • Oxygenation: mechanisms that facilitate or impair body’s ability to supply oxygen to cells • Respiration : act of inhaling and exhaling air to transport oxygen to alveoli • So oxygen may be exchanged for carbon dioxide • Carbon dioxide expelled from body • Ventilation : actual exchange of oxygen and carbon dioxide (Breathing) Definitions (cont’d) • Diffusion- The movement of a substance from an area of high concentration to an area of low concentration (Gas exchange). • Perfusion – A continuous supply of oxygenated blood to every cell in the body (Pumped to all parts). Three main components/concepts to oxygenation of the body: •Ventilation – Breathing •Diffusion- Gas exchange •Perfusion – pumped to all parts Normal Presentation: • Adequate Oxygenation: – Depends on healthy intact respiratory system – Upper respiratory system • Inlet for air into body • Inlet typically nose • Breathing also through mouth Ventilation: The exchange of oxygen and carbon dioxide. (Air moving in and out of the lungs.) Average Respiratory Rates: *Infants: About 30 breaths per minute *Preschooler: Around 25 breaths per minute *Adolescents & Adults: 12- 18 breaths per minute Hypoxemia: Decreased level of oxygen First signs of hypoxia may include: Anxiety, restlessness, and/or confusion Cyanosis: Late sign of hypoxemia and is seen as a blue tinge to the skin Cyanosis is a late sign of hypoxemia Impaired Oxygenation: Can be life-threatening Mild to severe Diseases, injuries Frightening, frustrating Assessment: What do you see? (Examples include restlessness, anxiety, gasping, cyanosis, shortness of breath, increased respiratory rate?) Assessment: What do you hear? (With your ears and/or with your stethoscope…) Normal breath sounds are the inspiratory and expiratory sounds heard through the chest wall of a healthy individual. Do you hear coughing, wheezing, gasping, or any other sounds during breathing? Q. Ventilation is also known as _______? a. Wheezing b. Pneumonia c. Breathing d. Lung Abscess c. Breathing Quality of breathing requires a patent airway, one that is open and free of obstruction. A priority for the nurse is to always make certain the patient has a patent airway! Airway patency is a priority with patient status changes, facial/dental surgery, upper respiratory tract obstruction, and emergency situations! Swollen Tongue: Definitely an airway issue since this affects ventilation! When edema and swelling of the trachea/airway occur in response to a virus, bacterium, or other irritant, the airway is further narrowed. Think of diffusion as oxygen getting into the blood and carbon dioxide getting out… (Remember: gas exchange.) * Hemoglobin is the oxygen-carrying molecule within the red blood cells (RBC’s). * No RBC’s or hemoglobin; no oxygen! * Pulse Oximeter measures percentage of oxygen attached to hemoglobin Oxygen Saturation: Pulse Oximeter is used to measure the percentage of oxygen attached to hemoglobin When assessing respiratory status changes, determine if the patient is… *Short of breath and/or in respiratory distress? *Involved in or just completing physical activity or exertion causing increased respiratory rate (P.T. or up to the bathroom)? *Is pulse ox is attached properly and turned on? *Are they comfortable only when sitting upright and slightly forward with legs down? (See next slide) Tripod Position: Leaning forward with the hands on the knees Q. What is the first thing you do when someone has difficulty breathing? a. Have them raise their feet b. Sit them up in high upright position c. Give them water to drink d. Take their blood pressure b. Sit them in an upright position End of Week 5