Campylobacter & Helicobacter Campylobacter : -
advertisement

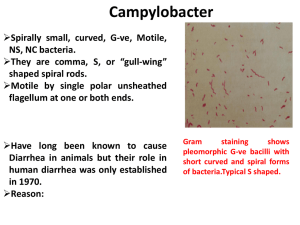
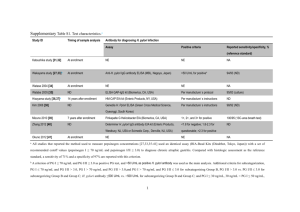
Campylobacter & Helicobacter 1 Campylobacter & Helicobacter Campylobacter and Helicobacter species are gram-negative rods that are all widely distributed in nature. The campylobacters are found in many species of animals. Campylobacter : - Campylobacters cause both diarrheal and systemic diseases and are among the most widespread causes of infection in the world. Campylobacter jejuni & Campylobacter coli Campylobacter jejuni and Campylobacter coli have emerged as common human pathogens, causing mainly enteritis and occasionally systemic infection. C jejuni and C coli cause infections that are clinically indistinguishable, and laboratories generally do not differentiate between the two species. C jejuni and the other campylobacters are gram-negative rods with comma, S, or "gull-wing" shapes. They are motile, with a single polar flagellum, and do not form spores. Antigenic Structure & Toxins The campylobacters have lipopolysaccharides with endotoxic activity. Cytopathic extracellular toxins and enterotoxins have been found. Pathogenesis & Pathology - The infection is acquired by the oral route from food, drink, or contact with infected animals or animal products. - C jejuni is susceptible to gastric acid, and ingestion of about 104 organisms is usually necessary to produce infection. - The organisms multiply in the small intestine, invade the epithelium, and produce inflammation that results in the appearance of red and white blood cells in the stools. - Occasionally, the bloodstream is invaded and a clinical picture of enteric fever develops. Localized tissue invasion coupled with the toxic activity appears to be responsible for the enteritis. 1 Campylobacter & Helicobacter 2 Clinical Findings: - Clinical manifestations are acute onset of :- crampy abdominal pain, profuse diarrhea that may be grossly bloody, headache, malaise, and fever. - Usually the illness is self-limited to a period of 5–8 days, but occasionally it continues longer. Diagnostic Laboratory Tests Specimens: - Diarrheal stool is the usual specimen. Smears: - Gram-stained smears of stool may show the typical "gull wing"-shaped rods. Dark-field or phase contrast microscopy may show the typical darting motility of the organisms. Culture: - Selective media are needed, and incubation must be in an atmosphere with reduced O2 (5% O2) with added CO2 (10% CO2). A relatively simple way to produce the incubation atmosphere is to place the plates in an anaerobe incubation jar without the catalyst and to produce the gas with a commercially available gasgenerating pack or by gas exchange. - Incubation of primary plates for isolation of C jejuni should be at 42 °C, incubation at 42 °C prevents growth of most of the other bacteria present in feces. - Several selective media are: Skirrow's medium contains vancomycin, polymyxin B, and trimethoprim to inhibit growth of other bacteria. Other selective media also contain antimicrobials, including cephalothin or cefoperazone, and inhibitory compounds. The colonies tend to be colorless or gray. They may be watery and spreading or round and convex, and both colony types may appear on one agar plate. Epidemiology & Control Campylobacter enteritis resembles other acute bacterial diarrheas, particularly Shigella dysentery. The source of infection may be food (eg, milk, undercooked fowl) or contact with infected animals or 2 Campylobacter & Helicobacter 3 humans and their excreta. Outbreaks arising from a common source, eg, unpasteurized milk may require public health control measures. Helicobacter pylori Helicobacter pylori is a spiral-shaped gram-negative rod. H. pylori is associated with antral gastritis, duodenal (peptic) ulcer disease, gastric ulcers, and gastric carcinoma. Other Helicobacter species that infect the gastric mucosa exist but are rare. H pylori has many characteristics in common with campylobacters. It is motile, and is a strong producer of urease. Pathogenesis & Pathology - H pylori grows optimally at a pH of 6.0–7.0 and would be killed or not grow at the pH within the gastric lumen. Gastric mucus is relatively impermeable to acid and has a strong buffering capacity. On the lumen side of the mucus, the pH is low (1.0–2.0) while on the epithelial side the pH is about 7.4. H pylori is found deep in the mucous layer near the epithelial surface where physiologic pH is present. - H pylori also produces a protease that modifies the gastric mucus and further reduces the ability of acid to diffuse through the mucus. - H pylori produces potent urease activity, which yields production of ammonia and further buffering of acid. - H pylori is quite motile, even in mucus, and is able to find its way to the epithelial surface. H pylori overlies gastric-type but not intestinal-type epithelial cells. - In human volunteers, ingestion of H pylori resulted in development of gastritis and hypochlorhydria. There is a strong association between the presence of H pylori infection and duodenal ulceration. Antimicrobial therapy results in clearing of H pylori and improvement of gastritis and duodenal ulcer disease. - Toxins and lipopolysaccharide may damage the mucosal cells, and the 3 Campylobacter & Helicobacter 4 ammonia produced by the urease activity may directly damage the cells also. - Histologically, gastritis is characterized by chronic and active inflammation. Polymorphonuclear and mononuclear cell infiltrates are seen within the epithelium and lamina propria. Vacuoles within cells are often pronounced. Destruction of the epithelium is common, and glandular atrophy may occur. H pylori thus may be a major risk factor for gastric cancer. Clinical Findings Acute infection can yield an upper gastrointestinal illness with nausea and pain; vomiting and fever may be present also. The acute symptoms may last for less than 1 week or as long as 2 weeks. Once colonized, the H pylori infection persists for years and perhaps decades or even a lifetime. About 90% of patients with duodenal ulcers and 50–80% of those with gastric ulcers have H pylori infection. H pylori also may have a role in gastric carcinoma and lymphoma. Diagnostic Laboratory Tests Specimens -Gastric biopsy specimens can be used for histological examination. Blood is collected for determination of serum antibodies. Smears: The diagnosis of gastritis and H pylori infection can be made histologically. A gastroscopy procedure with biopsy is required. Routine stains demonstrate gastritis, and Giemsa or special silver stains can show the curved or spiraled organisms. Antibodies Several assays have been developed to detect serum antibodies specific for H pylori. The serum antibodies persist even if the H pylori infection is eradicated. 4 Campylobacter & Helicobacter 5 Special Tests Gastric biopsy material can be placed onto a urea-containing medium with a color indicator. If H pylori is present, the urease rapidly splits the urea (1–2 days) and the resulting shift in pH yields a color change in the medium. In vivo tests for urease activity can be done also. 13C- or 14C-labeled urea is ingested by the patient. If H pylori is present, the urease activity generates labeled CO2 that can be detected in the patient's exhaled breath. Immunity Patients infected with H pylori develop an IgM antibody response to the infection. Subsequently, IgG and IgA are produced, and these persist, both systemically and at the mucosa, in high titer in chronically infected persons. Early antimicrobial treatment of H pylori infection blunts the antibody response; such patients are thought to be subject to repeat infection. Treatment - Triple therapy with metronidazole and either bismuth subsalicylate or bismuth subcitrate plus either amoxicillin or tetracycline for 14 days eradicates H pylori infection in 70–95% of patients. An acid-suppressing agent given for 4–6 weeks enhances ulcer healing. Proton pump inhibitors directly inhibit H pylori and appear to be potent urease inhibitors. - Either 1 week of a proton pump inhibitor plus amoxicillin and clarithromycin or of amoxicillin plus metronidazole also is highly effective. Epidemiology & Control H pylori is present on the gastric mucosa of less than 20% of persons under age 30 but increases in prevalence to 40–60% of persons age 60, including persons who are asymptomatic. In developing countries, the prevalence of infection may be 80% or higher in adults. Personto-person transmission of H pylori is likely because intrafamilial clustering of infection occurs. Acute epidemics of gastritis suggest a common source for H pylori. 5 Campylobacter & Helicobacter 6 6