Neonatal jaundice Source of bilirubin
advertisement

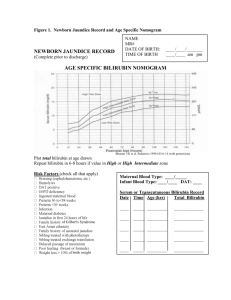
Neonatal jaundice: Source of bilirubin: It is derived from breakdown of heme containing proteins in the RES, Mainly from Hb,it forms about 75% of all bilirubin production. One gm of Hb produces 34mg of bilirubin. 25%of bilirubin is produced by heme containing substances like myoglobin,cytochromes,catalase….. Etiology: 1-Increased load :by hemolysis,polycythemia. 2-Damage or reduced activity of the transferase enzyme like hypoxia,hypothermia,hypothyroidism, infection. 3-Competition or blockage of the transferase enzyme. 4-Decreased activity of the transferase enzyme genetically or by prematurity. 5-Hypoprotienemia. 6-Displacement of bilirubin from combination sites by drugs,acidosis,increased free fatty acids secondary to hypoglycemia,starvation and hypothermia., Jaundice is the most common clinical condition in the neonatal period, it affects 50-60% of term newborns and 80% of prematures.It is clinically visible when it exceeds 5mgm/dl. Risk factors to get jaundice: 1-Low birth wt and prematurity. 2-Breast feeding. 3-Polycythemia. 4-A sibling affected. 5-Male sex. 6-Hemolytic conditions. 7-Extravasated blood. 8-Sepsis. Physiology:Red blood cell destruction releases globin,iron,and bilirubin which exists in two forms: 1-Albumin bound. bilirubin 2-Free . Glucoronyl transferase conjugate bilirubin in the liver and it becomes water soluble. The activity of this enzyme is about 0.1 to 1% of that of adults and reaches this level in 6-14 weeks after birth. Congugated bilirubin in the intestine may be deconjugated by beta glucoronidase and reabsorbed to undergo reconjugation in the liver(Enterohepatic circulation). Indications of investigations to determine the cause of jaundice: 1- If it appears on the first 24-36 hours. 2- Rise of SBR >5mg/dl/24 hours. 3- SBR more than 12mg/dl in term infants and more than 10mg/dl in preterm infants. 4- Jaundice persisting more than 10-14 days. 5- Direct hyperbilirubinemia. PHYSIOLOGIC JAUNDICE: 1-It is due to increased destruction of RBCS . 2-decreased ability of the liver to conjugate bilirubin. 3-Increased enterohepatic circulation. 4-Decreased uptake by the liver due to low level of ligandin. Characteristics: 1-Does not rise more than 12.9 ,very rarely 15mg /dl. 2-It appears on the 3rd-4th day of life. 3-Rarely increases by more than 5mgm/dl/day. 4-It disappears by one week in full term infants and by two weeks in preterm infants. 5-Healthy baby. Etiology: 1-Decreased RBC survival(40-60 days) 2Polycythemia,bruising,cephalhemat oma. 3-Poor feeding. 4-Dehydration. 5-Decreased glucoronyl transferase. 6-Shunt bilirubin(20%) from hem. Pigment. 7-Maternal diabetes. 8-Prematurity. 9-Oxytocin induction. Vasopressinlike action of oxytocin causes osmotic swelling of erythrocytes leading to decreased deformability and hence more rapid destruction of RBCS with resultant hyperbilirubinaemia in the neonate. 10-Delayed bowel movement. PATHOLOGIC JAUNDICE:It is pathologic if: 1-Occurs in the first 24 hours. 2-If bilirubin level rises 0.5mg /dl/hour or 5mg /dl/day. 3-If total serum bilirubin level exceeds 15mgm/dl in term infants or 10mgm/dl in preterm infants. 4-If there is evidence of acute hemolysis . 5-Signs of an underlying illness Clinical manifestations of Neonatal jaundice: Jaundice usually starts on the face and proceed caudally. Rough estimation can be done by pressing on the nose but it needs experience, division of the body in to zones can be used for rough estimation, there is interobserver variability. Face:5mg/dl Abdomen:15mg /dl Soles:20mg/dl CLINICAL TYPES: 1-Early jaundice(<10 days): A-first 24 hours:Causes: F Fetomaternal blood group incompatibility. I Intrauterine infection. R RBC enzyme defect. S Spherocytosis. T Thalassemia. 1-Haemolytic disease of the newborn: This is the most important type as SBR can rise to a dangerous level. The most common cause is Rh incmpatbility,the mother is Rh –ve and the baby is Rh +ve,there is severe jaundice,SBR increases up to 0.5mgm/dl/hour with a strong +ve coombs test. Pallor,reticulocytosis,hepatospleno megaly,+ve family history. When RBCS of Rh+ve fetus pass through the placenta of Rh –ve mother ,antibodies are formed in the mother which pass through the placenta to the fetus to cause hemolysis. Size of blood needed to cause sensitization is about one ml.The first baby escapes affection unless it is preceded by sensitization due to abortion or ameniocentesis. Not all Rh-ve mothers produce hemolysis in their babies because: 1-The baby may be Rh-ve. 2-Not all mothers produce enough Abs. 3-The mother might have been immunized by anti D immunoglobulin. 4-Fetomaternal transfusion occurs only in 50% of pregnancies. 5-Small family. 6-When the mother and baby are ABO incompatible. Hypoglycemia is common and is due to hyperinsulinism or hyperplasia of the islets cells of the pancreas. Hemolysis in utero causes severe anemia associated with low albumin presented as hydrops fetalis Treatment:The aim of treatment is to correct anemia and to prevent neurotoxicity. Intrauterine blood exchange transfusion is done for hydrops fetalis and fetal anemia PCV<37,it is done by canulation of the umbilical vein to raise PCV to 4555%. After birth cord Hb of 10gm/dl and SBR of 5mgm/dl are predictors of early blood exchange transfusion.Hb,PCV,Retics,should be measured 4-6 hourly. 2- ABO incompatibility: The mother is O and the baby is A or B.IgG antibodies are responsible,coombs test is –ve,blood film shows microspherocytes.It occurs in 2025% of pregnancies but hemolysis occurs in 10% only.Rarely the mother is A blood group and the baby is B and the opposite is true. 3- Rare causes of blood group haemolytic jaundice: subgroups,C,E,Kell,Duffy…… Other causes of haemolysis which present on the first day:G6PD deficiency,Pyrovate kinase deficiency,congenital spherocytosis,elliptocytosis,thalasse mia…………… 4-Sepsis. 5- Crigler-Najjar syndrome: can present early and continues beyond 10 days,It is due to glucuronyl transferase deficiency. . General investigations: SBR,Both direct and indirect,ABO and Rh, coombs test,Hb and Retics,blood film,G6PD assessment,blood sugar . Prolonged jaundice:>10 days in term and >14 days in preterm babies: Unconjugated hyperbilirubinemia. 1-Breast milk jaundice: The patient is usually well.2% of infants get the problem after the 7th day of life, maximum concentration is 10-30mg/dl reached during 2nd-3rd week.No signs of other illnesses,kernicterus has been reported but it is rare. Needs no treatment but phototherapy may be of help.. Usually settles by 6 weeks,but may go on longer up to three months.. Discontiuation of breast feeding for 48 hours is rarely needed, but it can reduce the level of jaundice. Betaglucoronidase in milk causes deconjugation of bilirubin diglucoronide in the intestine or it is due to an unidentified factors.. Good wt gain,normal liver,no evidence of hemolysis. Recurrence 70% in future pregnancies Breast feeding jaundice: Early onset of hyperbilirubinemia in the first week,occurs in 43% of infants due to decreased milk intake and dehydration. Treatment: Encourage breast feeding especially at night, no glucose water to enhance high density caloric milk. 2-Congenital hypothyroidism. 3-Intestinal stasis,obstruction,hirschsprung disease,atresia,meconium ileus. 4-sepsis 5-Galactosemia,fructosemia. 6-Cystic fibrosis by causing intestinal.ileus and its’effect on the liver. 7-Criggler Najjar syndrome. Prolonged conjugated hyperbilirubinemia: A value greater than 1.5mgm/dl or a fraction >10% of the total SBR is considered abnormal: Causes: 1-Infections. 2-Metabolic: galactosemia,fructosemia,ty rosinemia. 3-cystic fibrosis. 4-Dubin Johnson syndrome. 5-Rotors syndrome. 6-Idiopathic neonatal hepatitis. 7-Biliary atresia ,bile duct stenosis. 8-Choledical cyst. 9-Alpha one antitrypsin deficiency. 10-Hypothyroidism. Investigations (3) It depends on the situation. SBR,ABO and Rh of baby and mother,Hb,Retics,blood film,coombs test,blood culture,TORCH screen,reducing subs. in urine for galactosemia,G6PD screen,osmotic fragility test,T4,TSH,liver function tests,sweat test,abdominal ultrasound. . Transcutaneous bilirubinometry. Acute bilirubin encephalopathy: It describes the acute manifestations of bilirubin toxicity seen in the first weeks after birth manifested by poor feeding,high pitched cry,hypotonia. Chronic bilirubin encephalopathy: It is marked by athetosis,deafness,mild mental handicap,dental dysplasia. Kernicterus: Yellow staining of the brain with neuronal injury,there is necrosis,neuronal loss and gliosis.It is commonly seen in the basal ganglia,hypocampus,cerebellum,br ainstem and spinal cord.It is a pathological term. . Brain damage caused by bilirubin depends on: 1-Level of serum bilirubin and albumin. 2-Bilirubin binding by albumin 3-Status of the blood brain barrier. 4-Susceptibility of the CNS 5--Bilirubin is also produced in situ in the brain and metabolized by bilirubin oxygenase. damage to this mechanism may elevate local brain bilirubin level, in addition heme degradation in the brain produces carbon monoxide which may act as a local neurotoxin in some patients. Bilirubin gets entry to the brain cell by binding to membrane phospholipids and changed to bilirubin acid which is highly toxic to cell membrane and respiratory organells like mitochodria and endoplasmic reticulum. Clinical manifestations: Important points: 1-The level at which the baby is liable to get kernicterus is not well known. 2-Up to 15% of babies with subsequent kernicterus failed to show any definite neonatal neorologic symptoms. Clinical features:signs of Encephlopathy appear at 2-5 days after birth in term infants and as late as the 7th day in preterm infants,signs may simulate birth asphyxia,septicemia,hypothermia,h ypoglycemia,intracranial hemorrhage. Risk factors for bilirubin encephalopathy: 1-Severe hyperbilirubinemia. 2-Prematurity. 3-Asphyxia. 4-Acidosis. 5-Hypoglycemia. Pathology: Unconjucated bilirubin is deposited in the basal ganglia and the corpus subthalamicus,hypocompus,striate bodies,thalamus,globus pallidus,putamen,cerebellum. Preventable causes: 1- Early discharge. 2- Failure to check SBR. 3- Failure to recognize risk factors. 4- Underestimation of severity. 5- Lack of concern. 6- Delay in treatment. 7- Failure to respond to parental concern. Acute encephalopathy A-Phase1 :(1st 1-2 days):poor sucking,stupor,convulsions. B-Phase 2(middle of 1st week):hypertonia of extensor muscles,opisthotonus,retracted neck,fever,high pitched cry. C-Phase 3(after the 1st week):hypotonia. Chronic encephalopathy: First year:hypertonia,active deep tendon reflexes,delayed motor skills. After first year:movement disorders(choreoathetosis,tremor, jerking movement,abnormal slurred speech,sensorineural deafness).dental dysplasia,mental retardation may be present. What makes kernicterus an imminent problem? 1-Absence pathognomonic signs. of 2-Delayed presentation. 3-Failure to respond to parental worries. 4-Failure to recognize risk factors of kernicterus. 5-Failure of follow up of babies discharged early from the obstetric ward. 6-Failure to check SBR by depending on visual assessment. 7-Parental ignorance. Remember: 1-Direct bilirubin more than 20% of total is dangerous. 2-Dark yellow urine and pale stool are dangerous signs. Treatment of hyperbilirubinemia: The aim of therapy is to prevent neuronal damage by bilirubin. Treat the underlying cause like septicemia,acidosis,hypoglyc emia and ensure adequate hydration. Phototherapy: Bilirubin absorbs light in the blue range (Wave length420- 470nm).,however white ,narrow spectrum blue(super blue),green lights were also used.By photoisomerization unconjugated bilirubin is converted into non toxic conjugated bilirubin(lumirubin).. Bilirubin level decreases by2.5-3mgm/dl/day and 12mgm/dl in first 4-6 hours of phototherapy.Phototherapy works on the skin to a depth of 2mm from the epidermis. Because phototherapy “bleaches” the skin, both visual assessment of jaundice and TcB(Transcutaneos Bilirubinometry) measurements in infants undergoing phototherapy are not reliable. . The efficacy of phototherapy depends on: 1-The light energy emitted. 2-The distance between the light source and the baby(average 60 cm). 3-Amount of skin exposed ,the baby should be turned frequently. 4-The rate of haemolysis. 5-Hydration. 6-Intensity of light(double phototherapy,fibreoptic blankets) and type of light bulbs. Home phototherapy: This is an option way of treatment where facilities are available and fiber optic blankets are commonly used. The family should be well instructed and a well trained nurse should be present, it is usually used for simple jaundice. Complications of phototherapy: 1-Equipment failure. 2-Dehydration.30ml/kg/day fluid is added. 3-Loose stool. 4-Parental anxiety and interaction with their infant. 5-Skin rash. 6-Skin burn. 7-Bronze baby syndrome. 8-Eye damage. 9-Nasal obstruction. 10-Over heating. 11-In vitro DNA damage.It may be wise to shield the scrotum. 12-Decrease LV output and renal blood flow. 13- Hypocalcemia in preterm infants. Blood exchange transfusion: Exchange is done when the risk of kernicterus is imminent. A double volume exchange replaces 85% of the infant RBCS,and reduces pre-exchange bilirubin level to 50%. Volume of blood needed=85x2xbody weight. The time needed is about one and a half to two hours. There is no strict rule for indications of exchange transfusion,but by checking all the variables and risk factors,the table below is a guide: Age in days and serum bilirubin level 1234567 we igh t <1 8 8 8 1 1 1 1 00 0000 0 10 1 1 1 1 1 1 1 00- 0 0 0 0 0 5 5 12 49 12 1 1 1 1 1 1 1 50- 2 2 2 5 5 5 5 14 99 15 1 1 1 1 1 1 1 00- 5 5 5 5 5 5 6 17 49 17 1 1 1 1 1 1 1 50- 5 5 5 6 6 7 7 19 99 >2 1 1 1 1 1 1 1 00 8 8 8 8 8 8 8 0 Term babies 20 mgm/dl.BET should be done at low level if there is a risk of kernicterus,the baby is acidotic,septicemic,hypothermic,hy poglycemic,or another baby had kernicterus, The best guide is the clinical judgment. BET is usually done by canulation of the umbilical vein but a peripheral vein and artery can be canalized this is called isovolumetric exchange. BET is done for other diseases like septicemia,severe anemia,DIC,poisoning…. Complications of blood exchange transfusion: 1-Early complications: acidosis,electrolyte disturbances,hypoglycemia,bradyca rdia, Hypocalcemia,hypomagnesemia,thr ombosis,apnea,hypothermia, infection ,gangrene of a leg, death in 0.3/100 procedures. 2 -Late complications: 1-portal vein thrombosis and portal hypertension. 2-Late onset anemia. 3-Graft versus host disease. 4-Inspissated bile syndrome. Blood typing and cross matching: 1-Rh isoimmunization:The blood must be type O,Rh negative,low titer anti A ,anti B blood,it must be cross matched against the mothers’plasma and red cells. 2-ABO incompatibility:the blood must be type O,Rh compatable with the mother and the infant or Rh negative ,low titer anti A,anti B blood.It must be cross matched with the mother’s and the infant’s blood. 3-Haemolysis from other causes like metabolic causes,other haemolytic anemias ,the blood should be cross matched against the infant’s plasma and RBCs,the blood should be fresh(<48 hours) and should be agitated frequently. Other therapies: Protoporphyrins:It may inhibit the conversion of biliverdin to bilirubin by heme oxygenase. 2-IV immunoglobulin,500mg/kg per dose, twice daily for three days,useful in coomb's +ve infants by reducing hemolysis. 3-Phenobarbital? Key Messages: Promote and support successful breastfeeding. 2. Recognize that visual estimation of the degree of jaundice and those under 1. phototherapy can lead to errors. 3. Interpret all bilirubin levels according to the infant's age in hours. 4. Recognize that infants at less than 38 weeks' gestation are at higher risk of developing hyperbilirubinemia and require closer surveillance and monitoring. 5. Perform a systematic assessment on all infants before discharge for the risk of severe hyperbilirubinemia. 6. Provide appropriate followup based on the time of discharge and the risk assessment. 7. Treat newborns, when indicated,phototherapy or exchange transfusion .