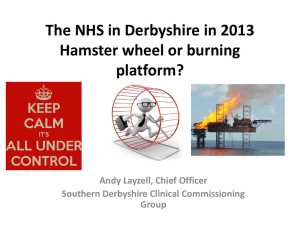
Quality Account 2011/12 Derbyshire Community Health Services NHS Trust
advertisement
Derbyshire Community Health Services NHS Trust Quality Account 2011/12 Contents Opening comments from Chief Executive Tracy Allen 5 A statement from the Chief Executive Tracy Allen and the Chair Andrew Fry 6 Introduction by the Director of Quality/Chief Nurse and the Medical Director 8 Monitoring progress 8 Overview of 2011/12 8 Looking forwards Quality Improvement Priorities for 2012/13 10 Review of Quality Improvements for 2011/12 13 Achievements, Awards and Accolades 14 Evidence of improvement in patient safety 17 Infection prevention and control 18 The Deep Clean Team 18 Infection Prevention Champions and Hand Hygiene (IP&C) 18 High Impact Actions Falls and Bone Health 19 Babington Rehabilitation Centre – Launch of the New Falls Programme 19 High Impact Actions - Tissue Viability 20 High Impact Actions - Catheter Acquired Tract Infections (CAUTI) 21 Venous Thromboembolism (VTE) 22 Safety Express 23 Rapid Implementation of National Patient Safety Alert on Syringe Drivers 24 Safeguarding 24/25 Evidence of clinical effectiveness improvements 26 Breast Feeding Success 27 Stroke 28 Discharge Planning 29 Dementia Care 29 Mortality Audit 30 Care of the Acutely Ill Patient 31 Leicestershire County and Rutland Out-patient, Diagnostic and Day Surgery 32 Hinckley and District Hospital 32 Loughborough Hospital 32 2 DCHS QUALITY ACCOUNT 2011/12 Coalville Hospital 33 Making a difference - a focus upon children and young people 33 Sexual Health Promotion Service 34 Specialist Children Services - Answering Awkward Questions 34 Speech and Language Therapy 35 Clinical Audit 35 Information Governance 38 Research and Knowledge Services 38 Clinical Records 39 Evidence of improvements for patient experience 40 Patient and Public Involvement (PPI) 41 Privacy and dignity 42 Patient experience 43 Carers 44 Listening and learning through complaints 44 Nutrition and Hydration 45 Supporting our End of Life patients and families 46 Addressing Spirituality [Riverside] Art Work 46 Tea Party 47 Improving the patient environment 47 Ilkeston Hospital 47 Patient Leaflet 47 Quality Focus - Occupational therapy outcomes 47 What others say about us 48 CQC update for Quality Account 2011/12 48 NHSLA - National Health Service Litigation Authority 48 Health Ombudsman outcomes in 2011/12 48 Coroner’s Inquests 49 Never Events 49 Serious Incidents 49 Patients/carers 49 What our Staff say 49 Declaration and Statements 50 Glossary 52 Are we accessible to you? This publication is available on request in other formats (for example, large print, easy read, Braille or audio version) and languages. For free translation and/or other format please call 01773 525099 extension 5587, or email us at: communications@dchs.nhs.uk To see the full list of the services we provide, please visit www.dchs.nhs.uk or call us on 01773 525099 for support. DCHS QUALITY ACCOUNT 2011/12 3 A statement from the Chief Executive Tracy Allen and the Chair Andrew Fry 4 DCHS QUALITY ACCOUNT 2011/12 Opening comments from Chief Executive Tracy Allen On behalf of our Trust I am pleased to present this Quality Account which sets out our hard work, achievements and areas of improvement for 2011/12 and our priorities for 2012/13. We place great emphasis on the positive culture and values of our Trust, the DCHS Way, investing and believing in our staff to deliver a high quality service. I believe that the DCHS Way and being proud of how we work will help us to improve and meet the challenges ahead of us. The scale and complexity of this challenge is very great for our Trust as an integral part of the health and social community. This community is actively involved in listening to local people and working together to deliver a better service as part of the new systems laid out in the Health and Social Care Act. Our success has been acknowledged in many ways over the last few years winning regional and national awards for our services. Our journey to become a Foundation Trust has helped us to improve our quality and performance systems. These have been tested by expert external scrutiny. In 2012/13 we plan to become one of the new community Foundation Trusts in England. We really look forward to engaging and working with our membership and governors helping us to be a well run, financially stable Trust that has quality at it’s heart. DCHS QUALITY ACCOUNT 2011/12 5 Statement of Directors’ Responsibilities in respect of the Quality Account In preparing the Quality Account we confirm that: • The Quality Account presents a balanced picture of the Trust’s performance over the period covered • The performance information reported in the Quality Account is reliable and accurate • There are proper internal controls over the collection and reporting of the measures of performance included in the Quality Account and these controls are subject to review to confirm that they are working effectively in practice • The data underpinning the measures of performance reporting in the Quality Account is robust and reliable, conforms to specified data quality standards and prescribed definitions, is subject to appropriate scrutiny and review; and the Quality Account has been prepared in accordance with Department of Health guidance. The directors confirm to the best of their knowledge and belief they have complied with the above requirements in preparing the Quality Account. By order of the Board 6 DCHS QUALITY ACCOUNT 2011/12 “In our Trust we have defined our way of working as the DCHS Way. This places quality as a golden thread that runs through DCHS whether it is about services, people or business matters.” DCHS QUALITY ACCOUNT 2011/12 7 Introduction by the Director of Quality/Chief Nurse and Medical Director 8 At Derbyshire Community Health Services NHS Trust (DCHS) we regard our annual Quality Account as an extremely important public report. We take great care to listen to the views and feedback from the readers of this report to continuously improve it. The purpose of this report is to help patients, their family and carers (as well as the wider public) hold us to account in relation to the quality of the services we provide. It shows how well we did in the last year to improve the quality of services, identifies what we could do better and sets out our plans for the forth-coming year. or business matters. DCHS responds to the financial pressures first and foremost through Quality Improvement techniques to help raise standards of care and offer better value for money to our public. In our Trust we have defined our way of working as the DCHS Way. This places quality as a golden thread that runs through DCHS whether it is about services, people We welcome your feedback in relation to this report and our quality priorities for the year ahead. Monitoring progress Overview of 2011/12 We were set a greater challenge for 2011/12 building on the very high standards and success of 2010/11 where we achieved 17 out of our 18 “CQUIN” targets. CQUIN (Commissioning for Quality and Innovation payment framework) is the national contract method for incentivising improvements against specific topics or service areas. A proportion of DCHS income in 2011/12 was conditional on achieving quality improvement and innovation goals as part of our contract. An example of how a focus area for quality improvement is translated into CQUINs includes the High Impact Action areas published by the Chief Nursing Officer. These relate to the CQUIN targets for falls, pressure ulcer, catheter acquired infection reductions needed and additionally venous thrombo embolism (VTE) assessments. In order for the Trust to receive full payment for the services it offers we must meet these targets. The contract for 2011/12 contained higher expectations for delivering quality as well as new specific, more detailed and stretching CQUINS. There were 11 in total with 6 national / regional targets and 5 local targets agreed between our commissioners and ourselves. We successfully met or exceeded the following CQUIN improvement targets: • Patient Experience • Engagement with Carers • Care Planning • Preventing readmissions to acute hospitals services • Equitable access to specialist services for patients with Learning disabilities • Assessing and preventing Venous Thromboembolism (VTE) • Reduction of urinary catheter acquired infections • Breast feeding sustainment rates. DCHS QUALITY ACCOUNT 2011/12 This year, in addition to our wide range of established services we have taken on the hosting of Planned Care Services for Leicestershire County and Rutland and also were awarded the contract for their community Dental Services. This Quality Account includes information on all of our services. During 2011/12 our total income for providing clinical services was £170m, of which £2.3m was dedicated to the delivery of CQUINs across our services. Of this we achieved 87% of the financial value. Further details of the agreed goals for 2011/12 and for the following 12 month period are available electronically. It was noted by the commissioners that whilst we have made significant improvement we narrowly missed some targets: • Reducing Falls • Stroke Community Care • Pressure ulcer (evidence of re-assessment) • Dementia indicator for OPMH (older people mental health) - reassessment of medications. We have set ourselves new plans for the coming year, with clear actions to maintain the good performance of the targets we achieved as well as meet the improvements for the ones we narrowly missed. These will be monitored in our contract for 2012/13. In addition to the CQUIN quality targets already mentioned there are other quality standards and targets in place which are set by the government and monitored by our commissioners and external regulatory bodies (such as the Care Quality Commission – CQC). Our Board of Directors has overall responsibility to ensure that these are delivered and during the past year we made a number of changes within our governance and assurance structures to ensure that these were being met. Our Quality Strategy provides a framework for the delivery of quality services within DCHS and within this we have defined quality as: • The delivery of services which are focused upon patient safety and reducing risk which may cause harm • The delivery of services which are effective in the context of clinical outcomes and patient related outcomes • The delivery of services which are considered by our patients, service users, their carers and families as being a positive or good patient experience. This forms part of our Quality Governance Framework which incorporates our strategy (Integrated Business Plan), the capabilities and culture within the organisation, our processes and structures (which support delivery) and how we measure success. DCHS QUALITY ACCOUNT 2011/12 9 Looking forward Quality Improvement Priorities for 2012/13 As the NHS prepares itself to meet the demands of the new Health and Social Care Act, working in partnership with our patients and their carers, other service providers, statutory agencies and the voluntary and community sector, will be key. This will be particularly important as we redesign our services to meet the needs of our local communities in view of the challenging economic and demographic climate. The delivery of quality services, by quality people within a quality business during this time is our priority. DCHS have identified key quality aims as part of our Quality Strategy and Annual Plan. These are: • Keeping patients safe whilst in our care • To get the basics right • To put patients at the centre of care delivery. Monitoring the delivery of these and our other quality targets are through our quality governance systems, with the Board of Directors having overall responsibility. These assurance systems include validated 10 DCHS QUALITY ACCOUNT 2011/12 evidence and data from our performance monitoring systems as well as our other quality and safety processes such as service quality and safety visits which span from frontline care to the Board Room. (In addition, we have developed a Safety and Quality Early Warning System (SQEWI) which combines quality, safety, patient feedback and staff performance measures to strengthen our process and help us to identify where we need to improve. This will enable us to act sooner and reduce avoidable harm to patients. Safety Express (which is a quality improvement tool as part of a national Safe Care programme) continues to be the way in which we will improve patient safety and quality of care. We are also aware from those who use our services that they wish to be listened to and involved in their care, treated with fairness, dignity and respect and treated by staff who demonstrate compassion. In 2011/12 NHS Midlands and East launched its Ambitions Programme with its 5 priorities. Two ambitions to emphasise in our next years objectives include the Patient Revolution and Eliminating Avoidable Pressure Ulceration. We have a new set of improvement measures for 2012/13 that we have agreed with our commissioners, these are fewer in number but have more national direction and regional overview. This is to help to inform collective improvements and for benchmarking one organisation against another. Clinical improvements remain a high focus and will be performance monitored against improving targets as part of our contract. The high impact action areas remain as part of this set with the rollout of the safety thermometer (which enables us to measure the impact of care) into community services as a driver to bring about reduction of harm to patients. Patient experience and patient engagement are high profile with significant work expected to demonstrate how we seek out and act upon the views of the service users, their families and their carers in all that we provide and undertake in meeting their health care needs. This programme of work is known as ‘the Patient Revolution’ and is being taken forward under the umbrella of our new Patient Experience and Involvement Strategy. Patients who use our service will get to know this as the “Family & Friends test” asking how likely they would recommend our services. 2012/13 Contracted Quality Improvement (including CQUIN) The priorities agreed in our contract for this year has a more national emphasis. This is to help national and local benchmarking of good practice and performance. It is understandable that many of these targets have an acute hospital focus. As a Community Trust we provide a range of hospital and community services and work closely with our local commissioners to see how best we can deliver improvements in these areas. DCHS QUALITY ACCOUNT 2011/12 11 Our CQUIN priorities for improvement as we move forward into the future are set out as follows: National • Reducing avoidable deaths, disability and chronic ill health from venous- thromboembolism (VTE) • Patient experience - Improve responsiveness to personal needs of patients • Dementia - Improve diagnosis of dementia, using risk assessment, in hospital settings • NHS Safety Thermometer - Improve the safe care of patients with regard to pressure ulcers, falls, urinary catheter care and VTE prevention. Regional • Patient Revolution - one of the 5 ambitions of NHS Midlands and East SHA. Measuring and improving the experience of patients using our services. Local • Support for residents of care homes - Improve partnership support with care homes • Nutrition - Reduce malnutrition in the frail elderly population 12 DCHS QUALITY ACCOUNT 2011/12 • Intermediate care support for patients in a domiciliary setting • Make every contact count - promoting key health and well being messages to all. These are mirrored by the regional ambitions for Health Care Delivery for the SHA regional cluster and pick up the national direction on priorities for health improvements. Delivering Same-Sex Accommodation Declaration of compliance DCHS has met the requirement to Eliminate Mixed Sex Accommodation and have not reported any breaches in 2011/12. Our programme for environmental improvements has continued throughout the year and these have included both eliminating mixed sex accommodation issues and meeting infection prevention and control standards. All premises have been assessed to determine they are ‘fit for purpose’. Review of quality improvements for 2011/12 This section describes in more detail our successes during the last year. We are also keen to present examples of where we could better, to ensure we give an open and balanced account. To help understand this information we have presented this in the following sections: Achievements Awards and Accolades Patient Safety (trying to prevent patients from being harmed) Clinical Effectiveness (making sure our treatment and care works well) Patient Experience (listening to what people think and feel about our services) DCHS QUALITY ACCOUNT 2011/12 13 Achievements, Awards and Accolades St Oswald’s our newest hospital was formally opened by HRH Prince Edward in May of this year Care Home Support Team This pilot project won a national award from the Health Service Journal (HSJ) for “Liberating Ideas”. It demonstrated that supporting patients in care homes helped to reduce falls and hospital admissions by 60% among frail elderly patients. The team worked with 29 care homes. This service has helped to improve residents’ sense of wellbeing and confidence, reducing the fear of falls and accidents. The learning from this initiative has been shared across our Trust and many others, and we are using this learning to further facilitate work in supporting care homes. National Guidance Queens Nurse Awards Gill McKay, Health Visitor, and Caroline Hannan Professional Lead, have both been awarded the prestigious title of Queen’s Nurse (QN) at awards ceremonies given by The Queen’s Nursing Institute (QNI), in London. They are representatives of a small cohort of 35 nurses recognised this year for excellence in practice. 14 DCHS QUALITY ACCOUNT 2011/12 The Derbyshire Sexual Health Promotion Service peer education is to be included as an example of best practice in guidelines being produced by the National Chlamydia Programme. Locally it is called the ‘Well Sexy Programme’ and is a peer support outreach service for young people between 15-25 yrs. DCHS has very high levels of uptake compared to some parts of the country. NHS Microsoft Award We received the NHS Microsoft Office Skills Training (MOST) Centre of Excellence award. This demonstrates a high level of commitment from our Trust to the training and certification of our staff. There are 187 MOST centres across England and we are the eighth centre to achieve the Centre of Excellence award. Safety Express We won a national award for the role we have played in developing the ‘Safety Express’ programme, a national campaign to providing safe care for NHS patients. Infection Prevention and Control (IP&C) Team A board game developed by our IP&C Team won a NHS East Midlands Patient Safety Innovation Award for making learning about safety more fun. Judges were so impressed that they have awarded the team £1,000 to develop the game further. DCHS QUALITY ACCOUNT 2011/12 15 These next pages are to provide contextual information of the range of activities undertaken to meet quality improvements Each of the core subect areas that reflect the quality improvement indicators are grouped together into the following colours: Evidence of improvements in patient safety Evidence of clinical effectiveness improvements Evidence of improvements for patient experience 16 DCHS QUALITY ACCOUNT 2011/12 Evidence of improvements in patient safety DCHS QUALITY ACCOUNT 2011/12 17 PATIENT SAFETY Infection prevention and control Target: to continue to reduce healthcare associated infections. What we achieved: • Hand Hygiene more than 97% compliance with a World Health Organisation Advanced Category status • No MRSA / MSSA Bacteraemia (no superbug infections in patients bloodstream) • Clostridium Difficle (a potentially severe bowel infection): halved our last years rates of infection with 12 recorded cases. What next: Our annual performance for Clostridium Difficile infections is not published through the national Health Protection Agency (HPA) system which focuses on Acute Trusts. Our own calculations based on the HPA system demonstrates that we have comparable performance. Despite these very good results, in this last year we had an episode on one ward of increased Clostridium infection affecting three patients. We have learned by investigating this incident how the management of these could have been better. We have now supported staff to improve and maintain standards. Our target is to continue to reduce rates of healthcare associated infections (HCAI). The Deep Clean Team Deep cleaning is an annual requirement and is incorporated into a rolling programme over and above the daily cleaning routine. This team, introduced in 2010, is now embedded and has an identified programme of cleaning for areas deemed to be requiring specialist cleaning interventions and helps us to be able to reopen wards much more rapidly. In 2011/12 the team worked hard providing specialist support in Noro Virus (“winter vomiting bug”) outbreaks. Again we have learned what works well and what we need to do better. This includes improving communications both across our teams and the public (especially visitors). 18 DCHS QUALITY ACCOUNT 2011/12 Simon Goldsmith IP&C Champion Programme Facilitator. DCHS is clearly able to demonstrate a commitment to creating a patient focused clean and safe environment having established this rapid intervention specialist team approach. This links to our PEAT (Patient Environment Assessment Team) inspections. Infection Prevention Champions and Hand Hygiene (IP&C) These Champions continue to play a key role to ensure all staff adhere to clinical policy and professional standards and to challenge any member of staff demonstrating poor IPC practices providing support and information. The Champion’s groundwork in hand hygiene compliance has seen high compliance rates of just over 97%. We still have more to do to reach the Trust target of 100%. This helps patient safety by reducing the risk of health care associated infections and helps patients feel more secure and positive about their care. In December 2011 we made an assessment of Hand Hygiene provision across our 12 community hospitals and Ashgreen Learning Disabilities Centre using the World Health Organisations online assessment tool. DCHS scored 465 out of a possible 500 which places us firmly in the advanced category, an indicator of good practice. High impact actions These are national improvements set for all nurses by the Chief Nursing Officer of England High Impact Actions - Falls and Bone Health Target: to reduce harm from falls What we achieved: A raised awareness of falls prevention actions and a reduction of serious harm from falls. What next: Our target is that at least 96% of our in-patients do not fall whilst in our care and that serious harm does not happen as the result of a fall. DCHS remains committed to providing high quality, evidence based treatment and care for people who are at risk of or have fallen, to improve their bone health and reduce the harm from these falls. Our falls strategy and interventions help patients in our care e.g. in one of our hospitals as well as in their own homes. Many service improvement initiatives and developments have been put in place and will continue to be developed and implemented this year: • Launch of “Safety Express” initiative across all in-patient services. This includes the “clinical rounding” process which has supported all staff to continually monitor and act on falls risk • Development of Preventing Harms, (including falls), ‘Board Game’. This is a tool that promotes whole team thinking and planning to keep patients safe • Monthly auditing of ‘4 harm’ incidents and sharing these results at local team level so front line staff can learn and plan • Continual review of falls prevention and management policies and associated protocols and clinical tools • Identification and training of falls champions for all DCHS patient facing services. The falls champion is the local resource for teams to use to support them to turn local and national policy and protocols into every day falls prevention and management actions and practice • Development of new accessible training materials to raise awareness for all DCHS staff in their individual roles and responsibilities. DCHS worked with commissioners and acute trust partners to develop and implement an integrated care pathway for falls across Derbyshire. This ensures high quality, evidence based falls care is standard across the county and gets people to the right services at the right time. This pathway includes a ‘Single Point of Access’ to falls services for GPs and other referrers, a falls prevention advice and information service, and new arrangements with ambulance services who attend people who have fallen but do not need to go to hospital, and a ‘falls recovery’ service for people who live in managed accommodation who fall but again do not need to go to hospital. This has resulted in a reduction of unnecessary admissions to our hospitals. Babington Rehabilitation Centre – Launch of the New Falls Programme The Falls Programme is provided for patients in the Amber Valley area aged 65 and over who have had a fall or are at risk of falling. These patients benefit from an experienced multidisciplinary team input from physiotherapists, occupational therapists, nurses, pharmacists and rehabilitation support workers. After an initial assessment, suitable patients attend a seven week programme and at the end of this period, benefit from improved balance and co-ordination, increased awareness of falls prevention, identification of falls risk factors, increased confidence and self-esteem, promotion of independence, peer group discussions as well as social interaction. On evaluation of the programme those patients who have attended this programme have a significant reduction in further falls, supporting our work in reducing falls and harm from falls. DCHS QUALITY ACCOUNT 2011/12 19 High Impact Actions - Tissue Viability Target: To improve reporting, monitoring and assessing all grades of pressure ulcers, and a reduction of in-patients that develop a new pressure ulcer whilst in our care (Safety Express). What we achieved: Our reporting increased across the organisation and all pressure ulcers were investigated (using root cause analysis). Our inpatient areas achieved an improvement from 83%-89% of in-patients who were assessed within 6 hours of admission, documented and reassessment increased from 26%-79% for those who did not develop a new pressure ulcer whilst in our care. What next: We are aiming to meet the Strategic Health Authority (SHA) Ambition 1 which is to eliminate all avoidable Grade 2, 3 and 4 pressure ulcers by December 2012. 20 DCHS QUALITY ACCOUNT 2011/12 Pressure ulcers are areas of damaged skin which can lead to ulceration and infection. People who are immobile or unwell are more likely to get these. Our Tissue Viability team will be working closely with staff across the organisation, other providers of care and patients in order to meet this challenging ambition. • Our improvement work is focused upon evidence based practice and learning from elsewhere in order to make the necessary reduction in patients developing pressure ulcers. This includes raising awareness of patients and staff, improving staff training, improving our data collection and monitoring systems and focussing on prevention. This will be enhanced by working within the SHA Ambition programme of work. Well planned interventions and care planning with patients and carers can ensure that no further deterioration of the skin occurs. To support this we have developed a Patient Information Leaflet and Self Care Advice Sheet for patients and carers about how they can help to improve or prevent pressure ulcers developing. High Impact Actions - Catheter Acquired Tract Infections (CAUTI) Target: To reduce the numbers of in-patients with an indwelling urinary catheter and the number of catheter acquired infections. What we achieved: A reduction of the numbers of in-patients with an inappropriate catheter whilst in our care from 19.9% to 11.9% and a reduction in the number of those patients who had an CAUTI from 7.1% to zero. What next: To work with our acute hospital provider partners to continue to monitor appropriate use of catheters, extend our improvement work across our community services and to continue to reduce catheter acquired infections. Catheters are used to help treat patients with problems of passing urine. Medical evidence tells us that these urinary catheters should only be used where absolutely necessary because they can cause or worsen urinary infections. To support the improvements a Specialist Nurse was appointed to provide clinical support to our Community Hospitals. The nurse visited every hospital in-patient area regularly to monitor and assess the use of catheterisation, provide training and to promote best practice. A detailed audit was undertaken to establish a baseline for improvement and the re-audit demonstrated improvement in reducing the numbers of patients with a catheter while in our care and the number of those patients who did not have an infection. A new DVD training resource for staff has been developed that will enable anyone involved with catheter care to increase their knowledge. Any catheter acquired urinary infection that develops within our care is recorded and reported as a clinical incident which will enable us to monitor the situation, identify any trends and deal with these immediately. Important next steps in improving continence and catheter care include working with different professionals to develop a better system to explain and communicate care plans when patients move from different care settings. DCHS QUALITY ACCOUNT 2011/12 21 Venous Thromboembolism (VTE) Target: >75% assessment rate for patients at risk of VTE. What we achieved: Average 89% assessment rate. What this means: By assessing and treating patients at risk of VTE it reduces the chance of harm and in 2011/12 we did not have a recorded in-patient death from VTE. VTE is the collective name for conditions where a blood clot forms in the body, usually in the deep veins in the leg. This is known as a Deep Vein Thrombosis (DVT). These thromboses can sometimes travel from the legs to the lungs where it is called a pulmonary embolism (PE). These blood clots are more likely to form when patients are ill and can’t walk easily during or following surgery or when they have other acute medical illnesses. These conditions can cause serious health problems and can occasionally be fatal. 22 DCHS QUALITY ACCOUNT 2011/12 • For the last two years DCHS has had in place a programme to assess and provide prophylaxis (preventative treatment) where appropriate, to all of our in-patients and day case patients • For the year 2011/12 we were set a CQUIN target by our commissioners of 75% of these groups of patients to have been assessed • We measure the results through specialist data collection systems and by doing audits in the wards and theatres, and we have exceeded this target with an average score of 89% consistently since June 2011 • For the new year starting April 2012 we will be expected to achieve a 90% assessment rate for these groups of patients. The assessments are carried out by an appropriately trained nurse or doctor and if preventative treatment is found to be necessary it is given by a small injection under the skin for a period of days. We also measure whether there have been any ill effects arising from the use of the treatment medication or whether we have had any untoward incidents or deaths arising from these conditions. During 2011/12 we have had no deaths arising from DVT or PE within our community hospital in-patients. Safety Express Target: To embed the safety thermometer measurement tool onto all our wards to reduce harm in our hospitals. What we achieved: Introduction of the tool on all wards. Monthly real time data is now provided that informs us for early interventions Monitoring and reporting of all catheter acquired infections, and the appropriateness of catheter use. What Next: To implement this tool within our community nursing services (in addition to the community hospital setting) and to embed Safety Express (Quality and Patient Safety improvement programme) across our services. Safety of our patients and staff is our highest priority and to further this DCHS signed up to the Department of Health Safety Express Programme which was developed from an initiative called the Patient Safety First Campaign. The effectiveness of Safety Express is measured using the Safety Thermometer tool. The vision nationally is to reduce harm from four main areas: • Pressure Ulcers • Falls • Catheter acquired urinary tract infections • Venous Thromboembolism As part of this national pilot we have introduced the safety thermometer tool to our hospitals wards. Initially as a pilot on 2 wards, this was then rolled out to all wards in all our hospitals. The implementation of the ‘Thermometer’ as part of the Safety Express programme is significantly strengthening how we collect and report data. This system supports other essential quality systems including DATIX incident and reporting. We now capture all grades of Pressure Ulcers and all Catheter Acquired Infections that happen within our care. Whilst there are few serious incidents, we feel we can learn from these. Our audit plan is being revised to align itself to the programme, providing us with richer data. We have been able to influence the national agenda in terms of the way that the programme is developing and how it impacts locally. Our input at a national level has been acknowledged in receiving a National Award for our contribution to the programme. We have • Raised awareness with our staff delivering presentations and Q&A session • Worked collaboratively with our regional SHA developing posters and leaflets for staff and the public. A DVD is in production • Introduced Safety Rounds to our community hospitals, and have developed a Safety Round tool suitable for the community setting • Development of a learning resource ‘Safety Express’ board game which will be used for staff training. DCHS QUALITY ACCOUNT 2011/12 23 Rapid Implementation of National Patient Safety Alert on Syringe Drivers Target: To comply with a new national equipment safety standard. • Better monitoring of use and equipment • Safer, more effective service, more positive patient satisfaction. What we achieved: Syringe Drivers are used predominantly in our Trust to deliver medicines as a continuous injection under the skin to reduce pain and distress of patients often approaching the end of their lives. By controlling these distressing symptoms in a safe way we help improve patients’ care and their experience. • removal of old / non compliant devices across the Trust • replacement with new syringe drivers • supported RCN accredited training. What this means: • Reduced safety risk factors • Reduced error and data retrieval problems from devices Safeguarding What we achieved: • New appointments of named nurses • Better organisation and leadership of our safeguarding teams • Closer working with partner organisations including Social Services • Delivered more training to staff about safeguarding. together within one Safeguarding Unit at Babington Hospital. With the increase in staff the team have raised awareness and improved support across the organisation. The Safeguarding Adults Team has strong links with the Health Community and partner agencies and has staff co-located with the police in the Central Referral Unit. This enables a consistent approach to safeguarding across all agencies and provides a timely and appropriate response to safeguarding concerns. We plan to further the developments with the appointment of a Head of Safeguarding and drive up standards through benchmarking and audit. Safeguarding Children Adults Our Trust is involved with many people who might be frail, elderly and or vulnerable to harm and abuse. This is why we have continued our investment and improvements to this specialist team. We appointed two new Named Nurses and brought the Adults and Children’s teams 24 DCHS QUALITY ACCOUNT 2011/12 Safeguarding children remains a high local and national priority. After the death of Peter Connelly – ‘Baby P’ it has been evident that the number of children at risk or referred to specialist services and social care nationally has risen. This increase is reflected in Derbyshire. During 2011, DCHS Safeguarding Children Service has continued to provide its core function of providing expert supervision, advice and training to health staff. In 2011/12 The Safeguarding Children Service delivered specialist training to 2581 members of staff, an increase from 2010 when 1215 staff received similar training. Our team of Lead Named Nurse and Locality Named Nurses work across our services and with other agencies (such as the Local Authority, Multi-Agency Teams (MAT), etc. providing the health expertise in safeguarding matters. We also continue to embed into practice learning from Serious Case Reviews and monitoring the impact of this is a joint priority for safeguarding services across Derbyshire in the coming year. The Named Nurses are involved in any Serious Case Reviews of suspected abuse. This includes scrutinising health records, individual professional practice, communication systems and programmes in order to identify any concerns and develop an action plan. These reviews help all the agencies involved understand how staff and systems performed and possible areas for improvement. As part of our policy of being open we publish these reviews and actions for improvement where possible. Learning from Serious Case reviews is also translated in our training programme for staff on both a local and a multi agency basis. Key developments in 2012/13 • To further improve electronic reporting and recording systems • Further improvements in joint working with social services • Review and implement the Munro Report of Safeguarding and the ‘Think Family’ strategy • Take forward and implement actions following the Ofsted review of Children’s Services in Derbyshire (undertaken in 2011/12). DCHS QUALITY ACCOUNT 2011/12 25 Evidence of clinical effectiveness improvements 26 DCHS QUALITY ACCOUNT 2011/12 Evidence of clinical effectiveness improvements Breast feeding success Target: To demonstrate we have supported 83% of our mothers to sustain breast feeding beyond 6 weeks. What we achieved: We successfully demonstrated supporting 84% of mothers exceeding our target. What next: Continue to maintain this level of support to our new mothers. • Achieved Baby Friendly Stage 21 accreditation, an international benchmark of quality. We received a commendation for the quality of evidence submitted • Developed and launched a breastfeeding public information website with live links to local information • Employed and trained some local breast feeding mothers to act as peer supporters within their own local community • Targeted work with low uptake breastfeeding communities using our new peer supporters to help mothers succeed • Established breastfeeding champions who work in partnership with wider services led by our health visitors. This year we set ourselves the target of achieving 84% of the mothers who started breast feeding and supporting them to carry on breastfeeding their baby beyond the age of 6 weeks which we have succeeded. Working with our wider partners will help us to maintain this level and encourage more mothers to try breastfeeding at the point of birth. We know that breast feeding gives the best long term health outcomes for our next generation. DCHS QUALITY ACCOUNT 2011/12 27 Stroke Target: To assess all patients with new strokes and provide individual planned therapy programmes. What we achieved: 87% received their complete planned therapy programme. Assessment of wellbeing and recovery are the areas we need to improve upon as we did not do this as well as expected. What next: Achieve further improvement to the comprehensive assessment for new stroke patients received into our care. ‘Stroke has a major impact on individual lives and on the whole nation’s health and economy. Strokes are a blood clot or bleed in the brain which can leave lasting damage, affecting mobility, cognition, sight or communication. After stroke, individual recovery can be enhanced through specialist therapy and wider social support.’ 28 DCHS QUALITY ACCOUNT 2011/12 The National Strategy for Stroke, December 2007 We remain committed to working with our acute Trust partners to provide high quality, evidence based stroke care and rehabilitation, in line with national standards. Many service improvement initiatives and developments have been put in place in 2010/11 and will continue to be developed and implemented next year including: • Identified Lead stroke clinicians • Multi-disciplinary stroke clinical reference groups • Developing standard outcome measures for stroke which will allow real evaluation of how effective the care provided by all teams is • Collaborative Stroke Discharge Service with the Chesterfield Royal Hospital • The Derbyshire Stroke Co-ordination and Support Service and Single Point of Access (SPA) continues to develop providing access for stroke survivors, their families and carers, to advice and information about stroke and holistic long term support to stroke survivors. Discharge Planning Target: 100% of our patients to have a planned discharge date in place. What we achieved: All patients had a planned discharge date in place and all planned dates were met. What Next: To sustain this approach and to reduce the length of time patients need to stay in our hospitals. Our Community Hospitals implemented several strategies to support well-organised, safe care through appropriate planning with the patient and their relatives/carers from admission to discharge. The implementation of the “JONAH” discharge planning database underpins the DCHS Discharge Planning process, providing a Multidisciplinary approach to delivering individualised patient care. Using this process has made sure all our patients have well managed and planned discharges which Dementia Care Target: To reduce the use of inappropriate antipsychotic medication (causing excess sedation) in patients in our care and involvement of carers. What we achieved: 80% had medication reviewed, 89% had a carer identified, 87% documented discussion with carer recorded, and reduction achieved for a small number of patients. What Next: More work is planned to further reduce these medicines in partnership with consultants, GP’s and families. enables them to be discharged on time and not have to stay longer in hospital. Discharge Summary-launched August 2011 An electronic Discharge Summary was introduced to provide the patient’s GP with the most up-to-date information within 24 hours of discharge. The summary provides the GP with an overview of the care provided during the patient’s admission and key information such as medication changes or any after care arrangements. This is sent to the GP within 24 hours of the patient’s discharge. Admission, Discharge and Transfer Policy- launched October 2011 DCHS revised their Admission Policy to include new developments and to add emphasis to the Discharge and Transfer processes encompassing the whole patient pathway following feedback from our patients. The Admission, Discharge and Transfer policy aims to define the purpose of in-patient care at our Community Hospitals and how to access these services. This year we worked together with our consultants to reduce the use of anti psychotic medication for our dementia patients and utilise more behavioural therapeutic interventions. This work is continued on the back of the environmental work we began in 2010 for “Enhancing the Healing Environment” and completed in 2011/12 . Both Spencer ward at Buxton and Riverside ward at Newholme have completed the environmental changes we talked about in the 2012/11 Quality Account. There has been a significant reduction in medication intervention needed with the patients in our care as the nurses utilise more therapeutic measures providing significant benefits to both patients and carers (see page 47). DCHS QUALITY ACCOUNT 2011/12 29 Mortality Audit Many people especially older patients, with disability and long term conditions, fear that by being admitted to hospital they may die. Public inquiries, national reports and head line media stories have quite rightly raised concerns. Since April 2010, we have collected and analysed data on all the deaths that have occurred on the wards in our community hospitals. This allows us to know who has died, from what cause and if their care met specific standards at that time. Nationally there is a system for acute hospital Trusts called the Summary Hospital Mortality Indicator. This wasn’t designed for and doesn’t apply to our Trust but we have been committed to develop a local scheme. We are now in a position to be able to look back and compare our results over time and see whether we are improving against our own local four summary indicators. 1.The majority of deaths (>90%) in our community hospitals will be expected This means we require our staff to identify patients who are dying from a natural process (where active treatment is no longer working) 2. Almost all (>90%) of expected deaths will be on the End of Life (EoL) pathway. This pathway is a system of care (nationally designed on best practice) to offer and monitor high quality palliative care (e.g. to reduce symptoms of pain and distress) 3.Of patients expected to die 80% will have their preferred place of death recorded Many people would want to die in places they feel safe and comfortable. Best practice is to ask patients (and their families if they are unable) where this preferred place is. 4.Deaths directly attributed to adverse events Even in the best hospitals some patients can die from adverse events such as a fall or from infections. Learning lessons from public enquires means that we have a minimal tolerance to these adverse events. By auditing them we can investigate and change practice where necessary. Local Indicators What we achieved Standard 1 Expected deaths >90% Standard 2 >90% expected deaths on EOL pathway Standard 3 Preferred place recorded 80% Standard 4 Minimal tolerance of deaths from adverse events 2010-2011 2010/2011 89% 65% 55% 0% 2011/2012* Quarters 1-3 95% 80% 62% 0% Quarter 4 94% 88% 63% 0% *At the time of writing this account the full annual mortality report is being prepared and validated. We have presented the results for this year with cumulative (and averaged) first three quarters and last quarter (January- April) separately. 30 DCHS QUALITY ACCOUNT 2011/12 What we learned • Standards 1 and 4 have met or exceed our high expectations • Standards 2 and 3 show steady improvement is taking place in the number of patients appropriately placed on the end of life care pathway and in the number of patients having their preferred place of death recorded • Standard 3 Establishing the Preferred Place of death is a challenge as there is a high prevalence of dementia in these patient groups which means often the patients don’t have the mental capacity to understand and explain their preference. This year we will look into this area in more detail. This indicator might change in description and expectation. What we do with these results These are reported to the Trust Board. This system for a specialist community provider, is an innovation which most comparable Trusts currently do not do. This information together with other clinical outcome data (such as Venous Thrombo Embolic Prevention) helps us to understand whether we offer safe and effective services. This system drives and fuels wider Quality Improvement objectives to improve: • Communication between staff and patients (and their families) • Assurance that our figures remain consistent and there are no unexpected increases or decreases in expected deaths by ward (driving positive leadership through local accountability) • The numbers of patients who have their resuscitation status discussed and recorded appropriately • Determine whether any deaths have occurred as a direct result of an adverse event on our premises so investigation and learning can be achieved • Assurance that we are adhering to best practice in end of life care and providing safe and high quality end of life care to our patients • Focus staff and Trust resources into priority areas which patients and public want and need. We have set very high standards for ourselves. We feel this is very important because this time in peoples’ lives is the most stressful and our staff should aspire to the very best of care. We are very encouraged by these results and will continue to liaise with staff to maintain and improve them further, and to support them in this often challenging and sensitive area of work. Care of the Acutely Ill Patient Embedding Best Practice and Training: • The new Care of the Acutely Ill Patient (CAIP) course is informative, interactive and hands-on. It is designed to give registered nurses and in-hospital health care assistants the essential skills and knowledge they need to recognise and manage a deteriorating patient whilst waiting for help. • Patient Safety Monitoring and Reporting • By using robust and reliable early warning systems and standard ways of communicating concerns about a patient that is deteriorating we are treating our patients more effectively. DCHS QUALITY ACCOUNT 2011/12 31 Leicestershire County and Rutland Out-patient, Diagnostic and Day Surgery (LCRODDS) LCRODDS identified the need for a flexible, future proof, robust Digital Dictation workflow system to be implemented Trust-wide. The implementation of the Winscribe Digital Dictation system made sure letters were typed up rapidly to meet the 18 week target. Benefits include improvements in efficiency, visibility and management of work across sites, provided the ability to transfer dictations from author to secretary from any site and reduced typing backlogs to achieve the two week turnaround time. It also made sure prioritisation monitoring and reporting of workloads, improved and secure and instant transfer of dictations via the hospital network, with no loss of tapes or accidental deletion of dictations, has occurred. This has stopped patient data and confidentiality breaches. Hinckley and District Hospital Hinckley District Hospital has invested £445,000 in new endoscopy equipment to help with the early diagnosis and treatment of patients. The new imaging equipment is the most advanced technology available with a miniature digital camera and newly developed 32 DCHS QUALITY ACCOUNT 2011/12 wireless technology. Barrie Rathbone, Consultant Physician and Gastroenterologist, said: “Good quality imaging is a prerequisite for the diagnosis and management of digestive diseases. The state of-the-art equipment will allow high quality endoscopy facilities at Hinckley, helping to provide the best possible service for patients.” Loughborough Hospital Loughborough Hospital was presented with a new piece of equipment in 2010/11 which is helping to ensure patients are in the best possible condition to undergo their minor operations. The new Hemocue - a special device that measures haemoglobin in the blood – was presented to the hospital’s outpatients department by the Rotary Club of Loughborough Beacon. This will help us to do a simple pin prick blood test on the day when patients come in for procedures. The Hemocue, is now being used routinely as part of the pre-operative care for patients coming into the hospital’s outpatients department for day case procedures and will help to make services safer and improve patients experience. Coalville Hospital The new Phlebotomy appointment system has transformed the department making it more accessible and flexible for service users. Patients can obtain advice and information from the receptionist by telephone, particularly special requirements when needed prior to a blood test. Patients have the option of using the phone at reception or can call from home to improve efficiency and reduce waiting time. April 2011 saw the launch of the first ‘drop-in’ afternoon which allows patients to use the service at their own convenience without having to book an appointment. The phlebotomists are trained in neonatal and paediatric blood taking ensuring that the service can be used by both adults and children. The phlebotomists also have teaching certificates which enables in-house training for other NHS professionals and provides continuation of care for both inpatients and service users. Making a Difference – a focus upon children and young people. During this year we have been undertaking work to improve children and young people’s services. There is a national priority to improve services for the early years of a child’s life. This has included a focus upon integrating the provision of health care with other services such as Children’s Centres and taking a more preventative and interactive approach to service delivery. We have also increased the number of Health Visitors (specially qualified nurses with an additional public health qualification). Derbyshire is a national early implementer site for the delivery and improvement of the new National Healthy Child Programme, (which increases the interactions with families at key stages in a child’s development). As a result of this work there has been an increase the number of children we have seen at key stages of their development and in particular for those ages 3-4 months old and aged two years. Although it is too early to monitor the impact of this we have received some very positive comments from the families involved who have responded well to this increased level of service provision. We have also been part of another national development called the Family Nurse Partnership (FNP). As a result of this we have increased the number of specially trained nurses and health visitors working with young first time mothers from early pregnancy until the child’s second birthday. Although it is too early to see the benefits of the FNP we know from national evidence that improved outcomes for the children and families can be expected. This work will continue through 2012/13 and outcomes measured in accordance with national programme requirements. DCHS QUALITY ACCOUNT 2011/12 33 Sexual Health Promotion Service Following on from the successful work programme to increase the uptake in chlamydia screening in 2009/10 the sexual health promotion service undertook a new piece of work. The focus of the Well Sexy peer education outreach programme was to increase awareness of sexual health issues. This initiative targets young people primarily aged between 15 and 25 in social settings such as pubs and nightclubs, in educational settings such as schools and colleges and at other young people’s events such as music festivals. The regular sustained programme that has been delivered has involved the dissemination of targeted health promotion messages through themed campaigns, stalls and road shows, along with the distribution of free safer sex packs and signposting information. This has been conducted throughout the year with great success. They continue to be a key player in the delivery of the National Chlamydia Screening programme. Specialist Children Services Answering Awkward Questions During 2011/12 our school nursing service undertook a piece of innovative work to improve services for young people. Recent 34 DCHS QUALITY ACCOUNT 2011/12 research shows that children and young people want to talk to their parents and carers about sex and relationships. Children are surrounded by sexual images and information and they naturally will need help in understanding these issues. By answering their awkward questions from an early age, they can be given confidence to make safe and healthy choices as they grow up reducing the chance of unplanned teenage pregnancy, unhealthy relationships and other risks later in life. Following a survey which took place in Bolsover, the service identified parent concerns and as a result, can now provide help and guidance to answer children’s questions. Books are available to be borrowed from primary schools to share with a child, school nurses and teachers are able to help with questions and two specific websites feature useful advice. Further leaflets and a website forum are planned by the service for future development. Speech and Language Therapy Key achievements this year: Working with Young Offenders 2nd Annual Trust Clinical Audit Day/Raising Awareness and Skills New Trust Strategy and Policy Investment in quality and clinical audit staff in services Delivering continuous clinical quality improvements Reporting improving levels of assurance, validated by independent Auditors A service model for young offenders with speech, language and communication needs (SLCN) was developed to detect unrecognised communication difficulties. This community based model encompasses universal elements including raising staff awareness and training, advice for staff working with such service users together with specialist assessment and access to speech and language interventions. The model is to be transferred and adapted to integrate with youth offending services. The patient benefits from early recognition of and empowerment to manage their communication difficulties. It is hoped it will also lead to a reduction of mental health problems later in life by earlier detection of undiagnosed communication difficulties. This then provides enhanced opportunities to participate in educational and recreational activities. The proposed model of service is included in the Integrated Pathway for SLCN. This is a tool jointly designed in partnership with Derbyshire County Council and North Derbyshire Speech and Language Therapy Service. It is to support the commissioning of both new and continuing services to improve outcomes for children with SLCN as identified in national and local strategies. Clinical Audit Clinical audit is a service improvement tool that measures how well we are doing against a standard (e.g. NICE Guidance), helps us target improvement on the basis of these results, and then measures how well we have improved after implementing the improvement plan. As part of the Trust’s work to meet NHS Litigation Authority standards for clinical audit we have put in a lot of work to produce a new Clinical Audit Strategy and Policy. The policy sets up a mechanism for ensuring each audit is checked before it starts and then tracked to completion, including evidence of a contribution to service improvement. This will be implemented in full in 2012/13, and a system to support this is under development. The appointment of additional quality and clinical audit support staff in the Integrated Community Based Services and Health, Wellbeing & Inclusion Divisions has been a welcome development, supporting the Annual Clinical Audit Service Plans and in some instances helping clinical staff with data collection for some audits. In 2011/12 we built on the progress of 2010/11 and each service was asked to complete an Annual Plan of Clinical Audits they expected to undertake in year. The table below provides a list of audits identified to be undertaken to meet the PCT commissioners expectations, national audits we are expected to deliver, and any other audits that are of high importance. DCHS QUALITY ACCOUNT 2011/12 35 36 2011-12 Priority Programme Compliance to Standards Stroke Community Care Derbyshire CQUIN 2011/12, NICE Stroke Quality Standard Safety Express Audit Derbyshire CQUIN 2011/12, DH initiative, NHSLA Content of Care Plans Derbyshire CQUIN 2011/12 Preventing Readmission Derbyshire CQUIN 2011/12 Learning Disabilities - Access to Appointment Audit Derbyshire CQUIN 2011/12 NICE Dementia Standards Audit Derbyshire CQUIN 2011/12, NICE Dementia Standard Children’s Service - Midwifery Handover Audit Derbyshire Quality Schedule 2011/12 Learning Disability - Physical Healthcare Audit Derbyshire Quality Schedule 2011/12 Learning Disability - Dual Diagnosis Audit Derbyshire Quality Schedule 2011/12 Adult End of Life - Inpatient Pathway Audit Derbyshire Quality Schedule 2011/12 Adult End of Life - Needs and Preferences Audit Derbyshire Quality Schedule 2011/12 Antimicrobial Audit MIU and Theatres L&R Quality Schedule 2011/12, Health & Social Care Act, CQC, NHSLA Safeguarding Children and Vulnerable Adults L&R Quality Schedule 2011/12, Good Practice for Safeguarding Children and Vulnerable Adults Care and Control of Medicines Policy L&R Quality Schedule 2011/12, Care and Control of Medicines Policy in Community Hospitals Controlled Drugs L&R Quality Schedule 2011/12, Controlled Drugs Legislation Safer Surgery Programme L&R Quality Schedule 2011/12, WHO Surgical Safety Checklist Clinical Records Audit L&R Quality Schedule 2011/12 NHSLA, CQC Clinical Records Audit NHSLA, CQC C Difficile Audit Health & Social Care Act, CQC, NHSLA MRSA Audit Health & Social Care Act, CQC, NHSLA Antimicrobial Audit Community Hospitals Health & Social Care Act, CQC, NHSLA PEAT Audit Health & Social Care Act, CQC, NHSLA Treatment Card Audit Monitoring of DCHS Medicines Code, CQC, NHSLA Insulin Prescribing Audit NPSA Alert, CQC, NHSLA Pharmacy Interventions Audit DCHS Medication Safety Team (MOST), CQC, NHSLA Mortality Shipman Report, Francis Report, CQC, NHSLA Wheelchair Audit Incident WHO Safe Surgical Checklist NPSA National Falls Patient Experience Audit NCAPOP, NHSLA National Integrated Care Audit NCAPOP, NHSLA DCHS QUALITY ACCOUNT 2011/12 Please see glossary for an explanation of the multiple abbreviations used. We participated in two specific national audits this year which are relevant to our Trust – see below. Many national audits in the NCAPOP programme are not suitable for our community Trust, but in future it is expected that new national audits will include more that we will be able to participate in. Next year the Clinical Audit Team working in collaboration with the Research Team will produce a new programme of four half day training modules in basic audit, evaluation and research skills for clinical staff. Falls Exercise Programme The national feedback to providers included: • Review the provision of exercise programmes within the organisation to ensure they are evidence-based exercise for falls – we have completed this and comply to the Otago* system • Ensure staff delivering exercise programmes are appropriately trained in delivering specific evidence based exercise interventions for reducing falls in older people - all our current staff are trained • Ensure staff routinely explain to patients the benefits of exercise and why they are being referred for an exercise programme • Ensure patients are given an opportunity to express any concerns they may have about being referred and/or taking part in an exercise programme. We continue to audit these recommendations and relate them to the outcomes of the programmes and the patient experience of the service they received. National Intermediate Care Audit This national audit started in 2011/12. We have submitted our data and at the time of publication we have not received any feedback. *Note – The Otago Exercise Programme (OEP) is an individually tailored exercise programme that is delivered in the patient’s home by a trained nurse or physiotherapist. It has been shown to reduce falls by 35%. DCHS QUALITY ACCOUNT 2011/12 37 Information Governance Percentage of valid NHS Numbers and Registered GP Practice codes for DCHS data submitted to the Secondary Uses Service (SUS) in 2011/12 (April 2011 to March 2012) for inclusion in the Hospital Episode Statistics (HES). This information is sourced from the NHS Information Centre’s Data Quality Dashboard: • Admitted patient care: 100% Valid NHS Numbers and 100% Registered GP Practice codes Research and Knowledge Services In 2011/12 we welcomed the transfer of these teams into our new Trust from the PCT. They continue to provide some services to the PCT and primary care. The aims of the research strategy for DCHS supports the participation in and the effective use of research and service evaluation to provide better community health care services for the people of Derbyshire. Our Trust complies with national requirements to promote and conduct research, set goals for research within our organisation and to report on our achievement to the Board in an annual report. We present a small fraction of their work as examples of what was done: • Access to Derbyshire community hospitals and clinics • Using financial incentives for smoking cessation in pregnancy 38 DCHS QUALITY ACCOUNT 2011/12 • Outpatient care: 99.9% valid NHS Numbers and 100% valid Registered GP Practice codes • Accident & Emergency (MIU) care: 99.4% valid NHS Numbers and 100% valid Registered GP Practice codes. Information Governance Toolkit submission for 2011/12 – DCHS scored an overall percentage of 71% and received a ‘satisfactory’ (green) rating. • Financial incentives for smoking cessation in pregnancy: A pilot behaviour change intervention study • Food health needs assessment - cooking skills and food purchase by recently bereaved elderly men • Evaluation of Tier 3 Weight Reduction Service Pilot (PCT/DCHS) • Complex health and social care needs • Principles to be used in making decisions about changes in health and social care services • Evaluation of Health Promoting Workforce Project • Single Point of Access and the Chesterfield Winter Pressures Pilot • Parents of children with additional needs views of services provided by Health Visitors • Young Carers views of services provided by School Nurses. Clinical Records Target: Increase the numbers of services engaged in records audit and demonstrate improvement in the worst performing services. What we Achieved: An increase in services engaging in this audit and showed significant improvements in our worst performing areas. What next: Clinical documentation and record keeping standards remain a priority in our Trust. Root Cause Analysis into specific serious incidents showed that poor standards of record keeping were contributory factors. Our Board will be reviewing the expectations and driving further improvement in 2012/13. This is part of our commitment to get the basics right reflecting our new quality strategy. This year’s clinical records audit was conducted in September and the results show that we have maintained the improvement from last year, but have only made a further 1% improvement this year. The number of services included in the audit increased from 29 to 37 this year as planned, including several services that have not participated before, though some of these services are now reported separately where they were part of a larger group last year. The results by each of the standards are shown in the table. The Research Team also supported and evaluated the DCHS Foundation Trust public consultation. This report to the Board helped the Trust listen to and really understand the expectations of local people and partner organisations. Comparison of Clinical Records Audit Results by Standard for 2010 and 2011 DCHS QUALITY ACCOUNT 2011/12 39 Evidence of improvements for patient experience 40 DCHS QUALITY ACCOUNT 2011/12 Evidence of improvements for patient experience The experience of our patients, relatives and carers who use our services in Derbyshire and Leicestershire and Rutland is of paramount importance. focus us upon placing our patients at the centre of everything we do and enabling us to make a difference together. Patient and Public Involvement (PPI) We understand the value, the benefits and positive outcomes, both financial and non financial, of involving patients and public in the planning and development of our health services. Target: Increase our patient and public involvement activity involving our PPI champions across the organisation further embedding PPI into our infrastructure. During 2011/12 our relationship with Local Involvement Networks (LINks) and the Improvement and Scrutiny Committee (ISC) has strengthened. We have also reviewed our internal systems and how we engage with our public and patients. Extend our engagement and involvement with the public in all we undertake. Our aim is to build upon this as the health system changes and as new organisations and structures emerge such as Healthwatch, Clinical Commissioning Organisations etc. Working with our commissioners, partners and our public will be key, especially as DCHS becomes a Community Foundation Trust and we will be held to account by our Council of Governors as well as our local populations. We have identified that our work in relation to patient engagement and involvement needs to take on a whole new dimension over the coming year. In order to do this we have developed a Patient Experience and Involvement Strategy. The aim of this is to What we achieved: 45 champions identified and we provided a range of evidence to our commissioners about the improvements. Examples of this include work in relation to improving nutrition and hydration for our patients, focus groups in relation to specific service changes, the development of patient diaries within our diagnostic and treatment centre, initiatives in relation to dignity and an increase in service users and carers being involved in service changes. What next: During 2012/13 we will implement our Patient Experience and Involvement Strategy with a clear focus upon delivering the ‘Patient Revolution’ and implementation of the “Family and Friends Test.” DCHS QUALITY ACCOUNT 2011/12 41 Privacy and Dignity Target: To ensure that from being admitted to hospital, right through treatment, going home or transferring to other care services there are the same standards in place - with good outcomes and positive experiences. What we achieved: Throughout DCHS staff continue to undertake the Essence of Care benchmark on Privacy and Dignity and Communication. We have achieved good standards in compliance and we have received positive feedback form our patients. We have also ‘signed up’ as a partner in a joint initiative with Derbyshire County Council’s Adult Care Service and Chesterfield Royal Hospital to work together to help ensure services deliver even better outcomes for vulnerable local people of all ages by using the Dignity in Care standards. What next: Privacy and Dignity remains a high priority for DCHS. The hospital wards within DCHS are now working towards the bronze award for Dignity and Respect Challenge. This is in conjunction with other Derbyshire Agencies and is to align ourselves with our social care providers who have been undertaking this work as a bench mark of good practice. This work will be completed during 2012/13 to meet the wider social /health care best practice benchmarking for CQC. 42 is not the best place for them or in agreeing packages of care to support this where the patient so desires. • The 3 Derbyshire care organisations believe that by focussing the attention of all staff onto the Dignity in Care standards they will be able to strengthen joint working and further improve the experience local people have when being admitted to or discharged from hospital. The joint programme will begin with development work involving Derbyshire Adult Care community social work teams working together with: • Chesterfield Royal Hospital wards • DCHS Admission, Discharge and Transfer team and Spire and Derwent Wards at Walton Hospital. The programme will be extended to include all DCHS Community Hospital ward teams. The aim is that all relevant teams will achieve the bronze, silver and gold Dignity in Care standard for their joint services through an independent evaluation. Dignity in Care Campaign-Raising the Standard Dignity Action Day was the 1 February 2012. All the wards within DCHS participated to celebrate the day with their patients. Events organised included musical events, film shows, display of major events celebrated since the Queen’s Coronation, displays around dignity and nutrition, war time posters, Pat dogs, manicures and pamper sessions, tea parties and education groups around falls. Hotel services provided a lunch to patients with a 40’s theme which was also available in all hospital restaurants. In November Derbyshire launched its joint DCHS, Chesterfield Royal Hospital (CRHFT) and Derbyshire Adult Care initiative to help their services deliver even better outcomes for local people. The campaign focuses particularly on improvements to the way hospital and community health teams work together with adult social care teams, to plan for discharge and care after their time in hospital. Part of this work involves helping patients to understand when returning home By supporting Dignity Action Day the staff : • Raised awareness of the importance of Dignity in Care • Provided someone with an extra special day • Reminded society that everyone has a role to play in respecting the dignity of those in your community • Were part of a national celebration and demonstrate solidarity for Dignity in Care. Web link: www.dignityincare.org.uk DCHS QUALITY ACCOUNT 2011/12 Patient Experience Target: To improve the patient experience evidence base and demonstrate positive change in light of action taken from feedback. What we achieved: A systematic approach to undertaking a patient questionnaire across our services. Development of service plans in order to act upon patient feedback. What Next: A comprehensive action plan has been developed to support the delivery our Patient Experience and Involvement Strategy. We will strengthen our processes to evidence the impact upon how we deliver services form our patient and service user feedback. The patient feedback questionnaire has been cascaded to all services and departments. Questions cover issues such as Communication, Privacy and Dignity, Cleanliness and Nutrition with an overall question about rating of care received. As we are such a large organisation a service level approach was taken. Planned Care Services were the first service groups targeted. This covers Physiotherapy, Podiatry and Occupational Therapy. Their results show that 96% of patients would recommend the services to others and 79% rated the level of care as Excellent. Action plans of these findings are displayed in the service departments and wards entitled “You said We did.” These results are reported to our commissioners as part of our Quality Assurance scheme. We will continue to analyse and act upon service change plans during 2012/13. During the year we enhanced this approach with a short postcard size questionnaire within our minor injuries units which asked what we did well, what we could do better and if there were any additional comments. This form of feedback provided immediate feedback from patients and resulted in faster changes within the service area. We have responded by enhancing the skills of our MIU nurses with a paediatric competency training programme, improved our triaging process allowing us to better allocate the staff to the patients and improved our way of keeping patients informed of waiting times. Following these changes we have seen a reduction in our complaints relating to children, sexual health emergency care and wait times. DCHS QUALITY ACCOUNT 2011/12 43 Carers Target: Supporting carers and ensuring their voices are heard, and their opinions sought and acted upon. What we achieved: A Carer champion has been identified for each ward, to support carers when they attend the ward and ensure they register with their GP as a carer. DCHS has worked with the voluntary sector Derbyshire Links to produce a patient / carer questionnaire for use across all our hospital sites. What next: Implementing action plans in order to address areas for improvement across our inpatient sites. Joint working was undertaken to ensure carers recognise the need to register with their GP as a carer. Carers are issued with the leaflet “Do you care for someone” when appropriate as they visit the wards. Evidence fed back to us from our commissioners is that there has been a significant rise in the numbers of carers now registered. Work was undertaken to establish a carers group within community hospitals for education on falls prevention once patients returned home. The feedback from this project was that it raised understanding of what they can do to help reduce falls in their own home and encourage mobility safely. 44 DCHS QUALITY ACCOUNT 2011/12 Riverside Ward at Newholme Hospital now hold a weekly carers forum on the ward. This supports carers (of current and previous patients), providing advice and information in recognition of the important role that carers have and the need for ongoing support. Listening and Learning through complaints In 2011/12 we received 6,300 compliments and 441 complaints of which 221 required further investigation. This is compared with 418 complaints received in 2010/11. This shows no increase when the new activity from the services hosted on behalf of Leicestershire and Rutland PCT is accounted for. As a result of the feedback we have received through our complaints process we have made a number of changes. Examples include improving our operational processes when patients transfer from DCHS to other hospitals, inviting patients and their relatives to share their experiences with the staff involved in order to help staff understand what it felt like from a patient or relatives perspective, and sharing patient stories (both positive and negative) within services and at our Quality Services Committee and Board meetings. We have also undertaken focused work with our reception staff to develop standards of care. As a result of our work in relation to Safety Express we have made changes to the ward environment such as smaller water jugs and in infection prevention and control we have improved the information for patients who need to be nursed separately to other patients due to an infection. Nutrition and Hydration PEAT (Patient Environment Action Team) is self assessed annually and the scores demonstrate how well individual healthcare providers believe they are performing in key areas including food, cleanliness, infection control and patient environment (including bathroom areas, décor, lighting, floors and patient areas). Our patients can expect “excellent” food and a high standard of privacy and dignity when receiving treatment across all of our community hospitals according to the latest PEAT Assessments 2011. SITE NAME Ash Green Babington Hospital Bolsover Hospital Buxton Hospital Cavendish Hospital Clay Cross Hospital Heanor Memorial Hospital Ilkeston Community Hospital Newholme Hospital Ripley Hospital St Oswald’s Hospital Whitworth Hospital Walton Hospital Sites are each given scores from one (unacceptable) to five (excellent) and the assessments are carried out by our Matrons, Locality Managers, Infection Prevention & Control Nurses and representatives from the Estates Department. Patient and Public Involvement (PPI) representatives are also part of this assessment process. The National Patient Safety Agency confirmed our results. We scored excellent on all sites for food as part of PEAT assessment. FOOD SCORE 2010 Excellent Excellent Excellent Excellent Excellent Excellent Excellent Excellent Excellent Audit cancelled ward closed Excellent Excellent Excellent FOOD SCORE 2011 Excellent Excellent Excellent Excellent Excellent Excellent Excellent Excellent Excellent Excellent Excellent Excellent Excellent These scores are displayed on all our hospital sites for the public to see the outcome of the assessment. DCHS QUALITY ACCOUNT 2011/12 45 Supporting our End of Life patients and families Our organisation remains committed to providing quality End of Life Care to patients and their families. To clarify “End of Life Care” is identified as being the last year of a person’s life and is inclusive of all patients with any disease. In February of this year DCHS held its first End of Life Care Conference. Over 250 staff came together from different organisations to discuss and highlight the achievements made so far and identify future needs to continue to “transform” and improve the End of Life Care that patients and families receive. Following on from the very successful DCHS End of Life Conference there was the Excellence in End of Life Care Awards. This attracted nominations from within our organisation and ones we work in partnership to. The joint winners of the award gave excellent examples of individuals and teams “going the extra mile” to give the best possible care and choice to patients and their families. Throughout 2011 we have looked at improving our communication and information and to further support this a new End of Life website has been created that professionals and the public can access through our DCHS webpage. 46 DCHS QUALITY ACCOUNT 2011/12 We continue to keep our staff trained and updated through a wide range of training opportunities. This year has seen some staff appointed as End of Life Care “Champions” who act as ambassadors to promote best practice within their individual areas. We are, and will remain committed to delivering the best possible End of Life Care experience to the people of Derbyshire. Older People Mental Health (OPMH) initiatives Addressing Spirituality (Riverside) Art Work Working in partnership with the local clergy who attend the ward at Newholme Hospital, the team have embarked upon significant work in addressing and meeting the spiritual needs of the patients in their care. This has been recognised and applauded and as a result the team were asked to give a presentation to the Diocesan Conference in Derby this year. They have received very positive feedback on the attention and care they have taken in meeting the spiritual needs of our OPMH patients. This has further informed the clergy of how our teams are considerate of faith to our patients approaching end of life while their links to every day life are disappearing. Tea Party Riverside ward at Newholme Hospital is one of our OPMH wards. The team have already undertaken national recognised changes to the environment and care approaches to the patients as we reported in last year’s quality account. Following on from this they continue to be very innovative in their approaches to enhancing the care and outcomes for the patients during their stay. They have introduced a café once a week with tea and cakes much as we would all remember from our younger days that have promoted increased conversations with their families and carers providing purpose and enjoyment to the time they spend together while in our care. Improving the patient environment Enhancing the Healing environment is a national initiative which focuses upon the therapeutic benefits gained from improving the environments in which we care for our patients. The approach involves ward staff, patients and relatives (supported by the Trust Board and other services) identifying how the clinical areas may be improved to deliver direct benefits to the well-being of patients. As part of this programme we were able to open a safe outdoor area on our older peoples mental health ward (Spencer Ward) in Buxton and redesigned patient areas on Riverside ward at Newholme Hospital. Early indications are that there has been a positive impact upon how patients are reacting with less falls and increased opportunities for focused therapeutic healing. Learning from this work has been shared with others on a national basis. Ilkeston Hospital - sensory garden A newly created courtyard and sensory garden at Ilkeston Community Hospital providing a peaceful haven for elderly patients has been opened by the Lord Lieutenant of Derbyshire, William Tucker. The courtyard and sensory garden has transformed a previously nondescript and unused concrete area into a calm and colourful purpose designed space, with features such as raised flower-beds, easy wheelchair access, handrails and even surfaces underfoot, so patients with reduced mobility can enjoy it safely. The transformation has been completed with more than £11,000 funding support from the hospital’s League of Friends and with help from students from Broomfield Hall, part of Derby College, to carry out the planting. Patient Leaflet – Planning Your Discharge From Hospital - launched December 2011 Working closely with our partnership organisations including Derbyshire Adult Care, Derby City Adult Care, Chesterfield Royal and Royal Derby Hospitals we have jointly developed a leaflet for Patients and their Families, “Planning Your Discharge from Hospital.” The leaflet briefly explains what patient’s can expect if they are admitted to hospital including the support they will receive to plan their discharge. This has helped us work more closely with patients, their carers, and their families, in patients understanding what will happen and planning early for discharge, which helps to reduce readmissions and reduce complaints about lack of information. DCHS will continue to support patients to receive the right care, in the right place, at the right time. Quality Focus – Changing the Way we Identify Occupational Therapy Outcomes The Specialist Neurology Occupational Therapy Service promotes or restores independence in meaningful occupation by addressing motor, cognitive and perceptual dysfunction, as well as participation in meaningful life roles and tasks. The Occupational Therapy role in rehabilitation is well recognised and documented in national strategy and frameworks for stroke and longterm neurological conditions. The benefits of this intervention are vast but are based within the terms – enablement, independence and quality of life. The focus is to help people live their lives with their condition and not just exist with it, bearing in mind that no two patients will have the same view about what is important and of value to their life. We find a way to show what really matters to a patient and improve their quality of life without necessarily seeing major improvements in their condition. DCHS QUALITY ACCOUNT 2011/12 47 WHAT OTHERS SAY ABOUT US Care Quality Commission (CQC) update for Quality Account 2011/12 National Health Service Litigation Authority (NHSLA) DCHS NHS Trust successfully achieved registration, without conditions, with the Care Quality Commission in April 2011. The organisation is now registered to provide the following regulated activities; • Treatment of disease, disorder or injury • Assessment or medical treatment for persons detained under the 1983 Mental Health Act • Surgical Procedures • Diagnostic and Screening procedures • Transport services • Nursing care • Termination of pregnancies. DCHS were assessed against the NHSLA Level 1 Risk Management Standards on 22nd February 2012, and successfully passed the assessment achieving a score of 50 out of 50 for the documentation. These regulated activities are undertaken at 22 locations across Derbyshire and Leicestershire including both hospitals based and community based services. Following our internal investigations into a complaint if a complainant remains unsatisfied with the outcome and wishes to take the issue further, it is referred to the ombudsman for an independent review. The Care Quality Commission is the independent regulatory body for health and social care in England. The role of the CQC is to ensure that care provided by hospitals, dentists, ambulances, care home and services in people’s own homes and elsewhere meets government standards of quality and safety. CQC inspectors make unannounced visits, to ensure that they see the hospital as a patient or visitor would see it. They focus on certain areas of practice to form a ‘snap shot’ of the trusts activities related to certain areas of care. 48 DCHS QUALITY ACCOUNT 2011/12 The organisation will now be working towards Level 2 of the NHSLA Risk Management Standards which means collecting twelve months worth of evidence for the processes of the 50 policies assessed at Level 1. The evidence collection process will cover the wide range of services that are provided by DCHS. Health Ombudsman outcomes in 2011/12 12 cases went to the Ombudsman for resolution. Of the 12 cases referred only one was upheld and following this a satisfactory remuneration was agreed and paid promptly. As this was our first year operating as an NHS Trust we have no comparative data for the previous year, this data is positive in comparison to other NHS provider organisations. Coroner’s Inquests During 2011/12, eight Coroner’s Inquests were held and concluded. There were no Rule 43 letters for the Trust as a result of the above Inquests. (Rule 43 of the Coroner’s Rules allows for a Coroner to report, to the appropriate agency, circumstances in which further deaths could occur if remedial action is not taken). Never Events further improve clinical record keeping. One serious incident where there was an increased incident of Clostridium Difficile infection (3 cases) on one ward highlighted the importance of strengthening and maintaining clinical leadership and professional standards. The learning from these incidents are captured in service improvement action plans and are monitored. Patients/carers – “I always chose to go to Ilkeston hospital if it’s an option. I like the convenience to where I live, and the generous parking bays for disabled patients. It is a high incentive for me to use my local hospital especially when I can see the same consultant” The NHS has a published list of clinical errors called Never Events. These are very serious errors that should not happen. “My GP used the choose and book system with me he printed the details and I booked it myself at home which really worked for me very efficient” Our Trust has never had a Never Event. “I have been to the local hospital before and had a good experience as it is local it is very convenient and I could fit it in with my work pattern” Serious Incidents Patient Safety is a priority for DCHS, however it is important to ensure that effective systems are in place for reporting, monitoring, investigating and improving following any incident. Data is recorded and reported by the National Patient Safety Agency and is based upon the rate of incident per 1,000 bed days (comparative data against 19 other primary care organisation with inpatient provision) (March 2012 report). When compared with the above organisations DCHS is within the middle 50% of reporters with a reporting rate of 32.5% against a median of 30.8%. Data for DCHS (1/4/11 – 30/9/11) shows that our rate of Serious Incidents which have resulted in severe harm or death is 0.4% against a rate of 0.7% in comparative organisations. Our Trust governance structure supports a systematic analysis and learning from serious incidents. Two serious incidents relating to pressure ulceration and a serious case review identified that there is a need to “All the staff were courteous and polite at all times explaining everything as they went along” “The hospital was the cleanest I have ever been in and smelt like a hospital should do” Response to the patient reference group“May I compliment DCHS from reception to nurses and specialist , the service was faultless and I can compare this to other hospitals I have been patients at and can clearly state that this was the best experience by far.” What our Staff say As part of the national staff survey our staff are asked the ‘net promoter’ question – i.e. whether they would recommend our services to family or friends. This is seen as one of the indicators of the quality of service provided. Our results for 2011/12 showed us that 76.5% of our staff either agreed or strongly agreed with this statement compared to 59% (average amongst other trusts working with the Picker Institute who collate this information). DCHS QUALITY ACCOUNT 2011/12 49 DECLARATION AND STATEMENTS Derbyshire County Council Improvement and Scrutiny Committee-People Comment on Derbyshire Community Health Services NHS Trust Quality Account 2011/12 The Improvement and Scrutiny Committee welcomes the opportunity to comment on Derbyshire Community Health Services’ (the Trust) Quality Account for 2011/12. The Committee has undertaken some work with the Trust during the reporting period, most notably around securing improvements for patients and the public on the issue of nutrition and hydration. The Committee, in its involvement with the Trust, have been impressed by the quality of services it provides and its enthusiasm and commitment to securing further quality improvements that will benefit patients, staff, and the service as a whole. The Committee look forward to seeing progress against the areas for improvement identified by the Trust for this year. Cllr Gill Farrington Chair Improvement & Scrutiny Young People Derbyshire LINk response to Derbyshire Community Health Services Quality Accounts 2011/12 Derbyshire Community Health Services (DCHS) NHS Trust has produced a comprehensive document and what is encouraging to Derbyshire LINk is that success and failure (sometimes by a narrow margin) is recognised equally and is seen as part of the priorities for improvement in 2012/13. Through our own engagement activities, comments collated regarding the services provided by DCHS are fed back through their involvement as a Derbyshire LINk Stakeholder. These comments are provided by way of a formal and confidential report, on a bi-monthly basis. It is interesting to read of the emphasis given to Infection Prevention and Control, through the Champions initiative along with the Safety Express and the Named Nurses for Safeguarding Adults. DCHS are receptive towards receiving this intelligence, which is gained independently from the Derbyshire public, and is considered by DCHS in the planning, development and delivery of their services. Discharge planning is an important aspect of patient care and one that Derbyshire LINk has extensively investigated and reported on. DCHS clearly have recognised this as an area for development and clearly demonstrate their ongoing commitment to improving patient experience. DCHS undoubtedly are responsible for delivering a wide variety of health services and Derbyshire LINk is pleased to have developed an open communication channel with them in order that the patients’ voice is heard. The Speech and Language service model, especially with young offenders, is constructive. We are sometimes not aware that we speak a different ‘language’ to young people especially where restricted language codes are involved. Of particular interest to Derbyshire LINk are the examples of Patient and Public Involvement (PPI) work that DCHS have undertaken. 50 DCHS QUALITY ACCOUNT 2011/12 Internal and external views sought as part of consultation process Front line care council (FLCC) this is our staff group from across all our services who act as a consultation and listening group. They were part of the consultation process for the writing and production of this document. The views of our Readers panel were sought through our PPI team as part of the consultation process along with some independent readers who are part of our LAY representatives. Commissioners General Comments North Derbyshire Clinical Commissioning Group (CCG) is the lead commissioner for Derbyshire Community Health Services NHS Trust (DCHS). The CCG is responsible for commissioning the services from this provider for NHS Derbyshire County and NHS Derby City. The CCG believes that Derbyshire Community Health Services NHS Trust has produced a comprehensive quality account which broadly reflects the information received by NHS Derbyshire County through its contract monitoring arrangements. Measuring & Improving Performance The CCG has well-established mechanisms in place for checking service quality as part of its contract monitoring arrangements. The CCG has agreed with DCHS to monitor quality in a wide range of areas, most of which are detailed in this quality account. As stated within the account a number of quality measures that attract an incentive payment were agreed for the year 2011/12 covering areas such as stroke care, dementia care, falls, reducing pressure ulcers, breastfeeding sustainment rates, care plans and patient experience. All of these schemes relating to the incentive payments are detailed in the account. Through review of the Trust performance in these areas the CCG noted whilst some of the CQUIN targets had not been achieved significant progress in relation to the improvement of the quality of services provided had been made. It is noteworthy that DCHS is committed to sustained improvement in the quality of the services they deliver. Evidence of this statement is shown within the strengthened clinical governance processes and structures which have been implemented within DCHS during 2011/12, alongside the nationally recognised work in relation to quality improvements and innovation such as Safety Express, HSJ award for Care Homes Support Team and regional recognition for the Infection Prevention and control team. delivers to patients. This has ensured that no patient is placed on a ward with mixed sex accommodation and facilities and signage has been improved. Additional Comments Quality Accounts are intended to help the general public understand how their local health services are performing and with that in mind they should be written in plain English. DCHS have produced a comprehensive, well written Quality Account. It is easy to read and is visually appealing. The Quality Account demonstrates a high level of commitment to quality in the broadest sense and is commended. Statement from NHS Leicester, Leicestershire County and Rutland The Derbyshire Community Health Services Quality Account provides information covering all areas of quality and reflects the work implemented to improve care through the CQUIN and quality indicators. We support their objectives for improving quality for 201213 and would suggest that future Quality Accounts are more outcome focused. Caroline Trevithick Chief Nurse and Quality Lead West Leicestershire CCG Carmel O’Brien Chief Nurse and Quality Officer East Leicestershire and Rutland CCG The other area for which DCHS requires praise is in the focus it has placed on improving the environment of the services it DCHS QUALITY ACCOUNT 2011/12 51 GLOSSARY 52 Abbreviation or term What it stands for What it means A4C Agenda for Change The national framework that determines pay and terms and conditions for NHS staff A&E Accident and Emergency Hospital departments that assess and treat people with serious injuries and those in need of emergency treatment Acute Care Specific care for diseases or illnesses that progress quickly, feature severe symptoms and have a brief duration AGM Annual General Meeting This is a public meeting were we present our performance over the year AHP Allied Health Professional A term used to describe a range of clinical professions (not doctors or nurses) such as physiotherapists, podiatrists, pharmacists etc. APO Autonomous Provider Organisation The term used to describe the provider arm of a PCT which is still legally part of the PCT but is managed as a separate ‘business unit’ BMA British Medical Association Professional association that represents UK doctors and acts as an independent trade union, scientific and educational body, and publisher BME Black and Minority Ethnic This is a recognised description of people from different racial and other minority groups Caldicott Guardians Senior staff in the NHS and Social Services appointed to protect patient information CAF Common Assessment Framework A multi-agency assessment tool used to identify and support children with additional needs C.difficile Clostridium Difficile A healthcare associated intestinal infection that mostly affects elderly patients with other underlying diseases CFT Community Foundation Trust This is a community trust that has been accepted by Monitor to become a Foundation Trust CMO Chief Medical Officer The Government’s principal medical adviser and the professional head of all medical staff in England CNO Chief Nursing Officer Responsible for delivering the Government’s strategy for nursing, and leading all of England’s nurses, midwives, health visitors and allied health professionals Community Matrons Case managers with advanced clinical skills and expertise in dealing with patients with complex long term conditions and high intensity needs DCHS QUALITY ACCOUNT 2011/12 Abbreviation or term What it stands for What it means Children’s Centres Local facilities designed to help families with young children Children’s Trusts Trusts that identify what needs to be improved in a local area for children and young people, and then plan services around those needs. Chaired by Local Authority Directors of Children’s Services CQC Care Quality Commission The regulator of the quality of NHS and social care services CQUIN (scheme) Commissioning for Quality and Innovation A set of nationally and locally defined quality indicators agreed between a provider and its commissioner. Performance against the indicators is monitored through the contract and a proportion of contract income is dependent on reaching the required level of performance DCC Derbyshire County Council DCHS Derbyshire Community Health Services NHS Trust We separated from the PCT and became our own Trust on 1st April 2011 DHIS Derbyshire Health Informatics Service A shared service, hosted by DCHS from October 2009, that provides IM&T services to NHS organisations across Derbyshire DNA Did Not Attend The term used to describe an appointment or operation where the patient failed to turn-up without prior cancellation. Can be an indicator of quality issues within the service and is also an efficient issue as capacity has been wasted DNACPR Do Not Attempt CardioPulmonary Resuscitation Cardio-Pulmonary Resuscitation is the medical treatment that attempts to restart a patient’s heart and breathing DSCB Derbyshire Safeguarding Children Board The multi-agency board, chaired by the County Council, that takes overall responsibility for safeguarding and promoting the well-being of children and young people across Derbyshire DTOCs Delayed Transfer of Care A nationally defined measure of patients still in hospital who are ready to transfer home or into residential/nursing care DCHS QUALITY ACCOUNT 2011/12 53 Abbreviation or term What it stands for What it means ESR (system) Electronic Staff Record A national human resources system which is used by many NHS organisations to manage its staff records. EoL End of Life Care Care for all adult patients nearing the end of their lives EPP Expert Patient Programme Programme designed to teach good self care and self management skills to people with long-term conditions FOI Freedom of Information Act Government act which gives a general right of access to all types of recorded information held by public authorities HCAI Healthcare associated infection An infection (e.g. MRSA, Clostridium Difficile) that a patient has caught as a result of their healthcare treatment IBP Integrated Business Plan The term used by Monitor (the regulator for Foundation Trusts) to describe a 3-5 year strategy and plan for an organisation Intermediate Care Integrated services for older people that promote faster recovery from illness, prevent unnecessary hospital admissions and maximise independent living KSF Knowledge and Skills Framework The NHS KSF process involves managers working with individual members of staff to plan their training and development LAA Local Area Agreement Three year agreement that sets out the priorities for a local area in certain policy fields as agreed between government, local authority and other partners LINk Local Involvement Network Local Involvement Networks were established in England and Wales as the new, independent way for all residents to get involved in having more say in social care, medical care and mental health services in Derbyshire LMWH Low Molecular Weight Heparin Drug treatment given by injection to prevent / treat Venous Thrombo Embolic Disease LTC Long Term Conditions Conditions such as diabetes, asthma and arthritis that cannot currently be cured but whose progress can be managed and influenced by medication and other therapies MIU Minor Injury Unit A walk-in unit in a community setting that provides treatment for minor injuries and illnesses. The regulator of Foundation Trusts. Operates the Foundation Trust application and authorisation process. Monitor MRSA 54 Methicillin Resistant Staphylococcus Aureus DCHS QUALITY ACCOUNT 2011/12 Bacteria that can cause infection in a range of tissues such as wounds, ulcers, abscesses or bloodstream Abbreviation or term NCAPOP NHSLA NICE NPSA NSF OPMH PALS PPI QIPP RTT SHA SHMI SLA TCS What it stands for National Clinical Audit and Patient Outcomes Programme NHS Litigation Authority National Institute for Health and Clinical Excellence National Patient Safety Agency National Service Framework Older Peoples Mental Health Patient Advice and Liaison Services What it means This is a closely linked set of centrally-funded national clinical audit projects that collect data on compliance with evidence based standards, and provide local trusts with benchmarked reports on compliance and performance An NHS ‘insurance scheme’ that organisations buy into to manage the financial risks of litigation The organisation that reviews new drugs and technologies and either gives the NHS a mandatory ruling about what should be funded on the NHS or gives advice that is optional The body responsible for collating and sharing information about patient safety risks across the NHS A national set of defined best practice relating to a condition or group of patients that commissioners and providers should be working towards This is a specialised service which supports elderly people with mental health issues such as depression or dementia Services that provide information, advice and support to help patients, families and their carers Involving the public in shaping a care system’s development Patient and Public and keeping patients well informed of clinical processes and Involvement decisions Quality, Innovation, A new phrase/national programme to describe the priorities Productivity and that NHS organisations should be focused on Prevention The measure of how long a patient has waited from being Referral to referred by their GP to a specialist to receiving whatever Treatment Time treatment is required There is a national requirement for patients to be treated within 18 weeks of referral The ‘intermediate tier’ of the NHS that performance manages Strategic Health and coordinates NHS organisations on behalf of the Authority Department of Health There are 10 across England and we are in the East Midlands SHA Summary This is a system where health providers can demonstrate how Hospital Mortality safe and efficient their services are and describe how and Indicator when people have died Service Level The term used for non-legally enforceable ‘contracts’ between Agreement NHS organisations Transforming The national programme launched by the Department of Community Health to drive up quality and value in community services Services It consists of different strands of national policy relating to quality, innovation, commissioning and organisational forms. People with disabilities or mental conditions who are unable to Vulnerable Adults take care of themselves or protect themselves against harm or exploitation from others DCHS QUALITY ACCOUNT 2011/12 55 Derbyshire Community Health Services NHS Trust Quality Account 2011/12 56 DCHS QUALITY ACCOUNT 2011/12