Andy Layzell
advertisement

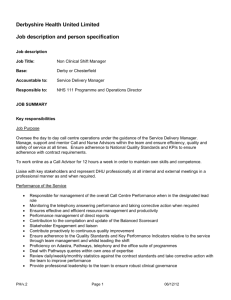
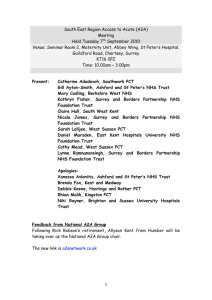
The NHS in Derbyshire in 2013 Hamster wheel or burning platform? Andy Layzell, Chief Officer Southern Derbyshire Clinical Commissioning Group Pressures in the NHS Over the last 10 years: – 50% increase in GP consultations – 35% increase in emergency care admissions – 65% increase in secondary care episodes for >75 – A&E Departments under pressure – ‘The worst winter I can remember’ What causes the pressures? Combination of factors: – Demographic change – Out-dated management of long term conditions – Poorly joined up services between primary, secondary and social care – Technical advance Long term conditions 25% of the population live with a long term condition, and account for: – 50% of all GP appointments – 70% of hospital bed days – 70% of NHS spend Quality • Quality suffers when systems are under pressure • Too many people in hospital • People not supported to retain their independence in the community • Too many people entering long term care too early or without proper assessment • Too many deaths in hospital rather than place of choice The money NHS finance increased in 2013/14 by 2.3% For the 4th year running NHS Trusts required to make 4% savings Estimated savings for Derbyshire is £250m this year Pooled budget with local authorities will be 3% of CCG allocation by 2015/16 The National Drive to Integration Integration of health and social care services for frail and elderly people and people with a long term condition, in order to: o Reduce hospitalisation o Retain independence o Reduce admissions to long term care o Improve quality o Make best use of ‘the public pound’ Integration Fund (3% of NHS funding) designed to: o Promote integration o Reduce acute expenditure A Call to Action ‘These pressures threaten the sustainability of a high-quality health service, free at the point of use’ ‘A Call to Action’ Launched by NHS England in July 2013 • Requires open dialogue with the public, providers and stakeholders about the future of the NHS • Each CCG to develop 5 year commissioning plans • To include use of the pooled budget • And explicit about impact on acute services Where is all this taking us? • Acute Trusts working more closely together in strategic partnerships • Community services working closely with primary care and social care to deliver integrated services • Primary care developed as a robust provider of a wider range of local services • Care Homes developed as strategic partners in the local health and social care economy • Mental health provision integrated with community provision • Some shift from medical to social models of care Integration in Derbyshire The Narrative “I can plan my care with people who work together to understand me and my carer(s), allow me control, and bring together services to achieve the outcomes important to me.” National Voices Progress in Derbyshire • Integrated care has developed steadily over the last two years • Different ‘brands’ to recognise differences in local circumstances, but same key principles: – – – – – – – – Joint health and social care teams linked to practices Based around populations of 20-30,000 Access to local beds Key workers/ Care Coordinators Single points of access Risk stratification Shared information In-reach to secondary care Integrated Care – where next? • • • • Starts to drive the Urgent Care agenda Starts to drive development of primary care Extend to include mental health Develop links to social capital and voluntary sector Workforce Implications • Less acute staff or more acute staff working out in the community • Integration of primary, community and social care • More tasks shared between health and social care staff • Training of Care Home staff • We need to understand a broader aim of public services • We need to be able to listen to people