Community Falls Policy
advertisement
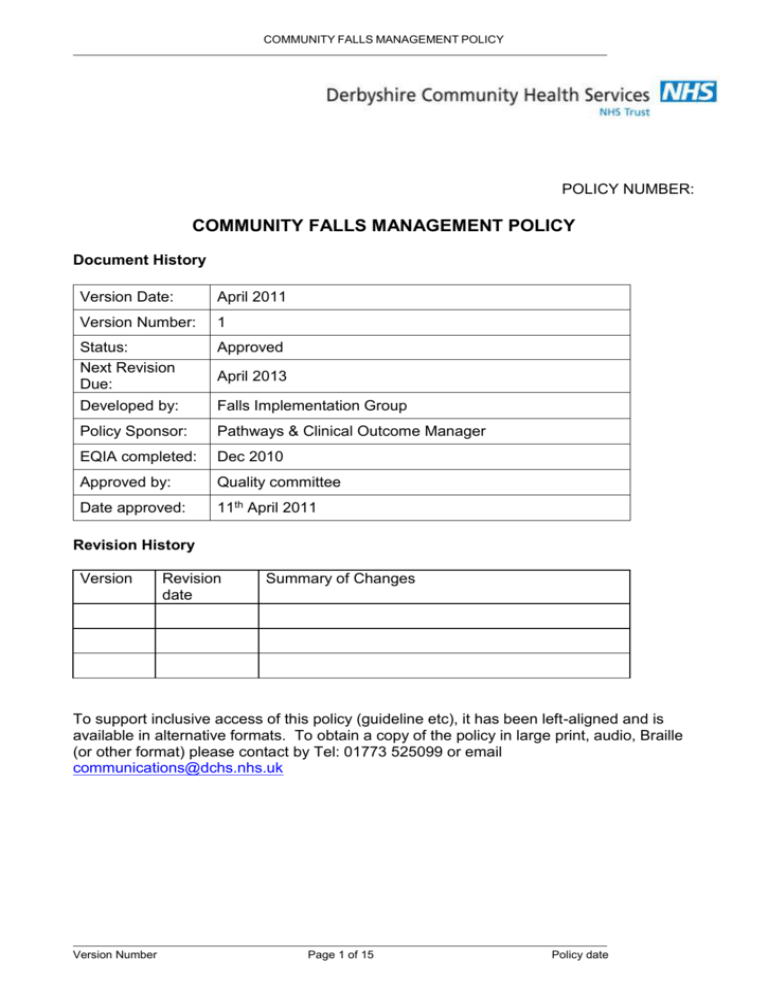
COMMUNITY FALLS MANAGEMENT POLICY POLICY NUMBER: COMMUNITY FALLS MANAGEMENT POLICY Document History Version Date: April 2011 Version Number: 1 Status: Next Revision Due: Developed by: Approved Policy Sponsor: Pathways & Clinical Outcome Manager EQIA completed: Dec 2010 Approved by: Quality committee Date approved: 11th April 2011 April 2013 Falls Implementation Group Revision History Version Revision date Summary of Changes To support inclusive access of this policy (guideline etc), it has been left-aligned and is available in alternative formats. To obtain a copy of the policy in large print, audio, Braille (or other format) please contact by Tel: 01773 525099 or email communications@dchs.nhs.uk Version Number Page 1 of 15 Policy date COMMUNITY FALLS MANAGEMENT POLICY TABLE OF CONTENTS 1. FULL DETAIL OF POLICY (INCLUDING RESULTS OF IMPACT AND RISK ASSESSMENTS) .........................................................................................................................3 1.1 Community Patients ........................................................................................................3 1.1.a 1.1.b 1.1.c 1.1.d 1.1.e 1.2 Screening ................................................................................................................3 Risk Assessment .....................................................................................................3 Treatment Plan ........................................................................................................3 Fall ..........................................................................................................................4 Onward Referral to Specialist Falls Services (Community or Day Service) ............4 Training and development for falls prevention and management ...............................5 2. References and Associated Documentation .....................................................................5 3. Appendices ..........................................................................................................................6 Appendix 1 – COMMUNITY FALLS MANAGEMENT FLOW CHART ........................................7 4. AIM .......................................................................................................................................10 5. 5.1 6. Background ........................................................................................................................10 Table - Objectives .........................................................................................................11 Area for Implementation ...................................................................................................11 7. Organisational Accountability/Responsibilities i.e. CEO, Directors, Managers, Staff ............................................................................................................................................11 8. Intended Users ...................................................................................................................12 9. Definition ............................................................................................................................12 10. Indications for Use .........................................................................................................12 11. Contra-indications .........................................................................................................12 12. Equality Impact Statement ............................................................................................13 13. Monitoring and Performance Management of the policy ...........................................13 14. Support and Additional Contacts .................................................................................14 Equality & Diversity Impact Assessment : Version Number Page 2 of 15 Level I Screening ...........................................15 Policy date COMMUNITY FALLS MANAGEMENT POLICY INPATIENT FALLS MANAGEMENT POLICY 1. FULL DETAIL OF POLICY This policy is to assist staff to reduce the risk, incidence and severity of falls by patients receiving care from Derbyshire Community Health Services, (DCHS), staff in their own homes or community settings. The policy should be read in conjunction with the policy for The Management and Prevention of Slips, Trips and Falls and the Community Bed Rail policy. 1.1 COMMUNITY PATIENTS All staff working in the community and see patients in their own homes or in outpatient settings must follow these steps. 1.1.a Screening All people over 65 years who have contact with clinical DCHS staff will be routinely screened to identify their falls risk. They will be asked if they have fallen in the past 12 months. This is the population cohort where evidence suggests maximum positive impact can be achieved. If they indicate they have experienced such a fall, additional information regarding the frequency, context and characteristics should be documented. 1.1.b Risk Assessment If screening question prompts a positive response and the additional information obtained indicates that it is appropriate to do so, a falls risk assessment must be completed see appendix 2 - Risk Assessment for the Prevention and Management of Falls in the Community by the member of staff who has asked the screening question. If assessment is ‘yes’ to four or more factors refer to specialist falls services, either in community or day services for specialist falls interventions. If assessment is less than 4 ‘yes’, the staff member who has completed the assessment should act upon any risk factors that were answered ‘yes’, that are appropriate to their scope of practice, in order to reduce the patient’s risk of further falls. Falls Prevention advice and information should be given to the patient e.g. Age UK Staying steady leaflet accessed via: http://www.ageuk.org.uk/ Onward referral to specialist falls services should be made for identified risk factors that fall outside the assessing member of staff’s scope of practice. A copy of the risk assessment and action plan will be held in the patient’s records. There should be evidence of any onward referral for medication review, specialist falls service, physiotherapy assessment, occupational therapy assessment or specialist nurse assessment. 1.1.c Treatment Plan Version Number Page 3 of 15 Policy date COMMUNITY FALLS MANAGEMENT POLICY A treatment/care plan should be generated identifying the risks and interventions agreed with the patient and be evaluated as clinically indicated see Appendix 3, Falls Risk Assessment for Older People – Community Tool – Action Plan. 1.1.d Fall If a patient falls or a fall related near miss occurs: Check the patient for signs of significant injury. If a severe injury is evident or suspected on initial assessment - dial 999 for transfer to Accident and Emergency. If the patient is assessed as having a fall without a severe injury return them to bed/chair using appropriate moving and handling technique and refer to GP. Perform baseline observation and document in patient notes and inform next of kin/ main carer. All incidents must be reported including patient details, time, location and circumstances of the falls. Reassess risk and document any actions required. If indicated initiate referral for medication review, falls service, community therapy services or specialist nurse assessment and document all interventions in the patient’s records. All incidents which have level 3 or 4 harm will be evaluated using root cause analysis by the Patient Safety Team. 1.1.e Onward Referral to Specialist Falls Services (Community or Day Service) All patients referred will receive: i. Evidence Based Multi-factorial Falls Assessment This uses the agreed standardised documentation within DCHS which is based upon the Connecting for Health Do Once and Share pathway for falls (2004). This includes the Community Falls Generic Assessment (document number 1143) for community therapy services and Staying Steady for day services (document number 0259). ii. Individualised Treatment Plan An individualised multi-factorial treatment plan will be generated and all interventions will be documented in the patient records. iii. Onward Referral An onward referral using locally agreed pathways, e.g. general practitioner, out-patient clinics for patients with an unexplained fall or request for further investigation if indicated, or for evidence based falls prevention exercise training. iv. Review Specialist falls prevention services will review case loads at agreed time intervals to monitor effectiveness of service and impact interventions. Version Number Page 4 of 15 Policy date COMMUNITY FALLS MANAGEMENT POLICY 1.2 TRAINING AND DEVELOPMENT FOR FALLS PREVENTION AND MANAGEMENT Within DCHS there will be 3 levels of training for falls prevention and management: Level 1 - ALL DCHS staff regardless of location, should have basic awareness training in relation to falls prevention and their roles and responsibilities therein. This will include an understanding of the potential causes of falls including intrinsic and extrinsic factors. All DCHS staff assessing patients, again regardless of location, will be made aware of and trained in the use of the relevant falls prevention and management tools and associated processes. They will also undertake further fall prevention and management training on areas relevant to their profession. All Level 1 staff will access the Falls Training DVD and line managers must keep a record of the staff who have undertaken this training and forward the details to the Learning Team to ensure the electronic staff record (ESR) is updated. Falls Awareness and Prevention will be included in essential training, all new staff induction and preceptorship competency frameworks. Level 2 - All services / teams /departments should have an identified ‘Falls Champion’ who will be expected to lead and ensure the process is in line with the policy and to lead the local scrutiny of monthly falls reports. Identified champions and other key clinical leaders will receive training on the falls policy, risk assessments decision algorithms. Level 3 - All staff providing a specialist falls service or performing specialist falls assessments will require evidence based training and skills updating. This training will require individuals to access ‘learning beyond registration’ funding to apply for accredited courses delivered by external providers. 2. REFERENCES AND ASSOCIATED DOCUMENTATION Department of Health (2009) Falls and Fractures: Effective interventions in health and social care. DCHS Management and Prevention of Slips, Trips and Falls Policy DCHS Record Keeping Policy DCHS Incident reporting Policy DCHS Joint Derby and Derbyshire Health & Social Care Policy for the Safe Use of Bed Rails in the Community. DCHS Policy for the Safe and Effective Use of Bed Rails within the Community Hospital Do Once Share Pathway web site accessed November 2010: http://www.connectingforhealth.nhs.uk/resources/systserv/do-onceand/?searchterm=do%20once%20and%20share Fonda D et al. (2006) Reducing serious fall related injuries in hospital. Medical Journal of Australia 184: 379-382 Version Number Page 5 of 15 Policy date COMMUNITY FALLS MANAGEMENT POLICY Haines TP et al (2004) Effectiveness of targeted falls prevention programmes in a sub acute setting. A randomised controlled trial. British Medical Journal 328: 676-679 Healey F et al. (2004) Using targeted risk factor reduction to prevent falls in older hospital inpatients A randomised controlled trial Age and Ageing 33: 390-395 Help the aged (2008) Falling Short Help the Aged London NHS Institute for Innovation and Improvement (2009) High Impact actions for Nursing and Midwifery http://www.institute.nhs.uk/images/stories/Building_Capability/HIA/NHSI%20High%20Impa ct%20Actions.pdf National Institute for Health and Clinical Excellence (2004) Falls-The assessment and prevention of falls in older people. Available at: www.nice.org.uk/guidance/CG21/guidance/pdf/English Department of Health (2001) National Service Framework for Older People Medicines and Healthcare products Regulatory Agency Device Alert 2007/001. Reporting Medical Device Adverse Incidents and Disseminating Medical Device Alerts. Available at: www.mhra.gov.uk The Patient Safety First Campaign have recently issued a ‘How to’ Guide for reducing harm from falls. http://www.patientsafetyfirst.nhs.uk/ashx/Asset.ashx?path=/Interventionsupport/FALLSHow-to%20Guide%20v4.pdf Prevention Package for Older People http://www.dh.gov.uk/en/SocialCare/Deliveringadultsocialcare/Olderpeople/Preventionpack age/index.htm http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/@pg/document s/digitalasset/dh_103152.pdf http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/@pg/document s/digitalasset/dh_103151.pdf http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/@pg/document s/digitalasset/dh_103147.pdf Royal College of Physicians (2008) National Falls and Bone Health in Older People accessible via (Accessed 9th November 09). 3. APPENDICES Appendix 1 – Community Falls Management Flowchart Appendix 2 – Risk Assessment for the Prevention and Management of Falls in the Community Appendix 3 – Falls Risk Assessment for Older People – Community Tool – Action Plan Version Number Page 6 of 15 Policy date COMMUNITY FALLS MANAGEMENT POLICY APPENDIX 1 – COMMUNITY FALLS MANAGEMENT FLOW CHART All DCHS clinical staff who work in the community or in out-patient settings should routinely ask all people aged over 65 years: 1. Have they have fallen in the past year? ‘Yes’ - Complete Falls Risk Assessment for Older People Tool. (hyperlink to) Complete action plan detailing treatment plan / onward referrals. Scored 4 or more risk factors Version Number Referral to Specialist Falls service, Community based or day services Scored less than 4 risk factors Page 7 of 15 Provide intervention to reduce risk of falls associated with identified risks. Provide advice leaflet regarding falls prevention i.e. Age UK Staying Steady Policy date COMMUNITY FALLS MANAGEMENT POLICY APPENDIX 2 RISK ASSESSMENT FOR THE PREVENTION AND MANAGEMENT OF FALLS (COMMUNITY) SURNAME NHS No ___/___/____ FORENAME ADDRESS MALE / FEMALE D.O.B HOSPITAL WARD GP/Consultant FALLS RISK ASSESSMENT FOR OLDER PEOPLE / COMMUNITY TOOL SCREENING TOOL Risk Factor Yes No 1. History of Falls Has history of 1 or more falls in past year 2. Number of Medications Takes more than 4 medications per day 3. Central Nervous System Suppressants (e.g. sleeping tablets, anti-depressants) Uses 1 or more for more than 2 weeks 4. Alcohol Intake More than 1 unit of alcohol per day 5. Postural Hypotension Dizziness on standing or sitting up 6. Nutrition Recent loss of weight, poor fluid intake 7. Vision Difficultly reading a book or newspaper, cannot recognise an object across room, recently started wearing bifocals 8. Hearing Has difficulty in hearing conversational speech 9. Footwear / Foot Care Difficulty with foot care affecting mobility, inappropriate footwear 10. Balance Needs to hold onto furniture, requires walking aid 11. Transfers Lack of control when moving between surfaces, e.g. bed to chair 12. Walking Unsteady on feet, shuffles or takes uneven steps, housebound 13. Environmental Hazards Cluttered, slip or trip hazards 14. Reduced Confidence Fear of further falls, change in lifestyle due to falls 15. Coping Strategies Unable to get up from floor. Unable to summon help 16. Memory/Comprehension (understanding) Short-term memory or comprehension difficulties which may affect ability to follow advice given if ‘YES’ for any factor, refer to intervention/referral guide, complete action plan and issue falls leaflet. If ‘YES’ for four or more factors, refer Specialist Falls Service. Version Number Page 8 of 15 Policy date COMMUNITY FALLS MANAGEMENT POLICY APPENDIX 3 FALLS RISK ASSESSMENT FOR OLDER PEOPLE – COMMUNITY TOOL – ACTION PLAN SURNAME NHS No ___/___/____ FORENAME ADDRESS MALE / FEMALE D.O.B HOSPITAL WARD GP/Consultant FALLS RISK ASSESSMENT FOR OLDER PEOPLE / COMMUNITY TOOL ACTION PLAN (including onward referrals if appropriate) Risk Identified Action Date/Time Print Name and Sign Please refer to guidance notes available on the intranet under Community Hospitals documentation. © Copyright 2009 Quality & Integrated Governance Team, Derbyshire Community Health Services Version Number Page 9 of 15 Policy date COMMUNITY FALLS MANAGEMENT POLICY 4. AIM The aim of this Policy is to manage the risk of, reduce the incidence of, and thereby reduce the harm from older people experiencing falls whilst under the care of DCHS staff in their own homes or other community settings. The Policy provides a framework with quality standards to: identify people who have fallen and or who are at risk of falling again identify those people who have sustained a fragility fracture and provide rehabilitation to restore function and prevent further fractures assess the level of risk for those individuals that have had a fall generate, implement and evaluate appropriate treatment plans provide a specialist falls service that delivers evidence based multi-factorial assessments and targeted interventions identify the need and scope for and of a specialist falls intervention. There is an expectation that clinicians will use the framework within everyday practice within DCHS. It recognises that falls are a multi-dimensional problem which requires a partnership approach across the localities and between health, social care and voluntary organisations. DCHS will deliver a service/pathway which will be based upon evidencebased practice as stated in key national guidelines (NICE). Our services will use, as part of the framework, validated tools to support the assessment and treatment process. 5. BACKGROUND Falls represent a significant public health challenge, with incidence increasing at about 2% per annum. Increased rates of falling, and the severity of the consequences, are associated with growing older and the rising rate of falls is expected to continue as the population ages. Hip fractures remain the most serious consequence of a fall and the commonest cause of accident-related death in older people – 20% of people with hip fracture die within four months and 30% within a year (DH 2009). Approximately half of those people who were previously independent become partly dependent following a hip fracture, while one-third become totally dependent. Falls are not a consequence of old age; rather they are nearly always due to one or more underlying risk factors. Recognising and modifying these risk factors is crucial in preventing falls and injuries. . Historically, the National Service Framework (2001) gave organisations key guidance in the identification and treatment for patients who have fallen. NICE guideline CG21 “Falls: the assessment and prevention of falls in older people” was issued in 2004 to provide guidance on key areas of risk, assessment, interventions, participation and education for the health care community. The Department of Health (DH) issued the Prevention Package for Older People which builds on the National Service Framework and NICE guidance. The Falls and Fractures, effective interventions in health and social care package outlines four key objectives shown in Table 1.0 (July 2009). Version Number Page 10 of 15 Policy date COMMUNITY FALLS MANAGEMENT POLICY 5.1 TABLE - OBJECTIVES See below Table 1.0 Objectives - Effective Interventions in Health and Social Care for Falls and Fractures 1. Improve patient outcomes and improve efficiency of care after hip fractures through compliance with core standards. 2. Respond to a first fracture and prevent the second – through fracture liaison services in acute and primary care settings. 3. Early intervention to restore independence – through falls care pathways, linking acute and urgent care services to secondary prevention of further falls and injuries Prevent frailty, promote bone health and reduce accidents – through encouraging physical activity and healthy lifestyle, and reducing unnecessary environmental hazards. In order for DCHS to meet the above objective and NICE guideline, the Falls framework and quality standards will be implemented. 4. 6. AREA FOR IMPLEMENTATION All patient homes or community settings where the patient receives community nursing or therapy service from DCHS. 7. ORGANISATIONAL ACCOUNTABILITY/RESPONSIBILITIES I.E. CEO, DIRECTORS, MANAGERS, STAFF This section to set out who holds organisational accountability and responsibility for the policy. The Chief Executive holds overall accountability and is responsible for assuring that there are effective systems in place to implement the guidance. The Director of Service Delivery is the lead operational officer for Derbyshire Community Health Services and is accountable to the Managing Director. The Director of Nursing and Quality is accountable for the quality and delivery of care. Operational Managers have responsibility for managing staff groups, risk management, clinical incidents, and competency practice issues once identified. Records of attendance on training will be kept by the Trust. Patient records will be audited to monitor compliance with policy. Staff competency will be evaluated during PDR process. Professionally Registered Staff. All staff are accountable for their professional practice and hold individual responsibility to maintain their knowledge and skills in relation to falls management. It is their responsibility to identify training needs and plan to meet learning objectives identified in their PDR. Version Number Page 11 of 15 Policy date COMMUNITY FALLS MANAGEMENT POLICY The policy sponsor is David Muir, Pathways & Clinical Outcome Manager. - The Policy is developed in line with the DCHS Policy Development Framework; The Policy is disseminated to its target audience; Appropriate training is given in the use of the Policy; The Policy’s implementation is monitored and reviewed on a regular basis. 8. INTENDED USERS All staff working for DCHS in the Community or in Outpatient situations. 9. DEFINITION Fall: An event which results in a person coming to rest at a lower level. Explained Fall: We know and understand the reasons that have contributed to falls. Intrinsic: Medical, psychological and physiological reasons for falls, e.g. ●Cognition & behaviours ●Mobility and transfer skills ●Incontinence ●Medical conditions ●Medication review ●Vision/hearing ●Footwear & clothing Extrinsic: Environmental reasons for falls. Unexplained Fall: We do not understand the reasons that have contributed to falls history. To presume these are more likely to have medical factors influencing i.e. history of falls Multi-professional: Multidisciplinary approach to falls prevention involving medical, nursing and therapy assessments. 10. INDICATIONS FOR USE All patients under the care of DCHS in the Community or Outpatients settings identified as at risk. 11. CONTRA-INDICATIONS None. Version Number Page 12 of 15 Policy date COMMUNITY FALLS MANAGEMENT POLICY 12. EQUALITY IMPACT STATEMENT We welcome feedback on this policy and the way it operates. We are interested to know of any possible or actual adverse impact that this policy may have on any groups in respect of gender or marital status, race, disability, sexual orientation, religion or belief, age, deprivation or other characteristics. This Policy has been screened to determine equality relevance for the following equality groups: Race, Gender, Disability, Age, Sexual Orientation, Religion/Belief, Transgender/ Transsexual. The Policy is considered to have little or no equality relevance. The person(s) responsible for equality impact assessment for this policy is Edwina Layton. Tel: 01246 515151 13. MONITORING AND PERFORMANCE MANAGEMENT OF THE POLICY To measure compliance to the Policy an annual audit will be developed and completed. This audit will be both of process and record keeping, but also of the quality and impact of risk assessments and action plans The findings of the audits and action plans will be reported and monitored by the Falls Implementation Group, (FIG). Exceptions will be reported by FIG to the Safety Committee and to the Service Delivery Directorate’s Governance Group. The Falls Implementation Group will define, develop and implement an implementation strategy across the county. Monitoring of the Guideline will take place via Falls Implementation Group. Audit of number of clinical incidents arising from falls in the community and out-patient setting. Audit number of hip factures Audit number of admissions due to falls Analysis of data demonstrating uptake of falls training. Complaints with regard to receiving falls service. Review of Guidelines initially after two years or earlier if new national guidance is released. Version Number Page 13 of 15 Policy date COMMUNITY FALLS MANAGEMENT POLICY 14. SUPPORT AND ADDITIONAL CONTACTS Name David MUIR Sarah SPILSBURY Joanna SILLS Title Falls Implementation Group Chair Senior Physiotherapist/ Falls Lead Integrated Community Manager Adelle CLEMENTS Patient Safety Manager Peter SLOAN Older Peoples Mental Health Liaison and Practice Development nurse Occupational Therapist/Occupational Therapy Team Leader – Learning Disabilities General Manager Nancy ABBOTTS Edwina LAYTON Karen CHAPPLE Version Number Senior Physiotherapist / Falls Lead Page 14 of 15 Base Babington Hospital Long Eaton Health Centre St Oswald’s Hospital Walton Hospital Newholme Contact Number Mobile: 07766500363 Telephone: 0115 8554067 Telephone: 01335 340806 Telephone: 01246 515814, Mobile: 07824 624452 Telephone: 01629 817945 Ash Green Telephone: 01629 532317 Walton Hospital Walton Hospital Mobile: 07881850226 Telephone: 01246 515910 / Email Policy date COMMUNITY FALLS MANAGEMENT POLICY EQUALITY & DIVERSITY IMPACT ASSESSMENT : SCREENING Race Which of the following diversity profiles could suffer detriment as a result of this policy / procedure /process? Religion/Belief What is the purpose of the policy under assessment? What is the background to the policy? (e.g. in response to a statutory requirement, development of good practice, organisational review etc..) Who is intended to benefit from the proposed policy? Is there any potential for impact on non-beneficiaries? Is there up to date data on the groups/individuals on whom there may be impact? Have there been changes to the equalities profile of the above groups/individuals since the collection of the data? Does the policy influence in a positive way relations between different groups of people? LEVEL I Gender Disability Age Sexual Orientation Transgender/ ALL GROUPS Transsexual The purpose of the policy is to screen, risk assess and treat patients who are at risk of falls living in the community or hospital. The back ground of the policy is to develop benchmark good practice against national guidelines. All patients who is at risk of or fears falling. The policy is for patients that are identified as at risk of falls or who fall whilst under the care of DCHS there is no impact on non-beneficiaries. This policy will impact upon patients being treated by DCHS and the implementation of a screening, risk assessment and treatment process to support the identification of those at risk of falls. Data on patients who have fallen whilst under the care of DCHS can be obtained from Datix. No It aims to be inclusive for those who are at risk of falls. It forms part of the falls pathway from identifying to specialist assessment / treatment. It gives the opportunity for screening, risk assessment and specialist Does it promote equality of opportunity? assessment for patients within DCHS relating to falls. Does the function either eliminate or contribute to the Although policy is biased towards older people, the policy recognises there elimination of unlawful; discrimination across all equalities are other patient groups in the community who may be at risk of falls due to themes? acute or long term conditions. The policy also links closely with the bed rails and in-patient policies. Are there any concerns expressed about the policy having No the potential for adverse impact on any group/s of people? Assessment Outcomes High Level 2 assessment required by Dec 2011 Level 1 assessment – signing off date: Dec 2010 Assessment carried out by: Edwina Layton, General Manager Walton Version Number Page 15 of 15 Policy date