Microbial pathogenicity Microbial pathogenicity By
advertisement

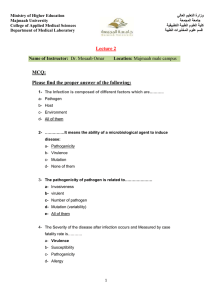
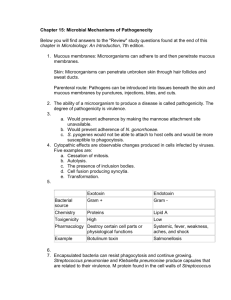
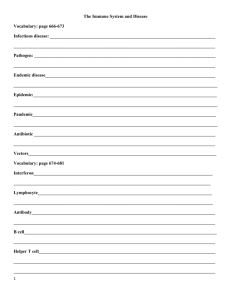
Microbial pathogenicity By Dr. Carmen Rexach Microbiology Mt San Antonio College Introduction • Pathogenicity – ability to cause disease in host • Virulence – degree of pathogenicity • Microbial pathogenesis is tug of war between virulence and pathogenicity – When microbe wins, attack of microbe overpowers host defenses – When host wins, host defenses control attack of microbe To cause disease, most pathogens: • • • • Must gain access into the host Adhere to the host tissues Penetrate or evade host defenses Damage host tissue directly or by accumulation of microbial waste products Portals of entry into host • Some organisms must enter through specific portal, others can cause disease after entry through several different portals • Skin – First line of defense – Openings in skin, hair follicles, sweat glands – dermatophytes Portals of entry into host • Mucous membrane – Respiratory tract most accessible • Have to overcome cilia, mucous, macrophage, IgA, etc. – GI tract (includes fecaloral route) • Must overcome pH in stomach, digestive enzymes – Genitourinary tract Inoculating dose • Number of organisms needed to cause disease • Depends on virulence – Very virulent, small dose may be sufficient – Less virulent, larger dose required • Nonspecific immune response takes out portion of invaders Adherence • Adhesins or ligands – Molecules on surface of pathogen – Bind to complementary surface receptors on cells of host tissues • Usually glycoproteins, lipoproteins – Located on glycocalyx or other surface structure – Example: fimbriae (pili) Penetration of host defenses • Capsules – Impair phagocytosis, but not if opsonized by antibodies – Produced by nonpathogenic bacteria to prevent dessication • Cell wall composition • Enzymes Cell wall composition • M protein of S. pyogenes – Heat resistant, acid resistant – On cell surface of fimbriae – Protective against phagocytosis • M. tuberculosis – Wax in acid-fast cells confers resistance to phagocytosis – Capable of intracellular replication in phagocytes • Common defense mechanism in some microbes Intracellular replication Enzymes • Exoenzymes = normal products to allow for absorption of necessary nutrients, also have harmful effects – Leukocidins • Destroys neutrophils and histiocytes • Produced by Staph/Strep – Hemolysins • Causes RBC lysis α,β,γ hemolysis Beta-hemolysis Enzymes • Coagulases – Coagulates fibrinogen – Forms fibrin clot = artificial capsule for bacteria – Isolated from host defenses • Bacterial kinases – Breaks down fibrin and dissolved clots – May wall off or isolate pathogen (streptokinase, staphylokinase) Streptokinase = thrombolytic Enzymes • Hyaluronidases – Dissolves hyaluronic acid (CT), encouraging disease spread • Collagenase – Breaks down collagen component of CT (muscle, organs, tissues) to encourage disease spread, such as gangrene (Clostridia) Treatment of stem cell cultures with collagenase frees colonies for removal Damage to host cells • Three methods – Direct damage to cells in close proximity • Not as common • May induce phagocytosis by host epithelial cells • May penetrate by secretion of enzymes destroying host cells – Production of toxins transported through blood and lymph • Poisonous substances produced by some microbes • Results in most associated pathology • Two types: exotoxins and endotoxins – Inducing hypersensitivity reaction Exotoxins • Proteins produced primarily in grampositive bacteria released into surrounding medium • Coded by genes in plasmids or phages infecting host bacteria – Some bacteria must be infected by bacteriophage to produce toxin • Can be very toxic Mechanisms & types of exoenyzmes • Mechanisms – Destroys part of host cell or inhibit metabolic function • Types – Cytotoxins • Kills cells or affects function – Neurotoxins • Interferes with nerve impulse transmission – Enterotoxins • Affect cells lining GI tract Protection against exoenzymes • Antitoxins = antibodies • Toxoids = chemically or physically inactivated toxins which can still stimulate immune response – Used as vaccines Exotoxin producing organisms • Corynebacterium diphtheriae – Diphtheria toxin – Must be infected by lysogenic phage containing tox gene – Cytotoxin inhibits protein synthesis in eukaryotic cells • Streptococcus pyogenes – Produces three types of erythrogenic toxins (cytotoxins) – Damage surface blood capillaries (red skin rash, scarlet fever) Exotoxin producing organisms • Clostridium botulinum – Botulinum toxin=neurotoxin produced when endospores germinate – Released when cell lyses – Inhibits release of ACh = flaccid paralysis • Vibrio cholerae – Cholera enterotoxin – Cause epithelial cells lining gi tract to produce large amounts fluids, electrolytes = interferes with muscular contraction, severe diarrhea, vomiting Scarlet fever Endotoxins • Part of outer portion of cell wall of gramnegative bacteria – Lipid A • Endotoxin (lipopolysaccharide) • No problem until cell lyses – Can occur due to exposure to antibiotics = worsening symptoms • Defenses – No effective antibodies produced Clinical signs and symptoms • Fever – Pyrogenic response – Lipid A induces release of IL-1 from macrophage – Carried to hypothalamus, induces prostaglandin release, increases temperature set point • Septic shock – Gram negative bacteria phagocytosed by macrophage – Releases TNF with following effects • Increase capillary permeability resulting in fluid loss, decrease in blood pressure • In CSF, causes release of both IL-1 and TNF, increases permeability of blood brain barrier Endotoxin producing organsims • Salmonella typhi – Typhoid fever • Proteus spp – UTI • Neisseria meningitidis – Meningococcal meningitis Mechanism of action of bacterial toxins Viruses • Host defense evasion – Intracellular reproduction eliminates exposure to immune system – Formation of syncytia • Avoids exposure to ECF and immune system – Direct invasion of immune effector cells • HIV invades cells of immune system • Reproduce in cells, and destroy cells when virus is released = immunocompromise CPE: animal cells invaded by virus • Three sources of damage – Accumulation of large #’s of viruses cause cell death – Production of viral proteins effect permeability of plasma membrane – Inhibition of host DNA, RNA, or protein synthesis CPE Human erythroleukemia cells with virus infection 1. HSV-1 2. CMV Cytocidal vs. noncytocidal effects • Cytocidal – Disruption of macromolecular synthesis in host cells • Lysosomes – Released in cells invaded by cytocidal viruses • Inclusion bodies – Negri bodies • Formation of syncytia • May cause no changes in infected cell – Changes in host cell function • Interferon production • Host antibody response to viral protein • Transform host cells – Loss of contact inhibition Pathogenicity in Fungi • No well defined virulence factors – Capsules – toxic metabolic byproducts – allergic response • Aflatoxin – Produced by Aspergillus flavus in peanuts and peanut butter – Carcinogenic properties • Poisonous mushrooms Citreoviridine • Toxin isolated from Penicillium citreonigrun + Aspergillus terreus • Inhibits absorption of Vitamin B1 (thiamine) – Beri-Beri – Affects muscles, heart, nervous and digestive systems – Seen in US only in alcoholics and rarely in gastric bypass patients • First report in Dec 2007 from Brazil due to P. citreonigrun contamination of rice, previously only in Asia – 550 cases with 42 deaths Pathogenicity of protozoa and helminths • Protozoa – Presence of protozoa and waste products – Giardia & Trypanosoma able to change surface coat structure to evade immune system • Helminths – Presence of organisms damages cells and organs structurally resulting in symptoms Pathogenicity of algae • Neurotoxin produced by few species • Saxitoxins – – – – Produced by dinoflagellates Ingested by mollusks Symptoms of botulism Red tide